
Fatigue is a recognised side effect of Wegovy (semaglutide 2.4 mg), a GLP-1 receptor agonist licensed in the UK for weight management. Many patients wonder whether Wegovy fatigue goes away with continued treatment. Whilst tiredness is common during initial dose escalation, individual experiences vary considerably. For most patients, fatigue diminishes as the body adapts to reduced caloric intake and metabolic changes, typically improving within weeks to months. However, persistent fatigue warrants medical review to exclude nutritional deficiencies, dehydration, or other contributing factors. Understanding the causes and implementing practical management strategies can help maintain energy levels whilst benefiting from Wegovy's therapeutic effects.
Quick Answer: Wegovy-related fatigue typically improves as the body adapts to treatment, often diminishing within weeks to months, though individual experiences vary and persistent tiredness requires medical evaluation.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities. Whilst the Medicines and Healthcare products Regulatory Agency (MHRA) approved Wegovy based on robust clinical trial data, patients may experience various side effects during treatment, with fatigue being a recognised concern.
Fatigue and tiredness are listed as common adverse reactions in the UK Summary of Product Characteristics (SmPC) and Patient Information Leaflet for Wegovy, alongside the more frequently discussed gastrointestinal effects such as nausea, diarrhoea, vomiting, and constipation. Tiredness and reduced energy levels may occur when initiating or escalating Wegovy doses. It is important to distinguish between direct drug-related fatigue and tiredness resulting from the medication's intended effects—namely reduced caloric intake and metabolic changes associated with weight loss.
Understanding the context of fatigue is essential for both patients and healthcare professionals. Fatigue may manifest as generalised tiredness, reduced physical stamina, or difficulty concentrating. The experience varies considerably between individuals, with some reporting mild symptoms that resolve spontaneously, whilst others find fatigue more persistent or troublesome. Recognising that fatigue can have multiple contributing factors—including dietary changes, dehydration, electrolyte imbalances, or concurrent medical conditions—is crucial for appropriate assessment and management. For patients also taking insulin or sulfonylureas, fatigue may sometimes reflect hypoglycaemia, requiring review of diabetes medication dosing.
Patients should be reassured that experiencing some degree of tiredness during the initial treatment phase is not uncommon and does not necessarily indicate treatment failure or serious adverse effects.
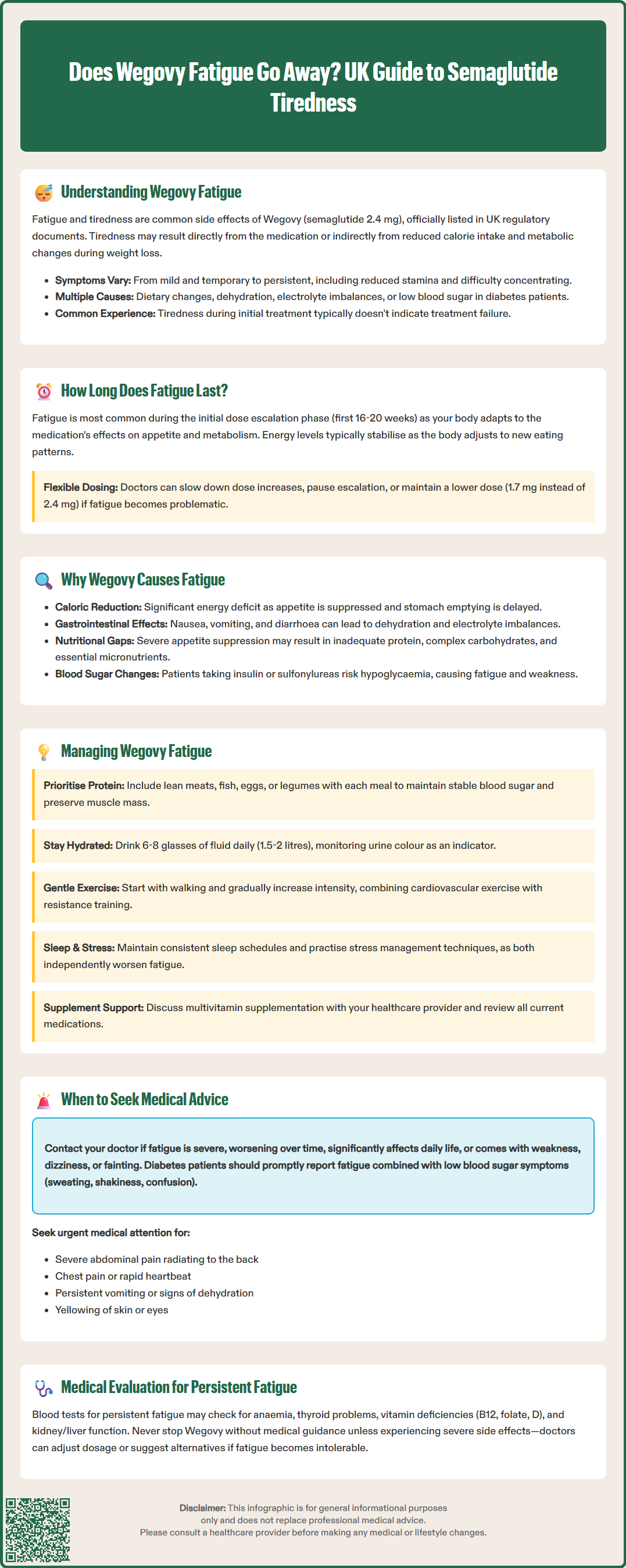
The duration of fatigue experienced by patients taking Wegovy varies considerably between individuals. Clinical experience suggests that fatigue is often most pronounced during the initial dose escalation phase, when the body is adapting to the medication's effects on appetite, gastric emptying, and glucose metabolism.
Wegovy treatment follows a structured dose escalation schedule, starting at 0.25 mg weekly and gradually increasing over 16–20 weeks to the maintenance dose of 2.4 mg weekly. This gradual titration is designed to minimise gastrointestinal side effects, but it also allows the body time to adjust metabolically. According to the SmPC, clinicians may consider pausing dose escalation, slowing the titration schedule, or maintaining a lower dose (such as 1.7 mg) if patients experience significant tolerability issues, including persistent fatigue.
Fatigue reported during the first month often coincides with significant dietary changes, as patients experience reduced appetite and consume fewer calories than their pre-treatment baseline. This caloric deficit, whilst therapeutically desirable for weight loss, can temporarily affect energy levels until metabolic adaptation occurs.
For many patients, fatigue may diminish as they progress through the dose escalation schedule and establish new eating patterns. The body typically adjusts to the lower caloric intake, and energy levels may stabilise over time. However, some patients may experience persistent fatigue, which warrants further clinical evaluation to exclude other contributing factors such as nutritional deficiencies (particularly iron, vitamin B12, or vitamin D), thyroid dysfunction, or inadequate protein intake.
It is important to note that there is no official clinical guidance specifying an exact timeline for resolution of Wegovy-related fatigue, as individual responses vary based on baseline health status, concurrent medications, lifestyle factors, and adherence to nutritional recommendations. Patients experiencing prolonged or worsening fatigue should discuss their symptoms with their prescribing clinician or GP.
Understanding the potential mechanisms underlying fatigue during Wegovy treatment requires consideration of both the drug's pharmacological action and its downstream metabolic effects. Semaglutide works by mimicking the action of endogenous GLP-1, a hormone released from the intestine in response to food intake. It acts on GLP-1 receptors in multiple tissues, including the pancreas, brain, and gastrointestinal tract.
The primary mechanisms through which Wegovy promotes weight loss include:
Appetite suppression through central nervous system effects, reducing hunger and food cravings
Delayed gastric emptying, prolonging satiety after meals
Enhanced insulin secretion and reduced glucagon release, improving glycaemic control
Reduced energy intake, creating a sustained caloric deficit
These therapeutic effects can contribute to fatigue through several pathways. The significant reduction in caloric intake represents the most direct mechanism—when energy consumption drops substantially, particularly during the initial treatment phase, the body may not immediately adapt its energy expenditure accordingly. This mismatch can manifest as tiredness, reduced physical stamina, and decreased motivation for physical activity.
Additionally, gastrointestinal side effects such as nausea, vomiting, or diarrhoea—which affect a substantial proportion of patients—can lead to dehydration and electrolyte disturbances, both recognised causes of fatigue. Inadequate fluid intake, whether due to nausea or reduced thirst perception, compounds this issue. Furthermore, patients who experience significant appetite suppression may inadvertently consume insufficient protein, complex carbohydrates, or micronutrients essential for maintaining energy levels and metabolic function.
Patients taking insulin or sulfonylureas alongside Wegovy may experience hypoglycaemia, which can present as fatigue, weakness, or confusion. This requires careful monitoring and potential adjustment of diabetes medications.
In rare cases, more serious conditions such as acute pancreatitis or gallbladder disease (both recognised potential adverse effects of GLP-1 receptor agonists) may present with systemic symptoms including fatigue and malaise alongside more specific symptoms.
While fatigue is a documented adverse reaction with semaglutide, the precise pharmacological mechanism is not fully established. Individual variation in drug metabolism, concurrent medical conditions, and baseline nutritional status may influence susceptibility to fatigue during treatment.
Practical strategies can help patients minimise fatigue and maintain quality of life whilst benefiting from Wegovy's weight management effects. A structured, multifaceted approach addressing nutrition, hydration, physical activity, and lifestyle factors typically yields the best outcomes.
Nutritional optimisation forms the cornerstone of fatigue management:
Include protein with each meal: Focus on incorporating protein sources at each meal, such as lean meats, fish, eggs, dairy products, legumes, or plant-based alternatives to help preserve muscle mass. If working with a dietitian, they may recommend specific protein targets based on your individual needs and health status (particularly important if you have kidney disease).
Choose nutrient-dense foods: Focus on whole grains, fruits, vegetables, nuts, and seeds to ensure adequate micronutrient intake despite reduced overall food consumption.
Eat regular, smaller meals: Rather than forcing large portions, consume smaller, frequent meals to maintain stable blood glucose levels and work with Wegovy's appetite-suppressing effects.
Consider supplementation: Discuss with your healthcare provider whether a multivitamin or specific supplements (iron, vitamin B12, vitamin D) might be appropriate, particularly if dietary intake is significantly restricted.
Hydration and electrolyte balance are equally important:
Aim for 6-8 glasses of fluid daily (about 1.5-2 litres), as recommended by the NHS, but individualise based on your activity level, climate, and medical conditions
If you have heart or kidney disease, discuss appropriate fluid intake with your healthcare provider
Include electrolyte-containing beverages if experiencing gastrointestinal side effects, but be mindful of sugar content
Monitor urine colour as a simple hydration indicator (pale yellow suggests adequate hydration)
Physical activity, whilst challenging when fatigued, can paradoxically improve energy levels:
Start with gentle activities such as walking, gradually increasing intensity as tolerated
Incorporate both cardiovascular exercise and resistance training to maintain muscle mass
Schedule activity during times of day when energy levels are typically higher
Sleep hygiene and stress management should not be overlooked, as poor sleep quality and chronic stress independently contribute to fatigue. Establishing consistent sleep schedules, creating a restful bedroom environment, and practising relaxation techniques can support overall energy levels during treatment.
Additional considerations:
If you have diabetes and take insulin or sulfonylureas, monitor your blood glucose levels regularly and discuss potential dose adjustments with your healthcare team
Review all current medications with your prescriber, as some may contribute to fatigue
Discuss with your clinician whether slowing the dose escalation or temporarily maintaining a lower dose might help manage fatigue
Whilst mild fatigue during the initial weeks of Wegovy treatment may be expected, certain symptoms warrant prompt medical evaluation. Patients should contact their GP or prescribing clinician if they experience any of the following:
Severe or worsening fatigue that:
Persists despite implementing lifestyle modifications
Progressively worsens rather than improving over time
Significantly impairs daily functioning, work performance, or quality of life
Is accompanied by weakness, dizziness, or fainting episodes
Associated symptoms suggesting potential complications:
Severe, persistent abdominal pain, possibly radiating to the back, with or without vomiting (potential signs of pancreatitis requiring urgent medical attention)
Pain in the right upper abdomen, fever, or jaundice (potential signs of gallbladder disease)
Persistent nausea, vomiting, or diarrhoea leading to dehydration
Signs of dehydration: dark urine, dry mouth, reduced urine output, confusion
Rapid or irregular heartbeat, chest pain, or shortness of breath
Unexplained weight loss exceeding recommended targets (faster than about 0.5-1 kg per week)
Mood changes, depression, or anxiety
Yellowing of skin or eyes, dark urine, or pale stools (potential liver concerns)
For patients with diabetes, particularly those taking insulin or sulfonylureas, symptoms of hypoglycaemia (sweating, shakiness, confusion, irritability) alongside fatigue require prompt attention and potential medication adjustment.
NICE guidance on obesity management emphasises the importance of regular monitoring during pharmacological treatment. Patients prescribed Wegovy should have scheduled follow-up appointments to assess treatment response, side effects, and overall health status. These consultations provide opportunities to discuss fatigue and other concerns, adjust management strategies, and conduct relevant investigations if indicated.
Investigations that may be appropriate for persistent fatigue include:
Full blood count (to exclude anaemia)
Thyroid function tests (TSH, free T4)
Vitamin B12 and folate levels
Vitamin D status
Renal and liver function tests
Fasting glucose and HbA1c (particularly in patients with diabetes)
Patients should not discontinue Wegovy without medical guidance unless experiencing severe adverse effects. If severe side effects occur, it is appropriate to stop the medication and seek urgent medical advice. If fatigue becomes intolerable, healthcare professionals can discuss dose adjustment, temporary treatment interruption, or alternative weight management strategies.
Open communication between patients and their healthcare team is essential for optimising treatment outcomes whilst maintaining safety and quality of life throughout the weight management journey. Suspected adverse reactions to Wegovy should be reported through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Wegovy-related fatigue is often most pronounced during the initial dose escalation phase (first 16–20 weeks) and typically improves as the body adapts to reduced caloric intake and metabolic changes. Individual experiences vary, with some patients noticing improvement within weeks whilst others may experience persistent tiredness requiring medical evaluation.
Yes, practical strategies include ensuring adequate protein intake at each meal, maintaining hydration (6-8 glasses daily), consuming nutrient-dense foods, eating smaller frequent meals, and gradually increasing physical activity. Discussing potential supplementation and medication adjustments with your healthcare provider may also help manage fatigue.
Contact your GP or prescribing clinician if fatigue is severe, progressively worsening, significantly impairs daily functioning, or is accompanied by symptoms such as persistent abdominal pain, vomiting, dizziness, rapid heartbeat, signs of dehydration, or symptoms of hypoglycaemia (if you have diabetes). Persistent fatigue despite lifestyle modifications also warrants medical review.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.