
Wegovy (semaglutide 2.4 mg) is a GLP-1 receptor agonist licensed for chronic weight management in adults with obesity or overweight with comorbidities. Many patients wonder whether weight loss continues once they reach the maintenance dose of 2.4 mg weekly, or if their weight will stabilise. Clinical evidence shows that whilst most people continue to lose weight after reaching the maintenance dose, the rate typically slows compared to the initial titration phase. Understanding what to expect during long-term maintenance therapy helps patients set realistic goals and optimise treatment outcomes alongside dietary modification, physical activity, and behavioural support.
Quick Answer: Most patients continue to experience gradual weight loss after reaching the 2.4 mg maintenance dose of Wegovy, though the rate typically slows and weight eventually stabilises between 60–68 weeks of treatment.
Wegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. However, NHS access via NICE Technology Appraisal 875 is more restricted, limiting treatment to specialist weight management services with specific BMI criteria (lower thresholds may apply for some ethnic groups, such as those of South Asian origin).
The maintenance dose of Wegovy is 2.4 mg once weekly , which represents the maximum therapeutic dose approved by the Medicines and Healthcare products Regulatory Agency (MHRA). Patients begin treatment at a lower starting dose of 0.25 mg weekly, with gradual increases every four weeks through intermediate doses of 0.5 mg, 1.0 mg, and 1.7 mg before reaching the 2.4 mg maintenance level. This standard titration period spans 16 weeks, though slower escalation may be used if needed for tolerability.
The maintenance dose is designed to provide optimal efficacy in appetite regulation and weight management. Semaglutide works by mimicking the action of endogenous GLP-1, a hormone that regulates appetite and food intake by acting on receptors in the brain's appetite centres. At the 2.4 mg dose, semaglutide achieves sustained receptor activation, promoting feelings of fullness (satiety), reducing hunger, and initially slowing gastric emptying (though this particular effect may diminish over time).
Patients who cannot tolerate the 2.4 mg dose due to persistent adverse effects may remain on the 1.7 mg dose as an alternative maintenance regimen, though this should be discussed with their prescribing clinician. Under NICE guidance, Wegovy should be prescribed as part of a comprehensive weight management programme that includes dietary modification, increased physical activity, and behavioural support, with NHS-funded treatment limited to a maximum of 2 years.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereClinical trial evidence demonstrates that many patients continue to experience weight loss after reaching the 2.4 mg maintenance dose of Wegovy, though the rate of loss typically slows compared to the initial titration phase. The landmark STEP (Semaglutide Treatment Effect in People with obesity) trials showed that participants continued losing weight for up to 68 weeks of treatment, with the most substantial reductions occurring during the first six months.
In the STEP 1 trial, adults without diabetes achieved an average weight loss of approximately 15% of their initial body weight over 68 weeks (compared to 2.4% with placebo). Importantly, weight loss did not plateau immediately upon reaching the maintenance dose; rather, participants experienced continued gradual reductions for several months thereafter. The trajectory of weight loss typically follows a pattern where rapid initial loss during dose escalation transitions to slower, more modest continued loss during the maintenance phase.
It should be noted that weight loss outcomes are typically lower in people with type 2 diabetes, as demonstrated in the STEP 2 trial, where the average weight reduction was approximately 10% at the 2.4 mg dose.
Individual responses vary considerably, and not all patients continue to lose weight once established on the maintenance dose. Some individuals reach a weight plateau where their body weight stabilises, whilst others may experience continued modest reductions. Research from the STEP 1 trial suggests that approximately 85% of patients without diabetes on Wegovy achieve clinically significant weight loss (defined as ≥5% of baseline body weight), with many exceeding this threshold.
It is important to recognise that weight loss is not linear, and temporary plateaus are normal physiological responses. Factors such as metabolic adaptation, changes in body composition, adherence to lifestyle modifications, and individual metabolic differences all influence whether weight loss continues during maintenance therapy. Patients should maintain realistic expectations and understand that stabilisation at a lower weight still represents a successful therapeutic outcome, particularly when accompanied by improvements in cardiometabolic health markers.
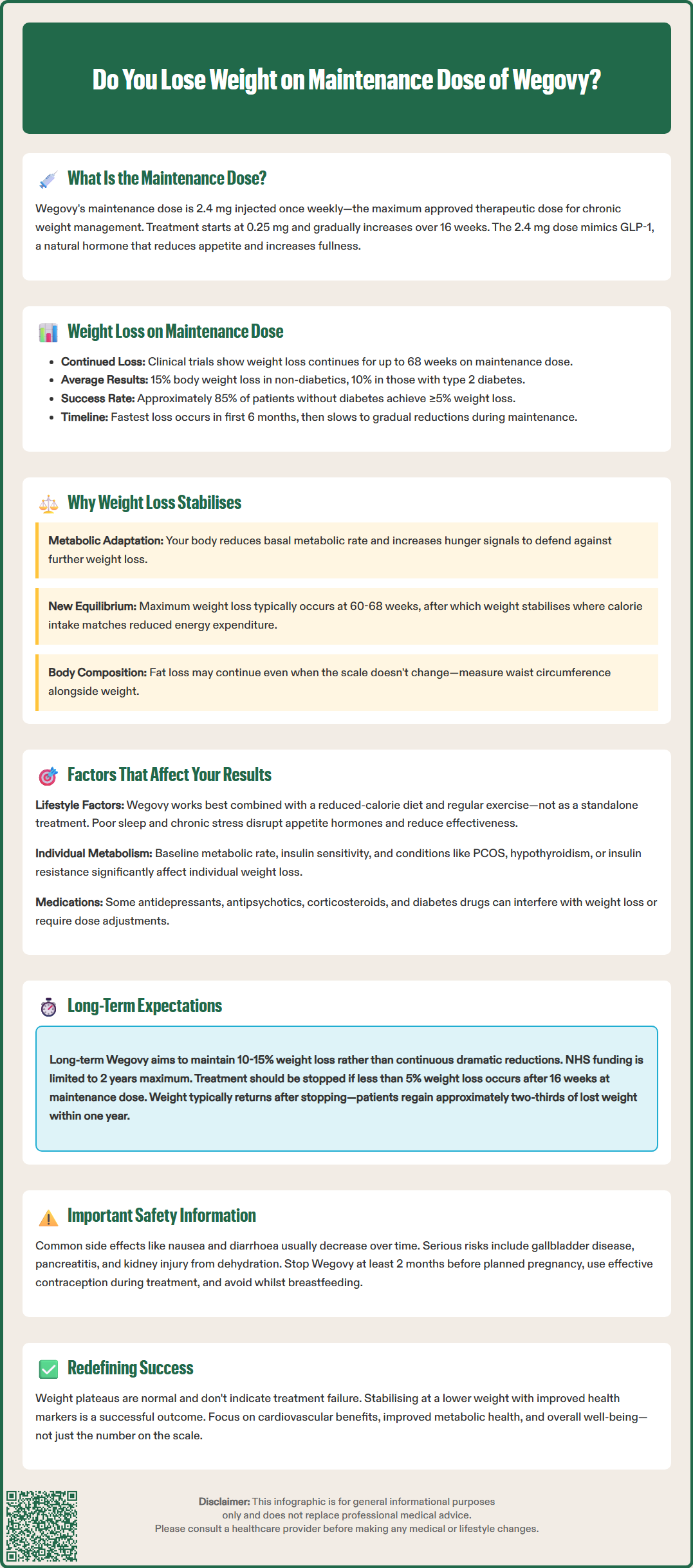
Weight stabilisation during Wegovy maintenance therapy reflects complex physiological adaptations rather than treatment failure. As the body loses weight, several compensatory mechanisms activate to defend against further weight reduction, a phenomenon known as metabolic adaptation or adaptive thermogenesis. These biological responses can slow or halt weight loss even whilst continuing the medication at the maintenance dose.
During sustained weight loss, the body's basal metabolic rate (BMR) typically decreases beyond what would be predicted by the reduction in body mass alone. This means the body becomes more efficient at conserving energy, requiring fewer calories to maintain basic physiological functions. Simultaneously, hormonal changes occur that increase hunger signals and reduce satiety, creating a biological drive to regain lost weight. Wegovy helps counteract some of these compensatory mechanisms through its effects on appetite-regulating hormones, but it does not completely override them. It's worth noting that while semaglutide initially slows gastric emptying, this effect tends to attenuate over time according to the SmPC.
Body composition changes also contribute to weight stabilisation. As patients lose fat mass, they may simultaneously preserve or even gain lean muscle mass, particularly if engaging in resistance exercise. Since muscle tissue is denser than adipose tissue, improvements in body composition may not always reflect on the scales, even though health benefits continue to accrue. Measurements such as waist circumference, body fat percentage, and clothing fit often provide better indicators of progress than weight alone.
Clinical studies, including the STEP 5 trial with 2-year data, indicate that most patients reach their maximum weight loss between 60 and 68 weeks of treatment, after which weight typically stabilises. This plateau represents a new equilibrium point where energy intake matches energy expenditure at the reduced body weight. Maintaining this lower weight requires ongoing treatment, as discontinuation of Wegovy typically results in weight regain, as demonstrated in the STEP 4 trial where participants who switched to placebo regained approximately two-thirds of their lost weight within one year.
Multiple variables influence the extent and duration of weight loss experienced during Wegovy maintenance therapy. Understanding these factors helps patients and clinicians set realistic expectations and optimise treatment outcomes.
Adherence to lifestyle modifications remains paramount. Wegovy is most effective when combined with a reduced-calorie diet and increased physical activity. Patients who maintain consistent dietary changes and regular exercise typically achieve greater weight loss than those relying on medication alone. NICE recommends that Wegovy should only be prescribed alongside a comprehensive weight management programme that addresses nutrition, physical activity, and behavioural factors within tiered weight management services.
Individual metabolic factors significantly impact treatment response. Baseline metabolic rate, insulin sensitivity, genetic predisposition to obesity, and hormonal status all influence how effectively someone loses weight on Wegovy. Patients with conditions such as polycystic ovary syndrome (PCOS), hypothyroidism, or insulin resistance may experience different weight loss trajectories compared to those without these comorbidities. Weight-related conditions like sleep apnoea and osteoarthritis may also improve with treatment. Optimising management of underlying conditions can enhance Wegovy's effectiveness.
Medication interactions and concurrent treatments may affect outcomes. Certain medications, including some antidepressants, antipsychotics, corticosteroids, and diabetes medications, can promote weight gain or interfere with weight loss efforts. In people with type 2 diabetes, concomitant use of insulin or sulfonylureas may require dose adjustment to reduce the risk of hypoglycaemia. Patients should discuss their complete medication regimen with their prescriber to identify potential barriers.
Sleep quality, stress levels, and psychological factors also play crucial roles. Chronic sleep deprivation disrupts appetite-regulating hormones (leptin and ghrelin), whilst elevated cortisol from chronic stress promotes central adiposity. Addressing sleep disorders and implementing stress management techniques can enhance weight loss outcomes. Additionally, emotional eating patterns, binge eating behaviours, and psychological relationship with food require concurrent behavioural support for optimal results.
Age and sex influence treatment response, with some studies suggesting variations in weight loss magnitude between demographic groups, though Wegovy demonstrates efficacy across diverse populations.
Long-term treatment with Wegovy maintenance dose requires realistic expectations, ongoing monitoring, and commitment to lifestyle modifications. Clinical evidence supports the medication's efficacy and safety for extended use, though patients should understand both the benefits and limitations of chronic therapy.
Sustained weight maintenance represents the primary goal of long-term Wegovy therapy. Whilst dramatic continued weight loss beyond 12-18 months is uncommon, maintaining a 10-15% reduction from baseline body weight confers substantial health benefits. Studies demonstrate improvements in cardiovascular risk factors, including reductions in blood pressure, triglycerides, and HbA1c in patients with type 2 diabetes. The SELECT cardiovascular outcomes trial showed that semaglutide 2.4 mg significantly reduced major adverse cardiovascular events in people with established cardiovascular disease, highlighting benefits beyond weight loss alone.
Monitoring and follow-up are essential components of long-term therapy. Treatment response should be evaluated according to the UK SmPC criteria, which recommend assessing the effect after 16 weeks on the 2.4 mg dose (or maximum tolerated). According to the SmPC, treatment should be discontinued if the patient has not lost at least 5% of their initial body weight. Under NICE TA875, NHS-funded treatment is limited to a maximum of 2 years and must be provided within specialist weight management services.
Common adverse effects during maintenance therapy include nausea, diarrhoea, constipation, and abdominal discomfort, though these typically diminish over time. Patients should be aware of important safety considerations including:
Risk of gallbladder disease (cholelithiasis, cholecystitis)
Pancreatitis (persistent severe abdominal pain, especially radiating to the back, warrants immediate medical assessment)
Diabetic retinopathy complications in people with type 2 diabetes
Dehydration and acute kidney injury risk from severe gastrointestinal symptoms
Small increases in heart rate
Not recommended during pregnancy or breastfeeding; treatment should be stopped at least 2 months before planned conception, and effective contraception should be used during treatment
Patients experiencing weight regain or plateau should contact their healthcare provider to discuss optimising lifestyle factors or reviewing their treatment plan. Any suspected side effects should be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Treatment duration remains individualised within the NHS 2-year funding limit. Patients should understand that Wegovy is intended as a chronic therapy; discontinuation typically results in weight regain. Decisions about treatment duration should involve shared decision-making between patient and clinician, weighing ongoing benefits against costs, side effects, and individual circumstances.
Clinical trials show that patients typically continue losing weight for up to 60–68 weeks of treatment, with the most substantial reductions occurring during the first six months. After this period, weight usually stabilises at a lower level.
Weight plateaus are normal physiological responses during maintenance therapy. If you have not lost at least 5% of your initial body weight after 16 weeks on the maintenance dose, treatment should be reviewed and may need to be discontinued according to UK prescribing guidance.
Yes, clinical trials demonstrate that discontinuing Wegovy typically results in weight regain, with patients regaining approximately two-thirds of their lost weight within one year. Wegovy is intended as a long-term chronic therapy to maintain weight loss.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.