Does tirzepatide cause sleeplessness? Tirzepatide is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus and weight management. Sleeplessness is not listed as a common adverse effect in the Summary of Product Characteristics or clinical trial data. Whilst sleep disturbances may occur indirectly through gastrointestinal symptoms, metabolic changes, or lifestyle adjustments during treatment, no direct causal link between tirzepatide and primary insomnia has been established. Patients experiencing persistent sleep problems should seek comprehensive clinical assessment to identify contributing factors and determine appropriate management strategies.
Quick Answer: Tirzepatide does not directly cause sleeplessness as a recognised adverse effect, though sleep disturbances may occur indirectly through gastrointestinal symptoms or metabolic changes.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereThe most frequently documented adverse effects of tirzepatide include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and decreased appetite, which occur in a significant proportion of patients, particularly during dose escalation. Sleep-related complaints, whilst not formally classified as common side effects, may occur indirectly as a consequence of these gastrointestinal disturbances or other metabolic changes associated with treatment. There is no official link established between tirzepatide and primary insomnia in the published literature or regulatory documentation.
It is important to recognise that sleep disturbances can arise from multiple factors, including the underlying condition being treated (type 2 diabetes or obesity), concurrent medications, lifestyle changes, or psychological factors such as anxiety about weight loss or glycaemic control. Patients experiencing persistent sleep problems should not assume a direct causal relationship with tirzepatide without thorough clinical assessment. A comprehensive evaluation by a healthcare professional is essential to identify contributing factors and determine appropriate management strategies.
If you suspect tirzepatide may be causing sleep disturbances, you can report this as a suspected adverse reaction via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
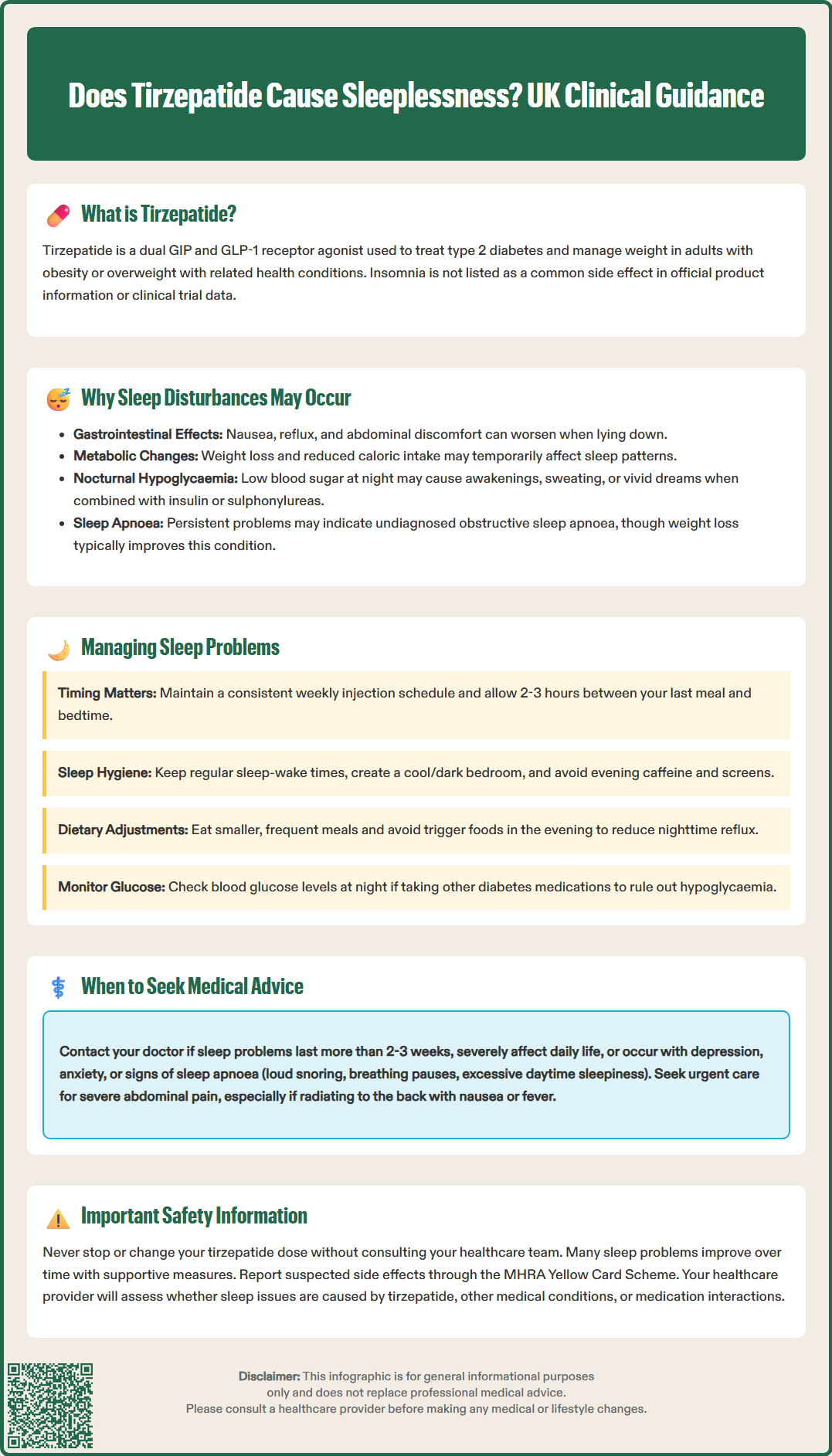
Several mechanisms may explain why some individuals experience sleep disturbances whilst taking tirzepatide, even though sleeplessness is not a recognised direct adverse effect of the medication. Understanding these potential contributing factors can help patients and clinicians address sleep problems more effectively.
Gastrointestinal adverse effects are the most common reason for treatment-related discomfort with tirzepatide. Nausea, abdominal discomfort, and reflux symptoms may worsen when lying down, potentially disrupting sleep onset or causing nocturnal awakenings. These symptoms are typically most pronounced during the initial weeks of treatment or following dose increases, as the body adjusts to the medication's effects on gastric emptying and satiety signalling.
Metabolic changes associated with significant weight loss and improved glycaemic control may potentially influence sleep patterns. Some patients may experience temporary sleep disruption during periods of active weight loss, though evidence for this specific to tirzepatide is limited. Additionally, changes in glucose metabolism may affect energy levels throughout the day, which could indirectly impact sleep patterns.
Dietary changes and reduced caloric intake, which often accompany tirzepatide treatment due to its appetite-suppressing effects, may contribute to sleep disturbances. Patients consuming significantly fewer calories or eating at different times may experience hunger-related awakenings or changes in their usual sleep-wake cycle.
Nocturnal hypoglycaemia may occur in patients taking concomitant insulin or sulfonylureas with tirzepatide, potentially causing night-time awakenings, sweating, or vivid dreams. The MHRA SmPC advises that when tirzepatide is used with insulin or a sulfonylurea, a reduction in the dose of these medications should be considered to reduce the risk of hypoglycaemia.
Anxiety about treatment outcomes, body image concerns, or adjustment to lifestyle modifications may also manifest as sleep difficulties in some individuals. It's worth noting that weight loss generally improves obstructive sleep apnoea over time, so assessment for this condition may be warranted if sleep symptoms persist.
If you are experiencing sleep disturbances whilst taking tirzepatide, several practical strategies may help improve sleep quality without necessarily requiring medication discontinuation. These approaches should be discussed with your healthcare team to ensure they are appropriate for your individual circumstances.
Optimising medication timing and dosing can be beneficial for some patients. Tirzepatide is administered once weekly via subcutaneous injection, and whilst there is no specific time of day recommended in the prescribing information, maintaining a consistent weekly schedule is important. If you miss a dose, follow the SmPC instructions: if less than 4 days have passed since the missed dose, administer as soon as possible; if more than 4 days have passed, skip the missed dose and administer the next dose on the regularly scheduled day. Some patients find that adjusting their injection day helps minimise sleep-related issues. If gastrointestinal symptoms are contributing to sleep problems, ensuring adequate time (2-3 hours) between your last meal and bedtime may reduce nocturnal discomfort. Your prescriber may also consider a slower dose escalation schedule or temporary dose reduction if symptoms are particularly troublesome.
Implementing good sleep hygiene practices is fundamental to managing sleep disturbances:
Maintain a consistent sleep-wake schedule, even on weekends
Create a comfortable sleep environment (cool, dark, and quiet)
Avoid caffeine and alcohol in the evening
Avoid large meals in the evening
Limit screen time for at least one hour before bed
Engage in regular physical activity, but not close to bedtime
Practice relaxation techniques such as deep breathing or meditation
Dietary modifications may also prove helpful. Eating smaller, more frequent meals throughout the day rather than large portions can reduce gastrointestinal discomfort. Avoiding foods that trigger reflux or nausea, particularly in the evening, may improve nocturnal symptoms. Staying well-hydrated throughout the day, whilst reducing fluid intake immediately before bed, can help manage both medication-related side effects and sleep quality.
Monitoring blood glucose levels, particularly if you are taking other diabetes medications alongside tirzepatide, can help identify whether nocturnal hypoglycaemia is contributing to sleep problems. Your diabetes care team may need to adjust doses of concurrent medications, especially insulin or sulfonylureas, to reduce this risk.
Whilst mild, transient sleep disturbances may resolve as your body adjusts to tirzepatide, certain situations warrant prompt medical attention. Understanding when to contact your GP or diabetes specialist nurse is important for ensuring safe and effective treatment.
You should seek medical advice if:
Sleep disturbances persist for more than two to three weeks despite implementing sleep hygiene measures
Insomnia is severe enough to significantly impair daytime functioning, concentration, or quality of life
You experience symptoms suggestive of sleep apnoea, such as loud snoring, witnessed breathing pauses, or excessive daytime sleepiness (particularly relevant as weight changes can affect sleep apnoea)
Sleep problems are accompanied by signs of depression, anxiety, or other mental health concerns
You suspect nocturnal hypoglycaemia (night sweats, vivid nightmares, morning headaches, or unexpectedly low morning glucose readings)
Gastrointestinal symptoms are severe, persistent, or worsening, particularly if accompanied by dehydration, inability to tolerate oral intake, or severe abdominal pain
Seek urgent medical attention if you experience:
Sudden severe, persistent abdominal pain (with or without vomiting), especially if radiating to the back, as this could indicate acute pancreatitis
Severe abdominal pain with nausea, vomiting, or fever, which might suggest gallbladder disease
Your healthcare provider will conduct a thorough assessment to determine whether sleep disturbances are related to tirzepatide, underlying medical conditions, or other factors. This evaluation may include reviewing your medication regimen, assessing for potential drug interactions, and screening for mood disorders or sleep disorders such as obstructive sleep apnoea. If sleep apnoea is suspected, your GP may refer you for assessment in line with NICE guidance.
NICE guidance recommends individualised treatment approaches for type 2 diabetes and obesity management. If sleep disturbances are significantly affecting your wellbeing, your clinician may consider adjusting your tirzepatide dose, temporarily pausing treatment, or exploring alternative therapeutic options. However, many patients find that sleep problems improve with time and supportive measures, allowing them to continue benefiting from tirzepatide's metabolic effects. Never discontinue or adjust your medication without consulting your healthcare team, as abrupt changes may affect your glycaemic control or weight management progress.
No, insomnia is not listed as a common adverse effect in the Summary of Product Characteristics or clinical trial data. Sleep disturbances may occur indirectly through gastrointestinal symptoms or metabolic changes, but no direct causal link has been established.
Implement good sleep hygiene practices, avoid large evening meals, and ensure adequate time between eating and bedtime. If sleep disturbances persist for more than two to three weeks or significantly impair daily functioning, seek medical advice for comprehensive assessment.
Nocturnal hypoglycaemia may occur when tirzepatide is used with insulin or sulfonylureas, potentially causing night-time awakenings and sweating. The MHRA advises considering dose reduction of these concomitant medications to reduce hypoglycaemia risk.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.