LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Does Wegovy help with insulin resistance? This question is increasingly relevant as obesity rates rise and metabolic health concerns grow across the UK. Wegovy (semaglutide 2.4 mg) is a once-weekly injection licensed for weight management in adults with obesity or overweight with comorbidities. Whilst not specifically licensed to treat insulin resistance, clinical evidence demonstrates that Wegovy does improve insulin sensitivity markers—primarily through substantial weight loss rather than direct insulin-sensitising effects. Understanding how this GLP-1 receptor agonist works, who might benefit, and its limitations is essential for informed decision-making about metabolic health management.
Quick Answer: Wegovy does improve insulin resistance markers, primarily through facilitating substantial weight loss rather than direct insulin-sensitising effects independent of weight reduction.
Wegovy (semaglutide 2.4 mg) is a once-weekly subcutaneous injection licensed in the UK for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. However, NHS funding through NICE guidance (TA875) applies stricter criteria, requiring BMI ≥35 kg/m² or BMI 30–34.9 kg/m² in exceptional circumstances via specialist weight management services.
Wegovy belongs to a class of medicines called glucagon-like peptide-1 (GLP-1) receptor agonists, which mimic the action of the naturally occurring hormone GLP-1.
GLP-1 is released from the intestine in response to food intake and plays several important roles in glucose metabolism and appetite regulation. Wegovy works by binding to GLP-1 receptors in multiple tissues throughout the body, including the pancreas, brain, and gastrointestinal tract. This activation triggers several physiological responses that contribute to weight loss and metabolic improvements.
Key mechanisms of action include:
Appetite suppression – Wegovy acts on receptors in the hypothalamus to reduce hunger and increase feelings of fullness (satiety)
Delayed gastric emptying – The medication slows the rate at which food leaves the stomach, prolonging satiety after meals
Enhanced insulin secretion – In the presence of elevated blood glucose, Wegovy stimulates the pancreas to release insulin more effectively
Reduced glucagon secretion – The drug suppresses the release of glucagon, a hormone that raises blood glucose levels
These combined effects lead to reduced calorie intake and significant weight loss, typically 10-15% of initial body weight over 68 weeks in clinical trials. The medication is approved by the Medicines and Healthcare products Regulatory Agency (MHRA) and recommended by NICE for specific patient groups meeting eligibility criteria.
Insulin resistance is a metabolic condition in which the body's cells become less responsive to insulin, the hormone responsible for facilitating glucose uptake from the bloodstream. This forces the pancreas to produce increasingly higher amounts of insulin to maintain normal blood glucose levels, a state known as hyperinsulinaemia. Over time, insulin resistance can progress to non-diabetic hyperglycaemia (also called prediabetes) and type 2 diabetes if the pancreas can no longer compensate.
Excess body weight, particularly visceral adiposity (fat stored around internal organs), is one of the primary drivers of insulin resistance. Adipose tissue, especially when inflamed, releases various substances including free fatty acids and pro-inflammatory cytokines (such as TNF-alpha and IL-6) that interfere with insulin signalling pathways in muscle, liver, and fat cells. This creates a vicious cycle where insulin resistance promotes further weight gain, and excess weight worsens insulin resistance.
Weight loss has been consistently shown to improve insulin sensitivity through multiple mechanisms. Even modest weight reduction of 5-10% can lead to meaningful metabolic improvements. When body weight decreases, several beneficial changes occur:
Reduction in visceral fat and associated inflammation
Decreased circulating free fatty acids that impair insulin signalling
Improved function of insulin receptors on cell surfaces
Reduced burden on pancreatic beta cells, allowing better insulin production
Lower levels of inflammatory markers throughout the body
The relationship between obesity and insulin resistance is well established in medical literature, with weight management forming a cornerstone of treatment strategies recommended by NICE (NG28) for preventing and managing type 2 diabetes. This fundamental connection provides the biological rationale for investigating whether weight-loss medications like Wegovy might offer benefits beyond simple weight reduction.
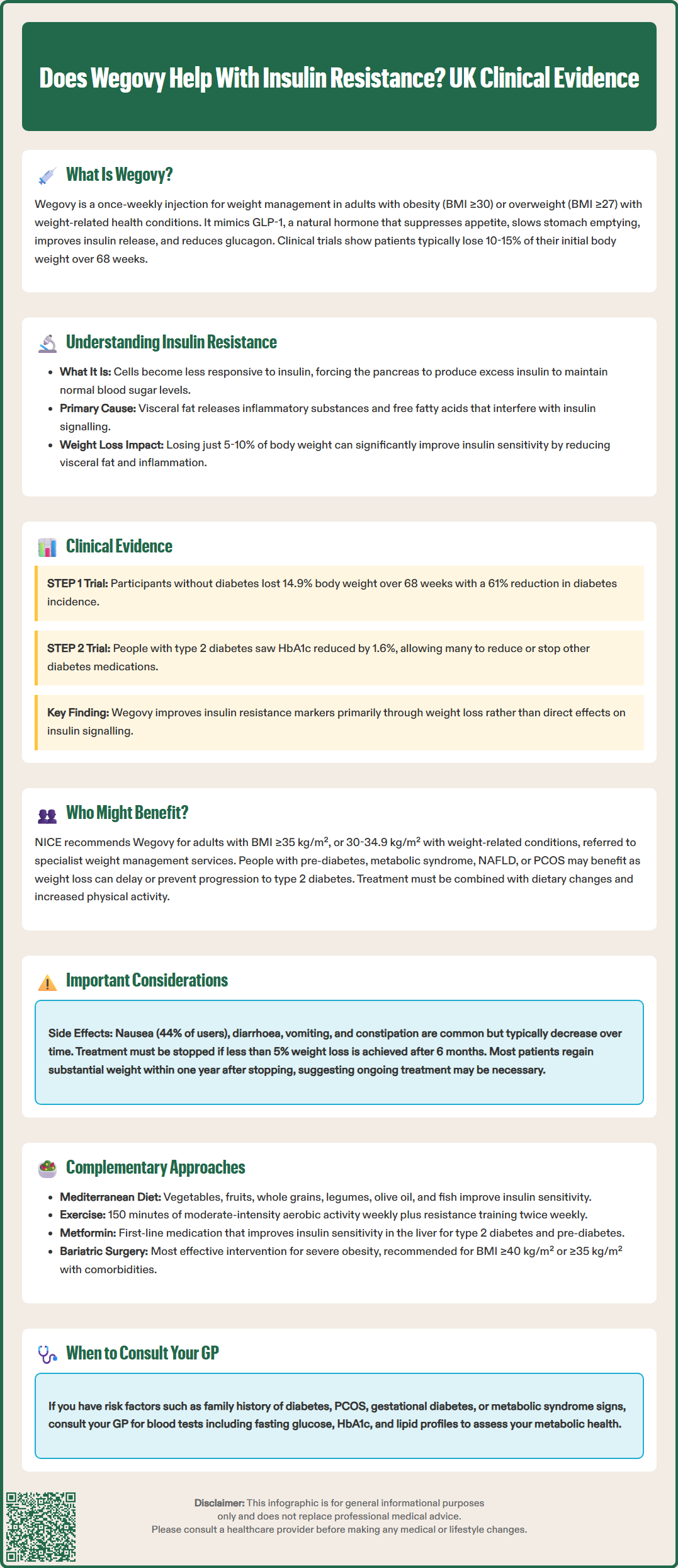
Clinical trial data demonstrates that Wegovy does improve markers of insulin sensitivity, though it's important to understand that these benefits appear to be primarily mediated through weight loss rather than direct insulin-sensitising effects independent of weight reduction. It should be noted that semaglutide is not specifically licensed to treat insulin resistance.
The landmark STEP (Semaglutide Treatment Effect in People with obesity) clinical trial programme provides the most robust evidence. In the STEP 1 trial, participants without diabetes who received Wegovy achieved an average weight loss of 14.9% compared to 2.4% with placebo over 68 weeks. Importantly, improvements in insulin resistance markers accompanied this weight loss, including:
Significant reductions in fasting insulin levels
Improvements in HOMA-IR (Homeostatic Model Assessment for Insulin Resistance), a validated research measure of insulin sensitivity
Decreased HbA1c levels, even in participants without diabetes
Favourable changes in lipid profiles, including reduced triglycerides
A post-hoc exploratory analysis of the STEP 1 trial suggested a 61% reduction in diabetes incidence compared to placebo, though this finding has not been specifically endorsed by UK regulatory bodies.
In the STEP 2 trial, which specifically enrolled participants with type 2 diabetes, semaglutide 2.4 mg led to substantial improvements in glycaemic control, with HbA1c reductions of approximately 1.6% from baseline. Many participants were able to reduce or discontinue other diabetes medications.
However, research suggests that the insulin sensitivity improvements are largely proportional to the degree of weight loss achieved. Studies comparing GLP-1 receptor agonists to other weight-loss interventions (such as bariatric surgery or intensive lifestyle modification) show similar metabolic improvements when equivalent weight loss is achieved. This indicates that whilst Wegovy is highly effective at facilitating weight loss, the improvements in insulin resistance are predominantly a consequence of reduced adiposity rather than a unique pharmacological effect on insulin signalling pathways independent of weight change.
NICE guidance (TA875) provides specific criteria for Wegovy prescription within the NHS, focusing on individuals who would benefit most from medically supervised weight loss. According to NICE, Wegovy is recommended for adults with a BMI of at least 35 kg/m², or between 30–34.9 kg/m² with weight-related comorbidities, and referred to a specialist weight management service (tier 3). The medication may be particularly valuable for people with insulin resistance in the following circumstances:
Individuals with non-diabetic hyperglycaemia or metabolic syndrome – Those with impaired fasting glucose, impaired glucose tolerance, or metabolic syndrome (a cluster of conditions including central obesity, raised blood pressure, dyslipidaemia, and insulin resistance) may benefit significantly. Weight loss achieved with Wegovy may help delay or prevent progression to type 2 diabetes, as demonstrated in the STEP programme.
People with type 2 diabetes and obesity – Wegovy is licensed for weight management in this population and can provide dual benefits of weight reduction and improved glycaemic control. However, it's worth noting that semaglutide is also available at lower doses (up to 1 mg) as Ozempic, specifically licensed for type 2 diabetes treatment, which may be more appropriate depending on individual circumstances.
Those with obesity-related complications – Individuals meeting the NICE BMI criteria who have struggled to achieve weight loss through lifestyle interventions alone may be suitable candidates. Insulin resistance often coexists with other conditions such as non-alcoholic fatty liver disease (NAFLD), polycystic ovary syndrome (PCOS), and obstructive sleep apnoea, all of which may improve with weight reduction.
Important eligibility considerations:
NICE recommends Wegovy only after dietary and exercise interventions have been tried
Treatment should be discontinued if less than 5% weight loss is achieved after 6 months
NICE recommends stopping treatment after 2 years unless a specialist review indicates exceptional circumstances for continued use
The medication is intended as an adjunct to, not a replacement for, lifestyle modification
Prescribing decisions should be made by specialists or GPs with appropriate training in obesity management
Whilst Wegovy can be an effective tool for weight management and associated metabolic improvements, several important considerations and limitations must be understood by both patients and healthcare professionals.
Common adverse effects are predominantly gastrointestinal and include nausea (experienced by approximately 44% of users), diarrhoea, vomiting, constipation, and abdominal pain. These effects are typically most pronounced during dose escalation and often diminish over time. To minimise side effects, Wegovy is initiated at a low dose (0.25 mg weekly) and gradually increased over 16-20 weeks to the maintenance dose of 2.4 mg.
Contraindications and cautions include:
Personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2
Severe gastrointestinal disease, including gastroparesis
History of pancreatitis (use with caution)
Pregnancy and breastfeeding (contraindicated)
Diabetic retinopathy (requires monitoring in people with diabetes)
Risk of hypoglycaemia when used with sulfonylureas or insulin (may require dose adjustment of these medications)
Patients should be advised to seek urgent medical attention if they experience severe or persistent abdominal pain which could indicate pancreatitis. Any suspected adverse reactions should be reported via the MHRA Yellow Card Scheme.
Weight regain after discontinuation is a significant limitation. Clinical trial data shows that most individuals regain a substantial portion of lost weight within one year of stopping Wegovy. This raises important questions about the duration of treatment and long-term sustainability. Current evidence suggests that ongoing treatment may be necessary to maintain weight loss and associated metabolic benefits, though long-term safety data beyond two years remains limited.
Cost and accessibility represent practical barriers. NHS availability is restricted according to NICE criteria. Many patients may not meet eligibility requirements or may face long waiting times for specialist assessment.
It is not a standalone solution – Wegovy works best when combined with dietary modification, increased physical activity, and behavioural support. Patients should be counselled that medication alone, without lifestyle changes, is unlikely to produce optimal or sustained results.
Managing insulin resistance requires a comprehensive approach, with multiple evidence-based strategies available beyond pharmacological interventions like Wegovy.
Lifestyle modification remains the foundation of insulin resistance management and should be attempted before or alongside any medication. Dietary approaches with strong evidence include:
Mediterranean diet – Rich in vegetables, fruits, whole grains, legumes, nuts, and olive oil, with moderate fish and poultry consumption. This pattern has been shown to improve insulin sensitivity and reduce diabetes risk.
Low glycaemic index (GI) foods – Some evidence suggests choosing foods that cause slower, more gradual rises in blood glucose may help reduce insulin demand, though the quality of carbohydrates is generally more important than GI alone.
Calorie restriction – Even without specific macronutrient manipulation, reducing overall energy intake to achieve weight loss improves insulin sensitivity.
Reduced refined carbohydrates and added sugars – Limiting processed foods, sugary beverages, and refined grains helps reduce insulin spikes.
Physical activity is equally important, with NICE recommending at least 150 minutes of moderate-intensity aerobic activity weekly, plus resistance training twice weekly. Exercise improves insulin sensitivity through multiple mechanisms, including increased glucose uptake by muscles, reduced visceral fat, and improved mitochondrial function.
Alternative pharmacological options for weight management and metabolic improvement include:
Metformin – First-line medication for type 2 diabetes that improves insulin sensitivity, particularly in the liver. Also used for non-diabetic hyperglycaemia and PCOS as per NICE guidance (NG28).
Orlistat – A lipase inhibitor that reduces fat absorption, available over-the-counter or on prescription.
Other GLP-1 receptor agonists – Including liraglutide (Saxenda for weight management) and dulaglutide.
Bariatric surgery represents the most effective intervention for severe obesity and insulin resistance, with procedures like gastric bypass producing dramatic improvements in insulin sensitivity, often before significant weight loss occurs. NICE recommends considering surgery for people with BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities including type 2 diabetes (NICE CG189).
When to seek medical advice: Individuals concerned about insulin resistance should consult their GP, particularly if they have risk factors such as family history of diabetes, PCOS, gestational diabetes, or signs of metabolic syndrome. Blood tests including fasting glucose, HbA1c, and lipid profiles can assess metabolic health and guide appropriate interventions.
Wegovy is available on the NHS only for weight management in adults meeting specific NICE criteria (BMI ≥35 kg/m² or 30–34.9 kg/m² with comorbidities) through specialist weight management services. It is not specifically licensed or funded for treating insulin resistance alone, though metabolic improvements may occur with weight loss.
Improvements in insulin sensitivity markers typically correlate with weight loss progression. Clinical trials show measurable changes in fasting insulin and HbA1c within 3–6 months, with maximum benefits observed after 12–18 months of treatment when weight loss plateaus.
Most individuals regain a substantial portion of lost weight within one year of discontinuing Wegovy, which typically reverses the metabolic improvements including insulin sensitivity. Ongoing lifestyle modification is essential to maintain benefits after stopping treatment.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.