Does Rybelsus make you hungry? Rybelsus (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for treating type 2 diabetes mellitus. The medication works by mimicking naturally occurring GLP-1, a hormone that typically reduces appetite and promotes feelings of fullness. For most patients, Rybelsus suppresses rather than increases hunger, contributing to modest weight loss through reduced caloric intake. However, individual responses vary, and some people report experiencing increased appetite whilst taking this medication. Understanding why this occurs and how to manage appetite changes is important for optimising diabetes treatment outcomes.
Quick Answer: Rybelsus typically reduces rather than increases hunger by mimicking GLP-1, a hormone that suppresses appetite and slows gastric emptying.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereRybelsus (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus, not for weight management. The medication works by mimicking the action of naturally occurring GLP-1, a hormone released from the intestine in response to food intake. This mechanism has several important effects on glucose regulation and appetite control.
When Rybelsus binds to GLP-1 receptors in the brain—particularly in areas such as the hypothalamus and brainstem—it typically reduces appetite and promotes feelings of satiety. The drug slows gastric emptying (most pronounced early in treatment), meaning food remains in the stomach for longer periods, which normally contributes to prolonged fullness after meals. This gastric-slowing effect may also affect the absorption of some oral medicines, such as levothyroxine. Additionally, semaglutide enhances insulin secretion in a glucose-dependent manner and suppresses inappropriate glucagon release, helping to stabilise blood glucose levels throughout the day.
For most patients, the predominant effect of Rybelsus is appetite suppression rather than increased hunger. Clinical trials have consistently demonstrated that GLP-1 receptor agonists lead to modest weight loss, primarily through reduced caloric intake. The PIONEER clinical trial programme, which evaluated oral semaglutide, showed that patients typically experienced decreased appetite as a common effect of treatment, with the MHRA/EMC SmPC listing decreased appetite as a common adverse reaction.
However, individual responses to medications can vary considerably. Whilst the pharmacological action of Rybelsus is designed to reduce hunger signals, some patients report experiencing increased appetite or persistent hunger. Understanding why this occurs requires consideration of multiple factors, including dosing, metabolic adaptation, blood glucose fluctuations, and individual physiological differences in drug response.
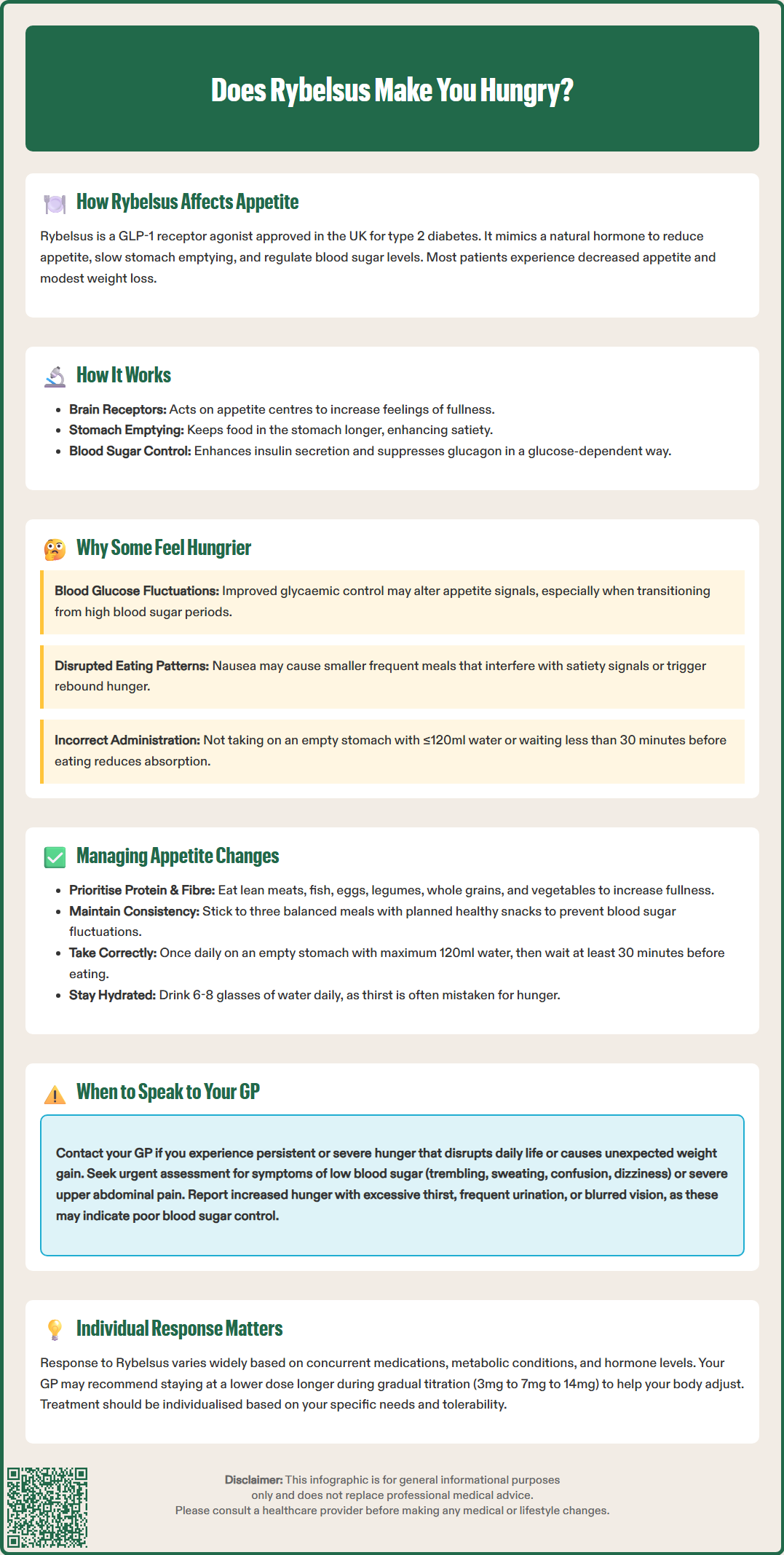
Although increased hunger is not a typical or commonly reported side effect of Rybelsus, several factors may potentially contribute to this experience in some individuals. Blood glucose fluctuations could play a role. As Rybelsus improves glycaemic control and lowers blood glucose levels, some patients—particularly those transitioning from periods of hyperglycaemia—may experience changes in appetite signals. It's important to note that true hypoglycaemia is uncommon with Rybelsus monotherapy but the risk increases when combined with insulin or sulfonylureas.
Metabolic adaptation might theoretically influence appetite. When Rybelsus effectively reduces caloric intake and promotes weight loss, the body may respond with counter-regulatory mechanisms designed to preserve energy stores. This hypothesis, while plausible, has not been specifically established for GLP-1 receptor agonists in clinical studies.
Gastrointestinal side effects commonly associated with Rybelsus—including nausea, vomiting, and abdominal discomfort—may paradoxically lead to altered eating patterns. Some individuals may eat smaller, more frequent meals to manage nausea, which can disrupt normal satiety signals and create a perception of increased hunger. Additionally, if patients experience significant nausea that prevents adequate food intake, subsequent hunger may feel more intense once the nausea subsides.
Incorrect administration is a practical factor that can affect Rybelsus efficacy. The medication must be taken on an empty stomach with no more than 120 ml of water, followed by waiting at least 30 minutes before consuming food, drinks, or other oral medicines. Tablets should be swallowed whole. Poor absorption due to incorrect administration may reduce glycaemic benefits and potentially affect appetite regulation.
There is also considerable individual variation in response to GLP-1 receptor agonists. Concurrent medications, existing metabolic conditions, and baseline hormone levels can all influence how a person responds to semaglutide. It is important to note that there is no official link established between Rybelsus and increased hunger as a direct pharmacological effect, but individual experiences warrant clinical attention.
If you experience increased hunger whilst taking Rybelsus, several practical strategies can help manage this symptom whilst maintaining the therapeutic benefits of the medication. Dietary modifications form the cornerstone of appetite management. Focus on consuming meals rich in protein, fibre, and healthy fats, which promote satiety and help stabilise blood glucose levels. Foods such as lean meats, fish, eggs, legumes, whole grains, vegetables, nuts, and seeds can help you feel fuller for longer periods, in line with NHS healthy eating guidance for diabetes.
Meal timing and structure are equally important. Rather than skipping meals or eating irregularly, establish a consistent eating schedule with three balanced meals and planned healthy snacks if needed. This approach helps prevent excessive hunger and maintains stable blood glucose levels throughout the day. Avoid prolonged fasting periods, which may intensify hunger sensations and make blood glucose management more challenging.
Correct administration of Rybelsus is essential for optimal effect. Always take Rybelsus once daily on an empty stomach with no more than 120 ml of water. Swallow the tablet whole and wait at least 30 minutes before eating, drinking, or taking other oral medicines. Poor absorption due to incorrect administration may reduce the medication's effectiveness.
Monitoring blood glucose levels may provide valuable insights, but only if you have been advised to self-monitor or already do so routinely. Many people with type 2 diabetes in the UK do not perform regular self-monitoring unless specifically recommended. If you notice patterns of increased hunger associated with glucose fluctuations, discuss this with your healthcare team. Adjustments to your diabetes management plan—including timing of Rybelsus, other medications, or meal composition—may be necessary.
Adequate hydration is often overlooked but essential. Sometimes thirst can be mistaken for hunger, and maintaining good fluid intake supports overall metabolic function. Aim for approximately 6–8 glasses of water daily, unless advised otherwise by your healthcare provider.
Gradual dose titration may help minimise appetite disturbances. Rybelsus is typically initiated at 3 mg daily for one month, then increased to 7 mg, with a possible further increase to 14 mg if additional glycaemic control is needed. If you experience significant appetite changes, your GP may recommend remaining at a lower dose for a longer period to allow your body to adjust. Never alter your dose without medical guidance, as this could compromise diabetes control.
Whilst some appetite variation is normal when starting or adjusting diabetes medications, certain situations warrant prompt discussion with your GP or diabetes specialist nurse. Persistent or severe hunger that interferes with your daily activities, causes significant distress, or leads to unintended weight gain should be evaluated. Your healthcare provider can assess whether the hunger is related to Rybelsus, another medication, or an underlying metabolic issue requiring investigation.
Contact your GP if you experience symptoms of hypoglycaemia alongside increased hunger, such as trembling, sweating, confusion, palpitations, or dizziness. These symptoms require urgent assessment, as they may indicate that your diabetes medications need adjustment. If you are taking Rybelsus in combination with insulin or sulfonylureas, the risk of hypoglycaemia is higher, and dose modifications may be necessary.
Unexplained weight gain whilst taking Rybelsus is unusual and should be investigated. Given that GLP-1 receptor agonists typically promote modest weight loss, significant weight gain may suggest inadequate diabetes control, fluid retention, or another medical condition requiring attention. Your GP may wish to review your HbA1c, renal function, and overall diabetes management strategy.
Seek immediate medical advice if you experience severe, persistent upper abdominal pain (which may radiate to your back) with or without vomiting, as these could be symptoms of acute pancreatitis. Similarly, report symptoms of gallbladder disease such as pain in the upper right abdomen, fever, or yellowing of the skin or eyes. Severe or persistent vomiting that leads to dehydration also requires urgent medical attention.
If you have pre-existing diabetic retinopathy, particularly if you are also taking insulin, be aware that rapid improvement in blood glucose control can sometimes be associated with temporary worsening of retinopathy. Report any visual changes promptly to your healthcare team.
You should also seek medical advice if increased hunger is accompanied by other concerning symptoms such as excessive thirst, frequent urination, fatigue, or blurred vision—signs that may indicate inadequate glycaemic control. Similarly, if gastrointestinal side effects (nausea, vomiting, diarrhoea, or abdominal pain) are severe or persistent, medical review is essential, as these may require dose adjustment or consideration of alternative treatments.
According to NICE guidance on type 2 diabetes management (NG28), treatment should be individualised based on efficacy, tolerability, and patient preference, including consideration of comorbidities such as cardiovascular disease or chronic kidney disease where SGLT2 inhibitors might be preferred. If Rybelsus is not providing adequate symptom control or is causing problematic side effects, your healthcare team can discuss alternative GLP-1 receptor agonists or other glucose-lowering therapies that may be better suited to your needs.
If you suspect you are experiencing side effects from Rybelsus, you can report these through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app). Regular monitoring and open communication with your diabetes care team ensure optimal treatment outcomes and quality of life.
Rybelsus typically decreases appetite rather than increasing it. The medication works by mimicking GLP-1, a hormone that reduces hunger signals in the brain and slows gastric emptying, leading to prolonged feelings of fullness after meals.
Increased hunger on Rybelsus may result from blood glucose fluctuations, incorrect administration reducing drug absorption, gastrointestinal side effects disrupting normal eating patterns, or individual metabolic variation. This is not a typical pharmacological effect and warrants discussion with your GP.
Contact your GP if you experience persistent or severe hunger interfering with daily activities, symptoms of hypoglycaemia (trembling, sweating, confusion), unexplained weight gain, or severe gastrointestinal symptoms. These situations may require medication adjustment or further investigation.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.