GLP-1 receptor agonists, such as semaglutide and liraglutide, are increasingly prescribed in the UK for type 2 diabetes and weight management. Many patients wonder whether these medications might help with elevated cortisol levels, particularly given their metabolic benefits. Whilst GLP-1 therapies improve insulin sensitivity, promote weight loss, and reduce visceral fat—factors that can influence the hypothalamic-pituitary-adrenal axis—they are not licensed or recommended for treating hypercortisolism. This article examines the current evidence on GLP-1 receptor agonists and cortisol regulation, clarifies when specialist assessment is needed, and outlines evidence-based treatments for pathological high cortisol in the UK.
Quick Answer: GLP-1 receptor agonists are not licensed or recommended for treating high cortisol and should not be used for this purpose.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereCortisol is a steroid hormone produced by the adrenal glands, often referred to as the 'stress hormone' because it plays a crucial role in the body's response to stress. Under normal circumstances, cortisol follows a diurnal rhythm, with levels highest in the morning to help us wake and gradually declining throughout the day. It regulates numerous physiological processes including metabolism, immune function, blood pressure, and blood glucose levels.
When cortisol levels remain persistently elevated—a condition known as hypercortisolism—significant health consequences can develop. True pathological hypercortisolism (Cushing's syndrome) is typically caused by endogenous ACTH excess, adrenal disease, or exogenous glucocorticoid medication use, rather than by chronic psychological stress alone. The effects of persistent high cortisol are wide-ranging and can include:
Weight gain, particularly around the abdomen and face
Insulin resistance and increased risk of type 2 diabetes
Hypertension (high blood pressure)
Osteoporosis and increased fracture risk
Mood disturbances, including anxiety and depression
Immune suppression, leading to increased infection susceptibility
Muscle weakness and skin changes
The relationship between cortisol and metabolic health is particularly significant. Elevated cortisol promotes gluconeogenesis (glucose production in the liver), reduces insulin sensitivity, and encourages fat deposition in visceral areas. This creates a metabolic environment that overlaps considerably with conditions such as metabolic syndrome and type 2 diabetes.
It's important to note that random cortisol measurements are not diagnostic for Cushing's syndrome. Proper screening requires specialised tests such as overnight dexamethasone suppression tests, late-night salivary cortisol, or 24-hour urinary free cortisol measurements, usually with at least two abnormal results. Some conditions, including alcohol misuse and severe depression, can cause 'pseudo-Cushing's' states that may affect test results and require specialist assessment.
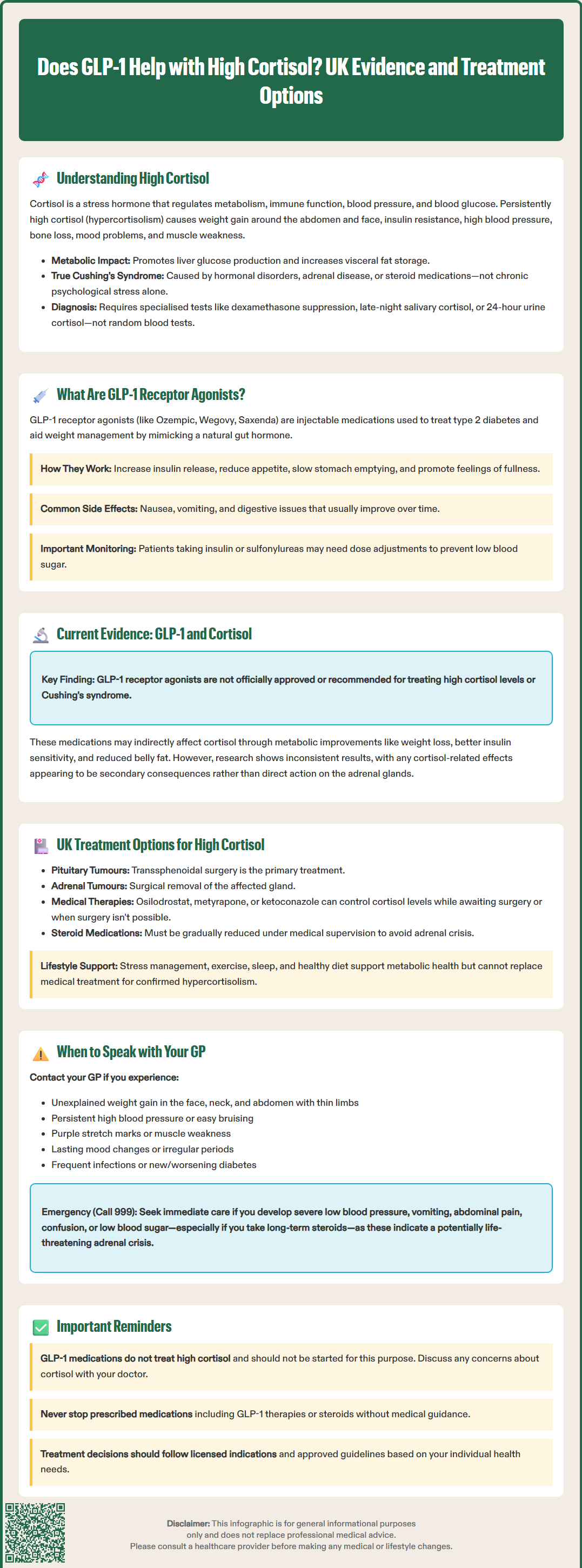
GLP-1 (glucagon-like peptide-1) receptor agonists are a class of medications primarily licensed in the UK for the treatment of type 2 diabetes and, more recently, for weight management in specific patient groups. These medicines include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and exenatide, among others. They are available on NHS prescription when NICE criteria are met (as outlined in NICE NG28 for type 2 diabetes and relevant technology appraisals for weight management), and are administered via subcutaneous injection, typically weekly or daily depending on the formulation.
GLP-1 is an incretin hormone naturally produced in the intestine in response to food intake. GLP-1 receptor agonists mimic this natural hormone, binding to GLP-1 receptors found throughout the body, including the pancreas, brain, gastrointestinal tract, and cardiovascular system. Their primary mechanisms of action include:
Enhancing glucose-dependent insulin secretion from pancreatic beta cells
Suppressing glucagon release, thereby reducing hepatic glucose production
Slowing gastric emptying, which moderates post-meal glucose spikes
Reducing appetite through central nervous system effects, particularly in hypothalamic regions
Promoting satiety, leading to reduced caloric intake
These medications have demonstrated significant benefits in glycaemic control, weight reduction, and cardiovascular risk reduction in clinical trials. Common adverse effects include nausea, vomiting, diarrhoea, and constipation, which typically diminish over time. More serious but rare complications can include pancreatitis and gallbladder disease.
Important safety considerations include:
Increased hypoglycaemia risk when used with insulin or sulfonylureas (dose adjustments of these medications may be needed)
Potential worsening of diabetic retinopathy with rapid improvement in blood glucose control, particularly with semaglutide
Need for monitoring in patients with pre-existing retinopathy
The MHRA continues to monitor the safety profile of these agents. Patients are encouraged to report suspected side effects via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk). Whilst GLP-1 receptor agonists have well-established metabolic benefits, their direct effects on cortisol regulation remain an area of ongoing research rather than established clinical practice.
The question of whether GLP-1 receptor agonists directly influence cortisol levels is complex, and there is no official link established between GLP-1 therapy and the treatment of hypercortisolism. These medications are not licensed or recommended by NICE or the MHRA for managing elevated cortisol levels, and they should not be considered a treatment for Cushing's syndrome or other primary causes of hypercortisolism.
However, emerging research has explored potential indirect relationships between GLP-1 receptor agonist therapy and cortisol regulation. Some studies have investigated whether the metabolic improvements seen with GLP-1 therapy—including weight loss, improved insulin sensitivity, and reduced visceral adiposity—might secondarily influence cortisol dynamics. The hypothalamic-pituitary-adrenal (HPA) axis, which regulates cortisol production, is known to be affected by metabolic status, obesity, and insulin resistance.
Limited preclinical and clinical data suggest that GLP-1 receptor agonists might modestly influence cortisol metabolism or HPA axis function in certain contexts, but findings have been inconsistent and not practice-changing. Some research has shown no significant changes in cortisol levels with GLP-1 therapy, whilst other studies have reported subtle alterations in cortisol rhythms or stress responses. Importantly, any observed effects appear to be indirect consequences of metabolic improvement rather than direct pharmacological actions on the adrenal glands or HPA axis.
For patients with true hypercortisolism (such as Cushing's syndrome), specific treatments targeting the underlying cause are required. These may include surgical removal of tumours, medications that block cortisol production (such as metyrapone or ketoconazole), or in some cases, adrenalectomy. GLP-1 receptor agonists would not replace these evidence-based interventions, though they might be used concurrently to manage associated metabolic complications such as diabetes, if clinically appropriate and under specialist guidance.
The management of elevated cortisol levels in the UK follows a structured diagnostic and therapeutic pathway, typically coordinated through endocrinology services. The first essential step is confirming whether cortisol elevation is pathological and identifying its underlying cause. NICE guidance emphasises the importance of appropriate investigation before initiating treatment.
Diagnostic investigations for suspected hypercortisolism may include:
24-hour urinary free cortisol measurements
Late-night salivary cortisol testing
Low-dose dexamethasone suppression test
Plasma ACTH levels to distinguish ACTH-dependent from ACTH-independent causes
Imaging studies (pituitary MRI, adrenal CT) when biochemical testing confirms Cushing's syndrome
At least two abnormal screening results are usually sought before proceeding to imaging, and conditions causing pseudo-Cushing's states (such as alcohol misuse or severe depression) should be considered.
Treatment approaches depend entirely on the underlying aetiology:
For Cushing's disease (pituitary adenoma): transsphenoidal surgery is the first-line treatment, with radiotherapy or medical therapy reserved for cases where surgery is unsuccessful or not feasible. Medical options include pasireotide, osilodrostat (NICE-approved), and cabergoline (used off-label).
For adrenal tumours: surgical adrenalectomy is typically curative for benign adenomas. Adrenal carcinoma requires specialist oncological management.
For ectopic ACTH syndrome: treatment focuses on the underlying tumour, often requiring surgical resection and oncological therapies.
For iatrogenic hypercortisolism (corticosteroid medication): gradual dose reduction under medical supervision is essential, as abrupt cessation can precipitate adrenal crisis.
Medical management to control cortisol excess whilst awaiting definitive treatment may include metyrapone, ketoconazole, or mitotane. These medications work by inhibiting cortisol synthesis at various enzymatic steps. Patients receiving these treatments require regular monitoring of cortisol levels, liver function (particularly with ketoconazole), electrolytes (especially with metyrapone and osilodrostat), and blood pressure. Lifestyle modifications including stress management, regular physical activity, adequate sleep, and a balanced diet support overall metabolic health but cannot substitute for specific treatment when pathological hypercortisolism is present.
Many people experience temporary elevations in cortisol due to everyday stress, illness, or lifestyle factors, which typically resolve without medical intervention. However, certain symptoms and circumstances warrant medical evaluation to exclude pathological hypercortisolism or other endocrine disorders.
You should contact your GP if you experience:
Unexplained weight gain, particularly affecting the face (moon face), neck (buffalo hump), and abdomen, with relatively thin arms and legs
Persistent hypertension that is difficult to control with standard medications
Easy bruising or thin, fragile skin that heals poorly
Purple or red stretch marks (striae) on the abdomen, thighs, or breasts
Muscle weakness, particularly affecting the shoulders and hips
Mood changes including depression, anxiety, or irritability that persist despite usual management
Irregular menstrual periods or reduced libido
Recurrent infections or poor wound healing
New-onset diabetes or worsening glycaemic control in established diabetes
Seek urgent medical attention if you develop signs of adrenal crisis, which can occur in patients with adrenal insufficiency (often after withdrawal of long-term steroids). Symptoms include severe hypotension, vomiting, abdominal pain, confusion, and hypoglycaemia. Call 999 or attend the Emergency Department and use emergency hydrocortisone if available. Patients on long-term steroids should carry the UK Steroid Emergency Card and discuss sick-day rules with their healthcare provider.
Your GP will take a thorough history, including details of any corticosteroid medications (tablets, inhalers, creams, or injections), perform a physical examination, and may arrange initial blood tests. If hypercortisolism is suspected, referral to an endocrinologist is appropriate for specialist investigation and management.
Regarding GLP-1 receptor agonists specifically, if you are already prescribed these medications for diabetes or weight management and have concerns about cortisol levels, discuss this with your GP or diabetes specialist. However, remember that GLP-1 medications are not treatments for high cortisol and should not be started with this expectation. Do not stop any prescribed medications, including GLP-1 therapies or steroids, without medical guidance. Any decision to initiate or continue GLP-1 therapy should be based on licensed indications and NICE-approved criteria, considering your individual metabolic health needs and treatment goals.
No, GLP-1 receptor agonists are not licensed or recommended for treating high cortisol. They are prescribed for type 2 diabetes and weight management, and any potential effects on cortisol appear indirect through metabolic improvements rather than direct hormonal action.
Treatment depends on the underlying cause and typically involves specialist endocrinology care. Options include transsphenoidal surgery for pituitary adenomas, adrenalectomy for adrenal tumours, or cortisol-blocking medications such as metyrapone, ketoconazole, or osilodrostat whilst awaiting definitive treatment.
Consult your GP if you experience unexplained weight gain (particularly facial and abdominal), persistent hypertension, easy bruising, purple stretch marks, muscle weakness, or mood changes. Your GP can arrange appropriate investigations and refer you to endocrinology if needed.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.