Wegovy (semaglutide 2.4 mg) is a GLP-1 receptor agonist licensed in the UK for weight management in adults with obesity or overweight with comorbidities. Whilst gastrointestinal side effects such as nausea and delayed gastric emptying are common with Wegovy, many patients wonder whether the medication can cause gastroparesis—a chronic condition characterised by abnormally slow stomach emptying. Understanding the distinction between expected pharmacological effects and true gastroparesis is essential for safe use. This article examines the evidence, explores gastrointestinal side effects, and provides guidance on when to seek medical advice whilst taking Wegovy.
Quick Answer: Wegovy does not cause gastroparesis as a recognised chronic condition, though its mechanism of delaying gastric emptying can produce symptoms resembling gastroparesis during treatment.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWegovy (semaglutide 2.4 mg) is a prescription medicine with UK marketing authorisation for weight management in adults with obesity or those who are overweight with weight-related health conditions. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which were originally developed for type 2 diabetes management.
The active ingredient, semaglutide, works by mimicking a naturally occurring hormone called GLP-1 that is released in the gut after eating. This mechanism produces several effects that support weight loss:
Appetite suppression: Wegovy acts on receptors in the brain that regulate hunger, helping patients feel fuller for longer periods and reducing overall calorie intake.
Slowed gastric emptying: The medication delays how quickly food moves from the stomach into the small intestine, which contributes to prolonged feelings of satiety.
Improved glucose regulation: Although primarily used for weight management, semaglutide also helps regulate blood sugar levels by stimulating insulin secretion when glucose levels are elevated and suppressing inappropriate glucagon secretion.
Wegovy is administered as a once-weekly subcutaneous injection, typically in the abdomen, thigh, or upper arm. The dose is gradually increased over several weeks to minimise side effects and allow the body to adjust to the medication. It is important to understand that Wegovy is not a standalone solution—it must be used alongside a reduced-calorie diet and increased physical activity for optimal results. Wegovy became available in the UK in 2023, and its use on the NHS follows NICE guidance (TA875) which provides specific clinical criteria for eligible patients.
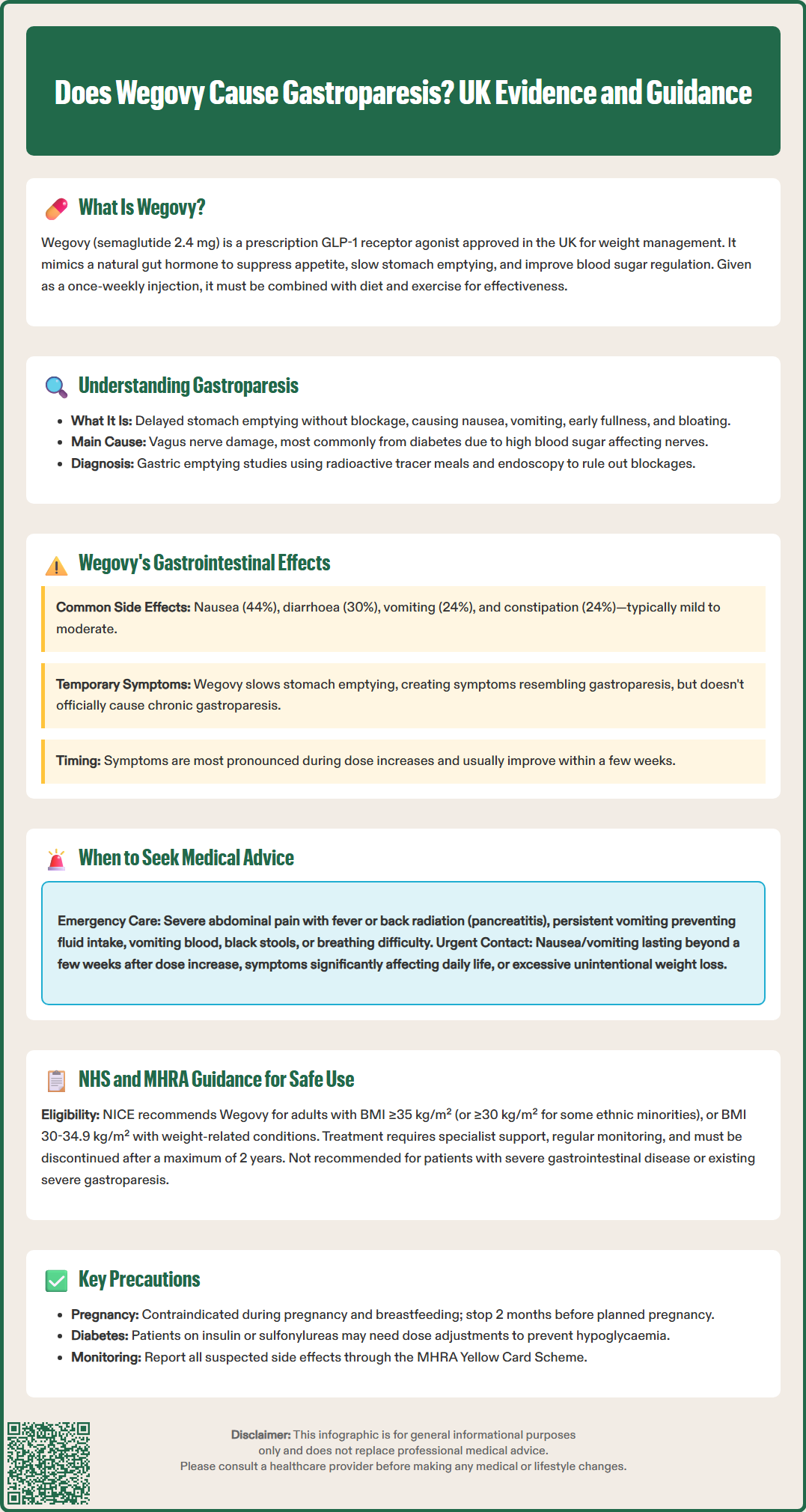
Gastroparesis is a chronic condition characterised by delayed gastric emptying without any mechanical obstruction. In this disorder, the stomach takes too long to empty its contents into the small intestine, leading to a range of uncomfortable and sometimes debilitating symptoms.
Common symptoms of gastroparesis include:
Persistent nausea and vomiting, particularly of undigested food
Early satiety (feeling full after eating only small amounts)
Abdominal bloating and discomfort
Upper abdominal pain
Heartburn or gastro-oesophageal reflux
Poor appetite and unintentional weight loss
Blood glucose fluctuations in people with diabetes
The condition occurs when the vagus nerve, which controls stomach muscle contractions, becomes damaged or stops functioning properly. Several underlying causes can lead to gastroparesis:
Diabetes mellitus is the most common identifiable cause, with prolonged high blood sugar levels damaging the vagus nerve over time. Post-surgical complications, particularly following stomach or oesophageal surgery, can disrupt normal gastric function. Certain medications, including opioid pain relievers, anticholinergics, and some antidepressants, may slow gastric emptying. Neurological conditions such as Parkinson's disease or multiple sclerosis can affect nerve signals to the stomach. In many cases, however, gastroparesis is classified as idiopathic, meaning no clear cause can be identified.
Diagnosis typically involves gastric emptying studies, where patients consume a meal containing a small amount of radioactive material, and imaging tracks how quickly the stomach empties. Endoscopy is usually performed to rule out mechanical obstruction. Patients with persistent unexplained nausea, vomiting, weight loss, or suspected diabetic gastroparesis should be referred to a gastroenterologist for specialist assessment.
Gastrointestinal side effects are the most commonly reported adverse reactions with Wegovy, affecting a significant proportion of patients, particularly during the initial dose escalation phase. These effects are directly related to the medication's mechanism of slowing gastric emptying.
The most frequent gastrointestinal side effects include:
Nausea (reported in up to 44% of patients in clinical trials)
Diarrhoea (affecting approximately 30% of users)
Vomiting (experienced by around 24% of patients)
Constipation (occurring in roughly 24% of individuals)
Abdominal pain and discomfort
Dyspepsia (indigestion)
These symptoms are typically mild to moderate in severity and tend to improve over time as the body adjusts to the medication. Most patients find that side effects are most pronounced when the dose is increased and gradually diminish within a few weeks.
Regarding the specific question of whether Wegovy causes gastroparesis, there is no official established causal link between semaglutide and the development of true gastroparesis as a chronic condition. However, the medication's pharmacological action of delaying gastric emptying can produce symptoms that may resemble gastroparesis during treatment. This is an expected pharmacological effect rather than a pathological disease state.
The UK product information for Wegovy acknowledges gastrointestinal adverse reactions but does not list gastroparesis as a recognised side effect. Post-marketing surveillance has identified rare cases of ileus (intestinal obstruction), which may be related to severe delayed gastric emptying. According to the UK SmPC, Wegovy is not recommended in patients with severe gastrointestinal disease, including severe gastroparesis, as it may worsen existing symptoms. The gradual dose titration schedule is specifically designed to minimise gastrointestinal tolerability issues.
While most side effects of Wegovy are manageable and resolve with time, certain symptoms warrant prompt medical attention. Patients should be aware of red flag symptoms that may indicate serious complications requiring urgent assessment.
Seek immediate medical attention if you experience:
Severe, persistent abdominal pain, particularly if accompanied by fever or radiating to the back. This could indicate pancreatitis—a rare but serious side effect. If pancreatitis is suspected, stop taking Wegovy immediately and seek urgent medical care.
Persistent vomiting that prevents you from keeping down food or fluids, leading to dehydration
Signs of dehydration, including dark urine, dizziness, reduced urination, or extreme thirst, which may lead to acute kidney injury
Vomiting blood or passing black, tarry stools, which may suggest gastrointestinal bleeding
Severe allergic reactions, such as difficulty breathing, facial swelling, or widespread rash (call 999 or go to A&E immediately)
Signs of intestinal obstruction: progressive abdominal distension, severe constipation, inability to pass gas, persistent vomiting
Contact your GP or prescribing clinician if:
Nausea or vomiting persists beyond the first few weeks after a dose increase
You experience significant unintentional weight loss beyond your target or cannot maintain adequate nutrition
Gastrointestinal symptoms significantly impact your quality of life or daily functioning
You develop new or worsening symptoms of gastroparesis, particularly if you have diabetes
You notice changes in blood glucose control (for patients with diabetes)
You experience symptoms of gallbladder problems, such as pain in the upper right abdomen, yellowing of skin or eyes, or fever
Patients should also inform their healthcare provider if they are taking other medications that affect gastric emptying. If you have upcoming surgical procedures, discuss Wegovy with your surgical and anaesthetic team, as specific perioperative management may be required.
Suspected side effects should be reported via the MHRA Yellow Card Scheme (https://yellowcard.mhra.gov.uk), which helps monitor medication safety.
The safe and effective use of Wegovy requires adherence to evidence-based prescribing guidelines and ongoing monitoring by healthcare professionals. NICE guidance (TA875, published March 2023) provides clear criteria for Wegovy use within the NHS.
NICE recommends Wegovy for adults who:
Have a body mass index (BMI) of 35 kg/m² or more (or 30 kg/m² or more for people from some minority ethnic groups), or
Have a BMI of 30–34.9 kg/m² (or 27.5–29.9 kg/m² for people from some minority ethnic groups) with at least one weight-related comorbidity (such as hypertension, type 2 diabetes, obstructive sleep apnoea, or cardiovascular disease)
Are participating in a specialist weight management service that provides dietary advice, physical activity support, and behavioural interventions
Treatment should be discontinued after a maximum of 2 years within the specialist weight management service. Regular review appointments are essential to monitor progress, assess tolerability, and provide ongoing lifestyle support.
Important safety considerations from the UK product information:
Contraindications: Wegovy is contraindicated in patients with hypersensitivity to semaglutide or any of the excipients, and during pregnancy.
Pregnancy and breastfeeding: Wegovy is not recommended during pregnancy or breastfeeding. Women of childbearing potential should use effective contraception, and the medication should be discontinued at least 2 months before a planned pregnancy.
Drug interactions: Wegovy may affect the absorption of medicines requiring rapid gastrointestinal absorption or with a narrow therapeutic index. INR monitoring is advised when used with warfarin or other coumarins. Semaglutide has no clinically relevant effect on combined oral contraceptives.
Special warnings: Caution is advised in patients with diabetic retinopathy, as rapid improvement in glucose control may be associated with temporary worsening of retinopathy. There is also an increased risk of cholelithiasis and cholecystitis.
Hypoglycaemia risk: When used alongside insulin or sulfonylureas in patients with diabetes, dose adjustments of these medications may be necessary to reduce hypoglycaemia risk.
Patients should receive proper training on injection technique, needle disposal, and storage requirements (Wegovy must be refrigerated before first use). Healthcare professionals should provide clear written information about expected side effects and when to seek help, ensuring patients feel supported throughout their treatment journey.
There is no established evidence that Wegovy causes permanent gastroparesis. Whilst the medication slows gastric emptying as part of its mechanism, this is a reversible pharmacological effect rather than a chronic disease state, and symptoms typically improve when treatment is stopped.
If you experience persistent vomiting that prevents you from keeping down food or fluids, or severe abdominal pain, contact your GP or prescribing clinician promptly. Severe symptoms may indicate complications requiring medical assessment, and dose adjustment or treatment discontinuation may be necessary.
Wegovy is not recommended for patients with severe gastroparesis, as its mechanism of delaying gastric emptying may worsen existing symptoms. Patients with pre-existing gastrointestinal conditions should discuss their suitability for Wegovy with their healthcare provider before starting treatment.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.