Does Wegovy cause IBS? This is a common concern for patients considering or taking this weight management medication. Wegovy (semaglutide 2.4 mg) is a GLP-1 receptor agonist licensed in the UK for obesity treatment, approved by the MHRA and recommended by NICE in specific circumstances. Whilst Wegovy frequently causes gastrointestinal side effects such as nausea, diarrhoea, and abdominal discomfort, there is no evidence that it directly causes irritable bowel syndrome (IBS) as a diagnosed condition. Understanding the distinction between medication-related digestive symptoms and IBS is essential for patients and clinicians managing treatment expectations and tolerability.
Quick Answer: Wegovy does not cause irritable bowel syndrome (IBS) as a diagnosed condition, though it commonly produces gastrointestinal side effects that may resemble IBS symptoms.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities. Approved by the MHRA and recommended by NICE (TA875) in specific circumstances, Wegovy works by mimicking the natural hormone GLP-1, which regulates appetite and food intake.
The mechanism of action of Wegovy directly involves the gastrointestinal system. GLP-1 receptors are found throughout the gut, and when activated by semaglutide, they slow gastric emptying—the rate at which food leaves the stomach and enters the small intestine. This delayed emptying contributes to increased satiety and reduced calorie intake, which supports weight loss. However, this same mechanism also explains why gastrointestinal side effects are among the most commonly reported adverse reactions to Wegovy.
It is important to understand that whilst Wegovy frequently causes digestive symptoms, there is no evidence establishing that Wegovy directly causes irritable bowel syndrome (IBS). IBS is not listed as an adverse reaction in the MHRA/EMC Summary of Product Characteristics (SmPC) for Wegovy. IBS is a chronic functional gastrointestinal disorder characterised by recurrent abdominal pain associated with altered bowel habits, typically diagnosed using the Rome IV criteria (symptom onset at least 6 months before diagnosis, with abdominal pain at least 1 day/week in the last 3 months, plus related stool/defecation criteria). The gastrointestinal effects of Wegovy are generally considered acute pharmacological responses rather than the development of a chronic functional disorder.
Notably, the Wegovy SmPC includes cautions regarding use in patients with severe gastrointestinal disease, including severe gastroparesis. The overlap in symptoms between Wegovy's side effects and IBS can understandably cause concern for patients, making it essential to distinguish between medication-related effects and pre-existing or newly diagnosed IBS.
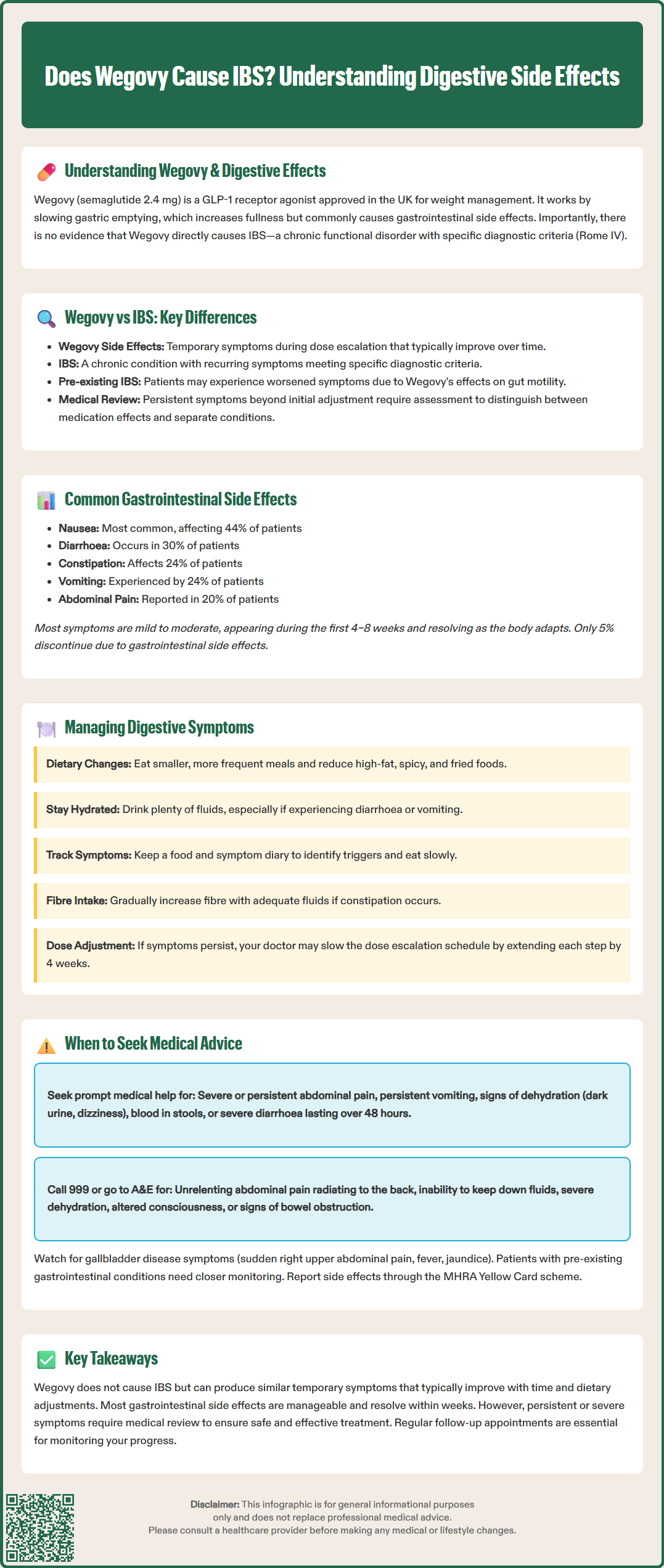
Whilst Wegovy does not cause IBS as a diagnosed condition, many patients experience gastrointestinal symptoms that closely resemble those seen in IBS. These include abdominal pain, bloating, altered bowel habits (diarrhoea or constipation), and abdominal discomfort. The similarity in symptom presentation can make it challenging to differentiate between medication side effects and underlying functional bowel disorders.
Clinical trial data from the STEP (Semaglutide Treatment Effect in People with obesity) programme demonstrated that gastrointestinal adverse events were reported in a substantial proportion of participants. According to the EMA European Public Assessment Report (EPAR) for Wegovy, these symptoms typically emerged during dose escalation and often diminished over time as patients developed tolerance to the medication. The transient nature of these effects differs from IBS, which is characterised by chronic, recurring symptoms meeting the Rome IV diagnostic criteria.
For patients with pre-existing IBS, starting Wegovy may potentially exacerbate their baseline symptoms, particularly during the initial treatment phase. The slowed gastric emptying and altered gut motility caused by semaglutide may interact with the already dysregulated gut function characteristic of IBS. However, systematic evidence examining this interaction remains limited, and clinical experience varies considerably between individuals.
If IBS-like symptoms persist beyond the dose escalation period or after dose stabilisation, clinical review is advisable to determine whether these represent medication side effects or a separate condition requiring diagnosis and management. It is also worth noting that weight loss itself—regardless of the method—can influence bowel habits and gastrointestinal symptoms. Dietary changes often accompany Wegovy treatment, and these modifications may independently affect digestive function. Therefore, attributing new or worsening bowel symptoms solely to Wegovy requires careful clinical assessment, considering the patient's complete medical history, dietary patterns, and any pre-existing gastrointestinal conditions.
According to the MHRA/EMC SmPC for Wegovy, the most frequently reported gastrointestinal side effects include:
Nausea – the most common adverse effect, affecting approximately 44% of patients in clinical trials, typically most pronounced during dose escalation
Diarrhoea – reported in around 30% of patients, ranging from mild to moderate severity
Constipation – affecting approximately 24% of patients, related to slowed gut transit
Vomiting – occurring in roughly 24% of patients, often associated with nausea
Abdominal pain or discomfort – reported by approximately 20% of patients
Dyspepsia (indigestion) – affecting around 9% of patients
Bloating and flatulence – commonly reported but less precisely quantified in trials
These side effects are dose-dependent, meaning they tend to be more pronounced at higher doses and during the escalation phase. The standard Wegovy dosing schedule involves gradual increases over 16–20 weeks, specifically designed to improve gastrointestinal tolerability. Most patients experience the greatest symptom burden during the first 4–8 weeks of treatment.
The majority of gastrointestinal adverse effects are mild to moderate in severity and tend to resolve or significantly improve within several weeks as the body adapts to the medication. In clinical trials, discontinuation due to gastrointestinal side effects occurred in approximately 5% of patients receiving Wegovy compared to 1% with placebo (as reported in the SmPC).
Importantly, these effects are considered pharmacological consequences of GLP-1 receptor activation rather than signs of organ damage or serious pathology. However, the SmPC does include warnings about more serious potential complications including pancreatitis, cholelithiasis/cholecystitis, and dehydration potentially leading to acute kidney injury. Persistent or severe symptoms warrant medical review to exclude these complications and assess whether treatment continuation is appropriate for the individual patient.
Effective management of gastrointestinal symptoms can significantly improve treatment adherence and patient quality of life whilst taking Wegovy. Dietary modifications represent the first-line approach to minimising digestive discomfort:
Eat smaller, more frequent meals rather than large portions, which can overwhelm the already-slowed digestive system
Reduce intake of high-fat foods, as these delay gastric emptying further and may exacerbate nausea
Avoid spicy, heavily seasoned, or fried foods that may irritate the gastrointestinal tract
Stay well hydrated, particularly if experiencing diarrhoea or vomiting
Increase dietary fibre gradually if constipation is problematic, alongside adequate fluid intake
Identify and avoid personal trigger foods that worsen symptoms
Practical lifestyle strategies can also help:
Take Wegovy at a consistent time each week; the time of day does not affect efficacy
Avoid lying down immediately after eating
Eat slowly and chew food thoroughly
Consider keeping a food and symptom diary to identify patterns
For persistent nausea, anti-emetic medications may be prescribed short-term under medical supervision. The MHRA has issued safety restrictions for commonly used antiemetics: domperidone should only be used for nausea/vomiting, at the lowest effective dose with cardiac monitoring due to QT prolongation risk; metoclopramide use should be limited to a maximum of 5 days. Alternative antiemetics such as cyclizine, prochlorperazine or ondansetron (noting potential constipation) may be considered by prescribers. For constipation, osmotic laxatives like macrogol are generally preferred over stimulant laxatives, as recommended in the BNF.
If symptoms remain troublesome despite these measures, the Wegovy SmPC advises that slowing the dose escalation schedule may be appropriate. Each dose step can be extended by 4 weeks if needed, or maintenance at 1.7 mg considered if 2.4 mg is not tolerated. Never adjust your Wegovy dose without medical guidance, as this may affect both efficacy and safety.
Whilst mild gastrointestinal symptoms are expected with Wegovy, certain presentations require prompt medical assessment. Contact your GP or prescribing clinician if you experience:
Severe or persistent abdominal pain, particularly if sharp, localised, or worsening, which could indicate pancreatitis or other serious conditions
Sudden or persistent right upper abdominal pain, fever, jaundice, pale stools or dark urine which may indicate gallbladder disease (cholelithiasis or cholecystitis)
Persistent vomiting that prevents adequate fluid or medication intake, risking dehydration
Signs of dehydration including dark urine, dizziness, reduced urination, or extreme thirst, which may lead to acute kidney injury in at-risk patients
Blood in stools (either bright red or dark, tarry stools) or persistent rectal bleeding
Severe diarrhoea lasting more than 48 hours or accompanied by fever
Unexplained weight loss beyond expected therapeutic effects or loss of appetite that seems excessive
New or significantly worsened symptoms in patients with pre-existing IBS or inflammatory bowel disease
Seek immediate medical attention (call 999 or attend A&E) if you develop:
Severe, unrelenting abdominal pain, especially if radiating to the back
Persistent vomiting with inability to keep down fluids
Signs of severe dehydration or altered consciousness
Symptoms suggestive of bowel obstruction (severe bloating, inability to pass stool or wind, vomiting)
For patients with pre-existing gastrointestinal conditions, including diagnosed IBS, Crohn's disease, ulcerative colitis, or gastroparesis, closer monitoring is advisable when starting Wegovy. NICE guidance (TA875) emphasises individualised assessment of suitability for GLP-1 receptor agonists, and your clinician should consider your complete medical history when prescribing.
If you believe you have experienced side effects from Wegovy, you can report these through the MHRA Yellow Card scheme (website or app). Regular follow-up appointments allow for ongoing assessment of both treatment efficacy and tolerability, ensuring that Wegovy remains an appropriate and safe option for your weight management journey.
Wegovy can cause gastrointestinal symptoms such as abdominal pain, bloating, and altered bowel habits that resemble IBS, but these are typically transient medication side effects rather than the development of chronic IBS. If symptoms persist beyond dose escalation, clinical review is needed to distinguish between medication effects and a separate functional bowel disorder.
Most gastrointestinal side effects from Wegovy are most pronounced during the first 4–8 weeks of treatment and during dose escalation. The majority of symptoms are mild to moderate and tend to resolve or significantly improve within several weeks as the body adapts to the medication.
Do not stop Wegovy without medical guidance. Mild digestive symptoms are common and often manageable with dietary modifications and lifestyle strategies. However, severe or persistent abdominal pain, persistent vomiting, signs of dehydration, blood in stools, or symptoms suggestive of pancreatitis or gallbladder disease require prompt medical assessment.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.