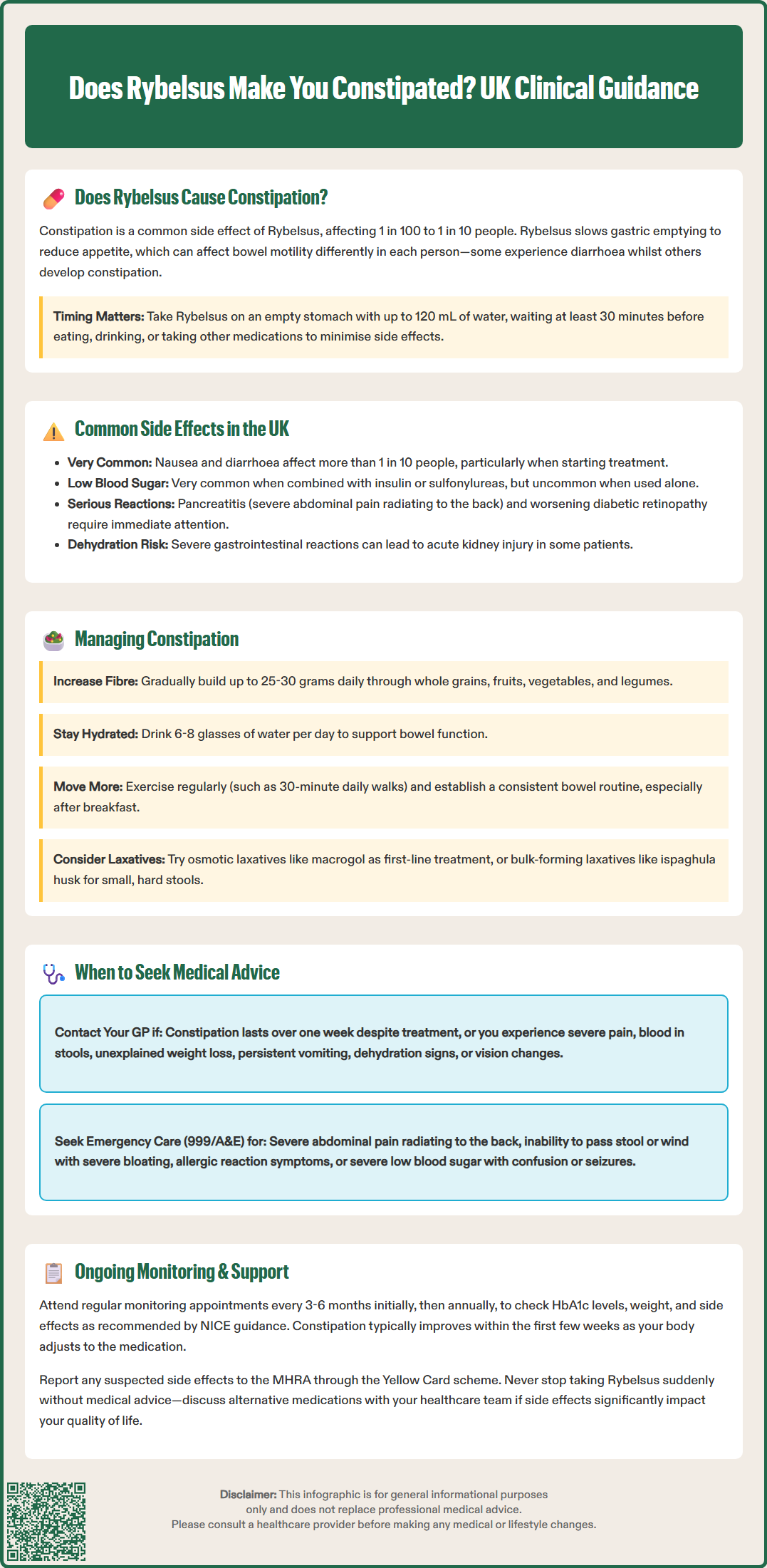
Rybelsus (semaglutide) is an oral GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus. Whilst nausea and diarrhoea are the most frequently reported gastrointestinal side effects, constipation can affect between 1 in 100 and 1 in 10 patients. This occurs because semaglutide slows gastric emptying, which can alter bowel motility in different ways. Constipation is typically most pronounced during initial treatment or dose escalation, and often improves as the body adjusts. Understanding how to recognise, manage, and when to seek medical advice about constipation whilst taking Rybelsus is essential for safe and effective diabetes management.
Quick Answer: Rybelsus can cause constipation in between 1 in 100 and 1 in 10 patients, classified as a 'common' side effect by the MHRA.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereRybelsus (semaglutide) is an oral glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Whilst constipation is not among the most frequently reported adverse effects of Rybelsus, it can occur in some patients during treatment.
The most common gastrointestinal side effects associated with Rybelsus include nausea, diarrhoea, vomiting, and abdominal pain. According to the Summary of Product Characteristics (SmPC) approved by the Medicines and Healthcare products Regulatory Agency (MHRA), constipation is classified as a 'common' adverse reaction, meaning it affects between 1 in 100 and 1 in 10 people taking the medication.
Mechanism of gastrointestinal effects: Semaglutide works by mimicking the action of the naturally occurring hormone GLP-1, which slows gastric emptying and reduces appetite. This delayed gastric emptying can affect bowel motility in different ways—whilst some patients experience diarrhoea, others may develop constipation. The effect varies considerably between individuals and may be influenced by factors such as diet, hydration status, concurrent medications, and underlying gastrointestinal conditions.
It is important to note that gastrointestinal side effects, including constipation, are typically most pronounced during the initial weeks of treatment or following dose escalation. Many patients find that these symptoms improve over time as the body adjusts to the medication. However, persistent or severe constipation warrants medical review to ensure appropriate management and to exclude other contributing factors.
Proper administration may help minimise gastrointestinal effects. Rybelsus should be taken on an empty stomach with up to 120 mL of water, at least 30 minutes before eating, drinking, or taking other oral medicines. If gastrointestinal symptoms persist, your doctor may delay dose escalation beyond the usual one-month interval.
Understanding the full spectrum of potential adverse effects associated with Rybelsus helps patients and healthcare professionals anticipate and manage treatment-related issues effectively. The MHRA-approved product information identifies several categories of side effects based on frequency.
Very common side effects (affecting more than 1 in 10 people):
Nausea – often the most troublesome symptom, particularly during treatment initiation
Diarrhoea – can range from mild to moderate in severity
Common side effects (affecting between 1 in 100 and 1 in 10 people):
Vomiting
Abdominal pain or discomfort
Constipation
Dyspepsia (indigestion)
Gastritis (inflammation of the stomach lining)
Decreased appetite
Cholelithiasis (gallstones)
Hypoglycaemia (low blood sugar) is very common when Rybelsus is used with insulin or sulfonylureas, but uncommon when used alone.
Less common but important side effects include pancreatitis (inflammation of the pancreas) and diabetic retinopathy complications. The risk of retinopathy complications is higher in patients with pre-existing diabetic retinopathy and those experiencing rapid improvement in blood glucose control. Patients should be counselled about recognising symptoms of acute pancreatitis, such as severe, persistent abdominal pain radiating to the back.
Severe gastrointestinal adverse reactions may lead to dehydration, potentially causing acute kidney injury in some patients.
The National Institute for Health and Care Excellence (NICE) guidance on type 2 diabetes management acknowledges that GLP-1 receptor agonists like semaglutide are associated with gastrointestinal adverse effects, and recommends that patients receive appropriate counselling before starting treatment. Healthcare professionals should review the balance of glycaemic benefit against tolerability on an individual basis, particularly in patients with pre-existing gastrointestinal conditions.
Suspected adverse reactions to Rybelsus should be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
If you experience constipation whilst taking Rybelsus, several evidence-based strategies can help alleviate symptoms without necessarily requiring discontinuation of the medication.
Dietary modifications:
Increase dietary fibre intake gradually to 25–30 grams daily through wholegrain cereals, fruits, vegetables, pulses, and legumes
Maintain adequate hydration – aim for 6–8 drinks daily (unless contraindicated by other medical conditions)
Include natural laxative foods such as prunes, figs, and kiwi fruit
Avoid excessive consumption of constipating foods like processed cheese, red meat, and refined carbohydrates
Lifestyle measures:
Regular physical activity – even moderate exercise such as walking for 30 minutes daily can stimulate bowel motility
Establish a regular bowel routine – allow adequate time after meals, particularly breakfast, when the gastrocolic reflex is strongest
Respond promptly to the urge to defecate rather than delaying
Pharmacological options: If lifestyle measures prove insufficient, speak with your GP or pharmacist about appropriate laxatives. Osmotic laxatives (such as macrogol) are generally considered first-line options for chronic constipation. Bulk-forming laxatives (such as ispaghula husk) may be more suitable if your stools are small and hard. Both are available over the counter. Stimulant laxatives (such as senna or bisacodyl) may be used for short-term relief but should not be relied upon long-term without medical supervision.
Medication review: Consider whether other medications you are taking might contribute to constipation. Common culprits include opioid analgesics, certain antidepressants, iron supplements, and some antihypertensive agents. Your GP can review your medication regimen and make adjustments if appropriate.
It is worth noting that constipation related to Rybelsus often improves after the first few weeks of treatment as your body adjusts to the medication. If gastrointestinal symptoms persist, your doctor may delay dose escalation or maintain you on a lower dose for longer. Patience, combined with the measures outlined above, typically results in satisfactory symptom control.
Whilst mild constipation can often be managed with self-care measures, certain symptoms warrant prompt medical attention. Understanding when to contact your GP or seek urgent care is essential for patient safety.
Contact your GP if you experience:
Persistent constipation lasting more than one week despite lifestyle modifications and over-the-counter laxatives
Severe abdominal pain or bloating that does not resolve
Blood in your stools or black, tarry stools
Unexplained weight loss or loss of appetite beyond what is expected with diabetes treatment
Persistent nausea or vomiting that prevents adequate food or fluid intake
Signs of dehydration including reduced urine output, dizziness, or confusion
Right upper abdominal pain, jaundice (yellowing of skin/eyes), pale stools or dark urine which may indicate gallbladder problems
Changes in vision, new floaters or spots particularly if you have pre-existing diabetic retinopathy
Seek urgent medical attention (contact 999 or attend A&E) if you develop:
Severe, persistent abdominal pain radiating to the back, which may indicate pancreatitis
Signs of bowel obstruction including inability to pass stool or wind, severe abdominal distension, and vomiting
Symptoms of severe allergic reaction such as difficulty breathing, facial swelling, or widespread rash
Severe hypoglycaemia with confusion, loss of consciousness, or seizures (particularly relevant if taking Rybelsus with insulin or sulfonylureas)
Regular monitoring: NICE guidance recommends that patients taking GLP-1 receptor agonists should have regular follow-up appointments to assess treatment efficacy, tolerability, and continuation criteria. Your GP or diabetes specialist nurse should review your HbA1c levels, weight, and any adverse effects at appropriate intervals—typically at 3–6 months after initiation and then at least annually.
If side effects are significantly impacting your quality of life or preventing you from taking Rybelsus as prescribed, discuss this with your healthcare team. Alternative GLP-1 receptor agonists, different formulations, or alternative diabetes medications may be more suitable for your individual circumstances. Never stop taking Rybelsus abruptly without medical advice, as this may affect your blood glucose control.
Remember to report any suspected side effects to the MHRA through the Yellow Card scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Constipation is classified as a 'common' adverse reaction to Rybelsus, affecting between 1 in 100 and 1 in 10 people taking the medication. It is typically most pronounced during initial treatment or following dose escalation, and often improves as the body adjusts to semaglutide.
Rybelsus contains semaglutide, a GLP-1 receptor agonist that slows gastric emptying to help control blood glucose levels. This delayed gastric emptying can affect bowel motility differently in individuals—whilst some experience diarrhoea, others may develop constipation.
Contact your GP if constipation persists for more than one week despite lifestyle modifications and over-the-counter laxatives, or if you experience severe abdominal pain, blood in stools, persistent vomiting, or signs of dehydration. Severe, persistent abdominal pain radiating to the back requires urgent medical attention as it may indicate pancreatitis.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.