Mounjaro (tirzepatide) is a dual GIP/GLP-1 receptor agonist licensed in the UK for type 2 diabetes and chronic weight management in adults with obesity. Whilst it is not indicated for arthritis treatment, the substantial weight loss achieved with Mounjaro—averaging 15–22% of body weight in clinical trials—has prompted questions about potential benefits for osteoarthritis symptoms. Excess weight significantly increases mechanical stress on weight-bearing joints and promotes systemic inflammation, both contributing to arthritis progression. This article examines the current evidence on whether Mounjaro helps with arthritis, the mechanisms linking weight loss to joint health, and important considerations for patients.
Quick Answer: Mounjaro is not licensed or indicated for arthritis treatment, but the substantial weight loss it facilitates may indirectly improve osteoarthritis symptoms by reducing mechanical joint stress and systemic inflammation.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a prescription medication licensed in the UK for the treatment of type 2 diabetes mellitus and, more recently, for chronic weight management in adults with obesity or overweight with weight-related comorbidities. It belongs to a novel class of medicines known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists.
The medication works through a sophisticated mechanism of action. By activating both GIP and GLP-1 receptors, Mounjaro enhances insulin secretion when blood glucose levels are elevated, suppresses inappropriate glucagon release, slows gastric emptying, and reduces appetite through effects on the central nervous system. This dual action distinguishes it from single GLP-1 receptor agonists and contributes to its efficacy in glycaemic control and weight reduction.
Mounjaro is administered as a once-weekly subcutaneous injection, with doses typically starting at 2.5 mg for 4 weeks, then titrated in 2.5 mg increments at minimum 4-week intervals up to a maximum of 15 mg, depending on individual response and tolerability. For weight management, NHS treatment is typically available through specialist weight management services for patients meeting specific NICE criteria, including BMI thresholds and weight-related comorbidities, with defined treatment durations.
It is important to note that Mounjaro is not currently licensed or indicated for the treatment of arthritis. Its primary therapeutic targets remain diabetes management and weight reduction. However, the significant weight loss achieved with this medication has prompted questions about potential secondary benefits for weight-sensitive conditions, including osteoarthritis.
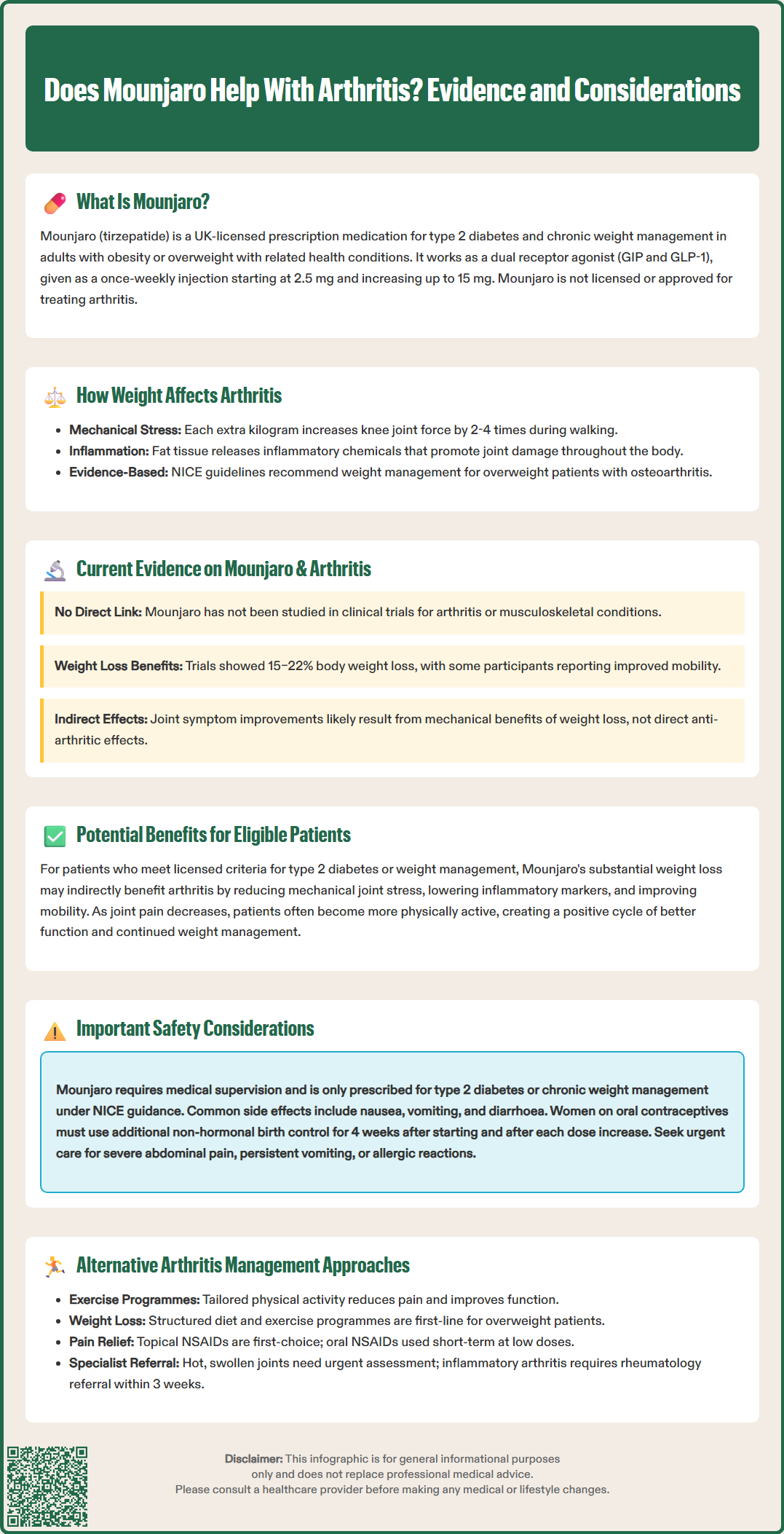
Excess body weight plays a substantial role in the development and progression of osteoarthritis (OA), particularly in weight-bearing joints such as the knees, hips, and ankles. The relationship between obesity and arthritis is multifaceted, involving both mechanical and metabolic factors.
Mechanical stress is the most obvious connection. Each additional kilogram of body weight increases the force across the knee joint during walking by approximately 2-4 times, according to biomechanical studies. This increased load accelerates cartilage degradation, promotes inflammation within the joint space, and contributes to pain and functional limitation. Research consistently demonstrates that weight reduction can significantly decrease joint loading and slow disease progression.
Beyond mechanical factors, adipose tissue is now recognised as an active endocrine organ that secretes pro-inflammatory cytokines and adipokines, including interleukin-6 (IL-6), tumour necrosis factor-alpha (TNF-α), and leptin. These inflammatory mediators contribute to systemic low-grade inflammation, which may exacerbate joint inflammation and cartilage breakdown. This metabolic component helps explain why obesity is also associated with increased risk of osteoarthritis in non-weight-bearing joints, such as the hands.
Clinical evidence supports weight loss as a cornerstone intervention for osteoarthritis management. NICE guideline NG226 recommends weight management for overweight or obese patients with osteoarthritis, noting that any weight loss is beneficial, with greater improvements seen with larger losses of around 10% or more of body weight. This established relationship has led to interest in whether medications that facilitate substantial weight loss, such as Mounjaro, might indirectly benefit arthritis symptoms.
At present, there is no official link established between Mounjaro and direct treatment of arthritis. The medication has not been studied in clinical trials specifically designed to evaluate its effects on arthritis outcomes, and it does not have a licensed indication for any rheumatological or musculoskeletal condition.
However, emerging data from weight management trials provide some relevant insights. In the SURMOUNT clinical trial programme (published in NEJM and JAMA), which evaluated tirzepatide for chronic weight management, participants achieved substantial weight loss—averaging 15–22% of initial body weight depending on dose. Patient-reported outcomes from these studies have suggested improvements in physical function and mobility, which may indirectly reflect reduced joint stress in individuals with underlying osteoarthritis.
Some observational data from diabetes trials have noted that patients with concurrent osteoarthritis reported subjective improvements in joint symptoms following significant weight reduction with GLP-1 receptor agonists. Whilst these observations are encouraging, they do not constitute robust evidence of a direct therapeutic effect on arthritis pathology. The improvements likely reflect the mechanical and metabolic benefits of weight loss rather than any specific anti-arthritic properties of the medication itself.
It is crucial to emphasise that Mounjaro should not be considered a treatment for arthritis. Patients with arthritis who are considering this medication should do so only if they meet the licensed criteria for type 2 diabetes or weight management, and any potential joint-related benefits should be viewed as secondary outcomes. Further research, including dedicated trials examining joint-specific endpoints, would be needed to establish any formal role for tirzepatide in arthritis management.
For individuals with both obesity and osteoarthritis, achieving significant weight loss through any means—including pharmacotherapy like Mounjaro—may confer several important benefits for joint health and symptom management.
Reduced mechanical loading is the most immediate benefit. Weight loss decreases the compressive forces acting on weight-bearing joints during daily activities. Biomechanical studies have shown that each kilogram of weight lost can reduce knee joint loading forces significantly during walking. This reduction in mechanical stress can slow cartilage degradation, decrease pain, and improve functional capacity. Patients often report enhanced mobility, reduced stiffness, and greater ease in performing activities of daily living.
Metabolic improvements accompanying weight loss may also benefit joint health. Reduction in adipose tissue mass decreases circulating levels of pro-inflammatory cytokines and adipokines, potentially reducing systemic inflammation that contributes to arthritis progression. Improved insulin sensitivity and glycaemic control—additional benefits of Mounjaro—may further reduce inflammatory markers and oxidative stress.
Enhanced physical function creates a positive cycle. As joint pain decreases and mobility improves, patients often become more physically active, which strengthens periarticular muscles, improves joint stability, and supports further weight management. This increased activity tolerance can significantly enhance quality of life and independence.
Clinical guidelines, including those from NICE (NG226) and Versus Arthritis, consistently recommend weight management as a core component of osteoarthritis treatment. For patients who meet criteria for Mounjaro use (diabetes or obesity), the substantial weight loss achievable with this medication may provide meaningful indirect benefits for arthritis symptoms, though these should be considered secondary to its primary indications.
Patients considering Mounjaro must understand that this medication is only appropriate for specific licensed indications and requires careful medical supervision. It is not a treatment for arthritis and should only be prescribed when criteria for type 2 diabetes management or chronic weight management are met according to NICE guidance.
Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, constipation, and abdominal discomfort. These effects are typically most pronounced during dose initiation and escalation, and often improve with continued use. Patients should be counselled about these potential side effects and strategies to minimise them, such as eating smaller meals and avoiding high-fat foods.
Important safety considerations include risk of pancreatitis, gallbladder disease (cholelithiasis, cholecystitis), and potential worsening of diabetic retinopathy in patients with type 2 diabetes (particularly those on insulin). Tirzepatide can also reduce the effectiveness of oral contraceptives; women should use additional non-hormonal contraception for 4 weeks after starting treatment and for 4 weeks after each dose increase. The medication is not recommended for those under 18 years of age.
Patients should seek urgent medical attention if they experience:
Severe, persistent abdominal pain (potential pancreatitis)
Right upper abdominal pain, fever, or yellowing of skin/eyes (gallbladder problems)
Symptoms of hypoglycaemia (particularly if taking insulin or sulfonylureas, which may need dose adjustment)
Severe or persistent vomiting leading to dehydration
Allergic reactions or injection site problems
Cost and access considerations are also relevant. Mounjaro is available on NHS prescription only for patients meeting specific eligibility criteria. Private prescriptions are available but can be expensive. Patients should discuss realistic expectations, treatment duration, and long-term weight maintenance strategies with their healthcare provider before commencing therapy.
Suspected adverse reactions should be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
For patients with arthritis, particularly osteoarthritis, a comprehensive management approach incorporating multiple evidence-based interventions typically provides the best outcomes. NICE guideline NG226 recommends a multimodal strategy that does not rely on any single treatment.
Core interventions include:
Exercise and physical activity: Strengthening and aerobic exercise programmes tailored to individual ability can reduce pain, improve function, and support weight management. Physiotherapy referral may be beneficial.
Weight management: For overweight or obese patients, structured weight loss programmes combining dietary modification and increased physical activity remain first-line approaches.
Pain management: Topical NSAIDs (non-steroidal anti-inflammatory drugs) are the first-line pharmacological option. Oral NSAIDs may be considered for short-term use at the lowest effective dose in patients without contraindications, with appropriate gastroprotection. Paracetamol is not recommended for routine use, and opioids should generally be avoided.
Education and self-management: Understanding arthritis, pacing activities, and using aids or adaptations can significantly improve quality of life.
Additional options may include:
Intra-articular corticosteroid injections for symptom flares
Assistive devices such as walking aids, shoe insoles, or joint supports
Referral to rheumatology or orthopaedics for specialist assessment, particularly if symptoms are severe, rapidly progressive, or inadequately controlled with conservative measures
For patients with inflammatory arthritis (such as rheumatoid arthritis), disease-modifying treatments and specialist rheumatology care are essential. A hot, swollen joint with fever requires same-day urgent assessment to rule out septic arthritis. Suspected new-onset inflammatory arthritis warrants urgent rheumatology referral (aim to be seen within 3 weeks).
Patients should consult their GP to develop an individualised management plan that addresses their specific type of arthritis, symptom severity, comorbidities, and treatment goals. Whilst medications like Mounjaro may indirectly benefit some patients through weight reduction, they should not replace established arthritis treatments or delay appropriate specialist referral when indicated.
No, Mounjaro is not licensed or approved for arthritis treatment. It is only indicated for type 2 diabetes mellitus and chronic weight management in adults with obesity or overweight with weight-related comorbidities.
Yes, the substantial weight loss achieved with Mounjaro may indirectly improve osteoarthritis symptoms by reducing mechanical stress on weight-bearing joints and decreasing systemic inflammation. NICE recommends weight management as a core osteoarthritis intervention, with greater benefits seen with larger weight losses.
Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, and diarrhoea. Serious risks include pancreatitis, gallbladder disease, potential worsening of diabetic retinopathy, and reduced effectiveness of oral contraceptives requiring additional contraception during treatment initiation and dose escalation.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.