
Tirzepatide (Mounjaro) is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus. Whilst patients often enquire whether tirzepatide causes high cholesterol, clinical evidence suggests the opposite: this medication typically improves lipid profiles rather than elevating cholesterol levels. Understanding tirzepatide's effects on cardiovascular risk markers, including cholesterol, is essential for patients and clinicians managing type 2 diabetes. This article examines the relationship between tirzepatide and cholesterol levels, drawing on clinical trial data and UK guidance to provide evidence-based information on lipid management during treatment.
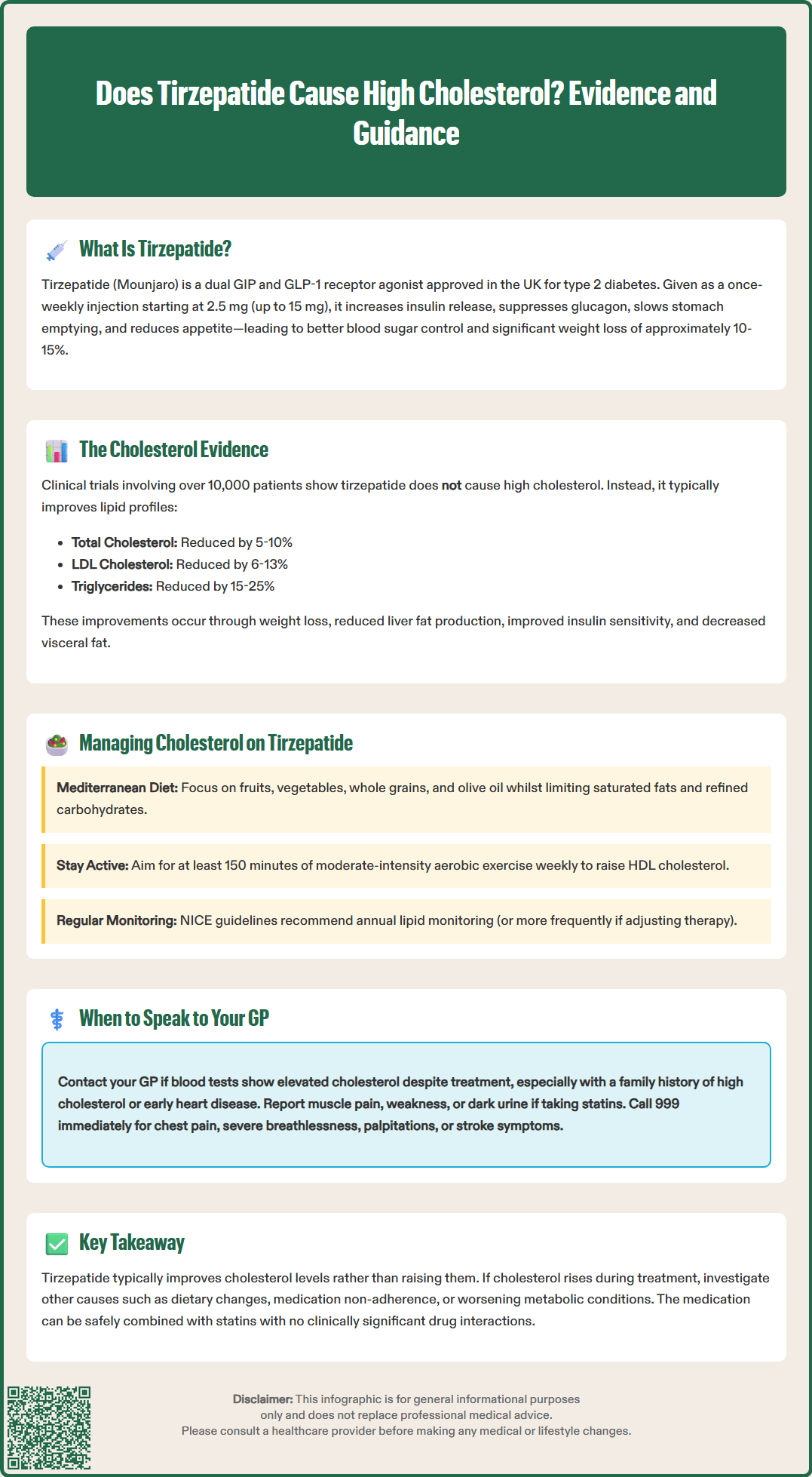
Quick Answer: Tirzepatide does not typically cause high cholesterol; clinical trials demonstrate it generally improves lipid profiles with reductions in total cholesterol, LDL-C, and triglycerides.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereTirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist authorised in the UK for the treatment of type 2 diabetes mellitus. It is marketed under the brand name Mounjaro and has been recommended by NICE for treating insufficiently controlled type 2 diabetes.
The medication works through a dual mechanism of action by simultaneously activating both GIP and GLP-1 receptors. This dual agonism enhances insulin secretion in a glucose-dependent manner, meaning insulin is primarily released when blood glucose levels are elevated. Additionally, tirzepatide suppresses glucagon secretion, slows gastric emptying, and promotes satiety through central nervous system pathways, leading to reduced caloric intake and weight loss.
Administered as a once-weekly subcutaneous injection, tirzepatide is initiated at 2.5 mg for 4 weeks (for tolerability, not glycaemic control) and then gradually titrated upwards to minimise gastrointestinal side effects. The maximum licensed dose for diabetes management is 15 mg weekly. The SURPASS clinical trials demonstrated that tirzepatide reduces HbA1c levels and body weight, with weight loss of up to approximately 10-15% observed in diabetes studies.
While tirzepatide has a low intrinsic risk of hypoglycaemia due to its glucose-dependent mechanism, this risk increases when combined with insulin or sulfonylureas, which may require dose adjustments of these medications.
Beyond glycaemic control and weight reduction, clinical studies suggest tirzepatide may have effects on various cardiometabolic risk factors, including blood pressure and lipid profiles, which are important considerations when evaluating its impact on cardiovascular health markers such as cholesterol levels.
Evidence from clinical trials indicates that tirzepatide does not typically cause high cholesterol. In fact, data from the SURPASS programme, which evaluated tirzepatide in patients with type 2 diabetes, demonstrated that the medication generally has neutral-to-beneficial effects on lipid profiles, with individual responses varying.
In the SURPASS clinical trials, which evaluated tirzepatide in over 10,000 patients with type 2 diabetes, participants experienced average reductions in total cholesterol of approximately 5-10%, LDL-C reductions of 6-13%, and triglyceride reductions of 15-25%, depending on the dose administered. Modest increases in HDL-C were also observed in some patients. These improvements occurred alongside weight loss and improved glycaemic control, suggesting a comprehensive effect on metabolic health.
The mechanisms underlying these lipid improvements are likely multifactorial. Weight loss itself is an important modifier of lipid metabolism, reducing hepatic lipogenesis and improving insulin sensitivity. Additionally, GLP-1 receptor activation may influence lipid metabolism through effects on hepatic lipid handling and intestinal lipoprotein production. The reduction in visceral adiposity—a key driver of metabolic dysfunction—may further contribute to improved lipid profiles.
It is important to note that individual responses may vary, and some patients might experience different lipid changes based on their baseline metabolic status, concurrent medications, dietary habits, and genetic factors. However, the overall evidence supports tirzepatide as having neutral-to-beneficial effects on cholesterol levels rather than causing elevations. If cholesterol levels rise during tirzepatide treatment, alternative explanations should be explored, including dietary changes, medication non-adherence, or progression of underlying metabolic conditions.
Whilst tirzepatide typically improves lipid profiles, comprehensive cardiovascular risk management remains essential for patients with type 2 diabetes or obesity. NICE guideline NG28 for type 2 diabetes recommends regular monitoring of lipid levels as part of routine diabetes care, typically annually or more frequently if lipid-lowering therapy is being adjusted.
Patients taking tirzepatide should maintain heart-healthy lifestyle modifications that complement the medication's metabolic benefits:
Dietary modifications: Adopt a Mediterranean-style diet rich in fruits, vegetables, whole grains, legumes, nuts, and olive oil whilst limiting saturated fats, trans fats, and refined carbohydrates. Reducing dietary cholesterol and increasing soluble fibre intake can further support healthy lipid levels.
Regular physical activity: Aim for at least 150 minutes of moderate-intensity aerobic exercise weekly, as recommended by the UK Chief Medical Officers' Physical Activity Guidelines. Physical activity raises HDL cholesterol and improves overall cardiovascular fitness.
Weight management: Continue working towards weight loss goals, as sustained weight reduction provides ongoing benefits to lipid metabolism and cardiovascular risk.
Smoking cessation: If applicable, stopping smoking significantly improves HDL cholesterol and reduces overall cardiovascular risk.
Many patients with type 2 diabetes require statin therapy for primary or secondary cardiovascular prevention, regardless of their current cholesterol levels. No clinically significant interactions between tirzepatide and statins have been reported, though tirzepatide's effect on gastric emptying may affect absorption of some oral medications. These medications can be safely continued or initiated as clinically indicated, with appropriate monitoring.
Your healthcare team will assess your overall cardiovascular risk using tools such as QRISK3 and determine whether lipid-lowering therapy is appropriate based on your individual risk profile, not solely on cholesterol numbers. Regular blood tests will monitor both lipid levels and other metabolic parameters to ensure optimal management of your condition.
Whilst tirzepatide treatment is generally associated with improved lipid profiles, certain situations warrant discussion with your GP or diabetes specialist:
Routine monitoring: Ensure you attend scheduled blood test appointments, typically recommended annually for stable patients or more frequently if you have established cardiovascular disease or are initiating new treatments. These tests assess not only cholesterol levels but also HbA1c, renal function, and liver enzymes.
Unexpected lipid changes: If recent blood tests show elevated cholesterol levels whilst taking tirzepatide, contact your GP to discuss possible causes. This is particularly important if you have a personal or family history of familial hypercholesterolaemia or premature cardiovascular disease.
New cardiovascular symptoms: Seek prompt medical attention if you experience chest pain, unusual breathlessness, palpitations, or symptoms suggestive of transient ischaemic attack or stroke. Call 999 if you have symptoms of a heart attack or stroke. Whilst these are not direct effects of cholesterol changes, they require urgent assessment.
Medication concerns: If you are prescribed statin therapy alongside tirzepatide and experience muscle pain, weakness, or dark urine, contact your GP promptly as these may indicate statin-related myopathy, though this is uncommon.
Lifestyle and dietary guidance: Request referral to a dietitian or diabetes educator if you need support optimising your diet for both diabetes management and cardiovascular health. Many NHS diabetes services offer structured education programmes that address nutrition, physical activity, and medication management.
Pre-existing lipid disorders: If you have a known lipid disorder or are already taking multiple lipid-lowering medications, discuss with your specialist how tirzepatide fits into your overall treatment plan and whether medication adjustments might be beneficial as your weight and metabolic health improve.
If you experience any suspected side effects from tirzepatide or other medications, report them via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Clinical evidence from the SURPASS trials indicates that tirzepatide typically improves rather than raises cholesterol levels, with most patients experiencing reductions in total cholesterol, LDL-C, and triglycerides. If cholesterol rises during treatment, alternative causes should be investigated.
NICE guidance recommends annual lipid monitoring for stable patients with type 2 diabetes, though more frequent testing may be appropriate if you have cardiovascular disease or are adjusting lipid-lowering therapy.
Yes, statins can be safely taken with tirzepatide, and no clinically significant interactions have been reported. Many patients with type 2 diabetes require statin therapy for cardiovascular protection regardless of current cholesterol levels.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.