
Feeling light-headed whilst taking Mounjaro (tirzepatide) is a recognised side effect that can affect patients with type 2 diabetes. This symptom may arise from several mechanisms, including low blood glucose, dehydration, or changes in blood pressure regulation. Understanding why light-headedness occurs and how to manage it effectively is essential for safe and successful treatment. This article explores the causes of dizziness on Mounjaro, when to seek medical advice, and practical strategies to minimise symptoms whilst continuing therapy. Appropriate monitoring and medication adjustments can help most patients manage this side effect safely.
Quick Answer: Light-headedness on Mounjaro (tirzepatide) commonly results from low blood glucose, dehydration, or orthostatic hypotension, particularly in patients taking concurrent glucose-lowering or antihypertensive medications.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Dizziness is listed as a common adverse reaction in the Summary of Product Characteristics (SmPC), with the risk being higher in patients taking concurrent glucose-lowering medications or experiencing dehydration.
The mechanism behind light-headedness on Mounjaro is multifactorial. As a GLP-1/GIP receptor agonist, tirzepatide enhances glucose-dependent insulin secretion and suppresses glucagon release, which can lead to lower blood glucose levels. In susceptible individuals, particularly those on concurrent glucose-lowering medications such as insulin or sulphonylureas, this may result in hypoglycaemia—a recognised cause of dizziness and light-headedness. Additionally, Mounjaro slows gastric emptying and reduces appetite, which can lead to decreased caloric and fluid intake. Reduced fluid consumption may contribute to dehydration and orthostatic hypotension (a drop in blood pressure upon standing), both of which manifest as dizziness.
Furthermore, patients using Mounjaro often experience significant weight loss, which can be accompanied by changes in blood pressure regulation. Those with pre-existing hypertension who are taking antihypertensive medications may find their blood pressure drops more than anticipated, leading to symptoms of light-headedness. Understanding these mechanisms is essential for both patients and healthcare professionals to identify the underlying cause and implement appropriate management strategies. It is important to note that whilst light-headedness can be concerning, it is often manageable with careful monitoring and dose adjustments.
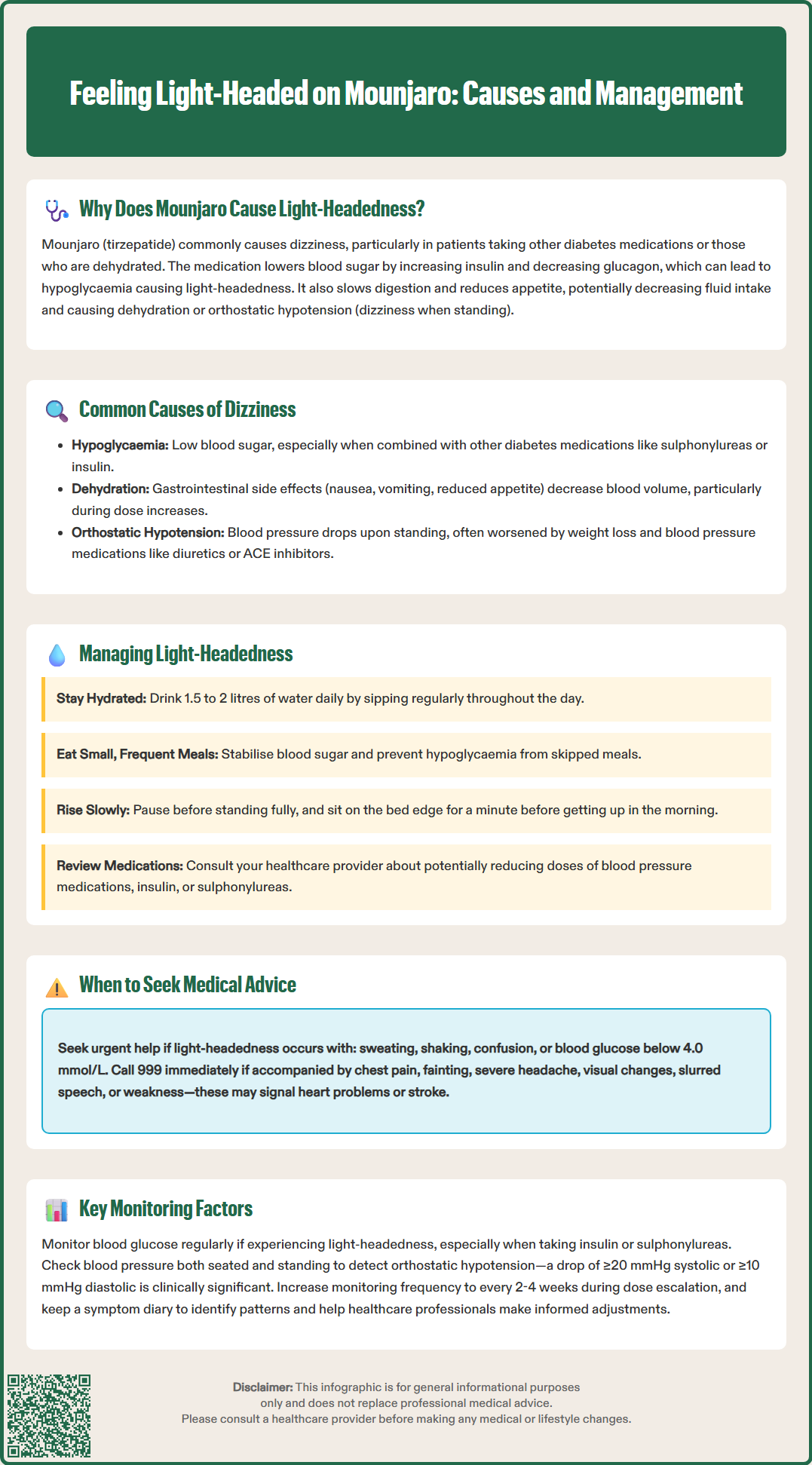
Several specific factors contribute to dizziness in patients taking Mounjaro, and recognising these can help guide appropriate intervention. Hypoglycaemia is a primary concern, especially in individuals using Mounjaro alongside other glucose-lowering agents such as sulphonylureas or insulin. Tirzepatide's glucose-dependent mechanism means it carries a lower intrinsic risk of hypoglycaemia when used alone, but combination therapy increases this risk. Symptoms of low blood sugar include dizziness, sweating, tremor, confusion, and palpitations.
Dehydration and reduced oral intake are common, particularly during the dose escalation phase. Mounjaro frequently causes gastrointestinal side effects—nausea, vomiting, and reduced appetite—which can lead to inadequate fluid and electrolyte intake. Dehydration reduces circulating blood volume, predisposing patients to orthostatic hypotension and dizziness, particularly when moving from sitting to standing.
Orthostatic hypotension may also occur independently of dehydration, especially in patients taking antihypertensive medications. As weight loss progresses and metabolic parameters improve, blood pressure may fall, sometimes excessively. This is particularly relevant for those on diuretics, ACE inhibitors, beta-blockers, alpha-blockers, or SGLT2 inhibitors (which can cause volume depletion). A postural drop in systolic blood pressure of 20 mmHg or more, or diastolic pressure of 10 mmHg or more, is clinically significant.
Vasovagal responses related to gastrointestinal distress or anxiety about injections may also contribute. If dizziness persists despite addressing medication-related causes, other common conditions such as anaemia, vestibular disorders, or cardiac arrhythmias should be considered. Identifying which of these factors is predominant in an individual patient is crucial for tailoring management effectively.
Whilst mild, transient light-headedness may resolve with simple measures, certain symptoms warrant prompt medical evaluation. Patients should contact their GP or diabetes specialist nurse if light-headedness is persistent, severe, or worsening despite self-management strategies, as this may indicate an underlying issue requiring medication adjustment or further investigation.
Symptoms suggestive of hypoglycaemia—such as dizziness accompanied by sweating, shaking, confusion, palpitations, or hunger—require urgent attention, particularly if blood glucose readings are consistently below 4.0 mmol/L. Patients on combination therapy with insulin or sulphonylureas should be especially vigilant, and dose reductions of these agents may be necessary.
Immediate medical attention is required if light-headedness is associated with chest pain, shortness of breath, palpitations, or syncope (fainting). These symptoms could indicate cardiac arrhythmia, significant hypotension, or other serious cardiovascular events. Similarly, if dizziness is accompanied by severe headache, visual disturbances, slurred speech, or weakness, this may suggest a neurological event such as a transient ischaemic attack or stroke, and emergency services (999) should be contacted immediately.
Patients experiencing recurrent falls due to dizziness should seek medical review, as falls carry significant risk of injury, particularly in older adults or those with comorbidities. Additionally, if light-headedness is accompanied by persistent vomiting, inability to tolerate fluids, or signs of dehydration (dark urine, dry mouth, reduced urine output), medical assessment is necessary to exclude complications such as acute kidney injury.
Urgent medical advice should also be sought for severe, persistent abdominal pain (with or without vomiting), which could indicate pancreatitis or gallbladder disease—known adverse effects associated with GLP-1 receptor agonists. NICE guidance (NG28) emphasises the importance of patient education regarding warning symptoms and clear pathways for seeking help when adverse effects occur.
Effective management of light-headedness on Mounjaro involves both non-pharmacological strategies and, where necessary, medication adjustments. Adequate hydration is paramount. Patients should be advised to maintain a fluid intake of at least 1.5 to 2 litres daily, unless contraindicated by other medical conditions. Sipping water regularly throughout the day, rather than consuming large volumes at once, can help maintain hydration without exacerbating nausea.
Dietary modifications are also important. Eating small, frequent meals rather than large portions can help manage gastrointestinal side effects and maintain stable blood glucose levels. Patients should avoid skipping meals, as this increases the risk of hypoglycaemia. Salt intake should not be increased unless specifically advised by a healthcare professional, as this could be harmful for those with hypertension, heart failure, or kidney disease.
Postural changes should be made gradually. Patients experiencing orthostatic symptoms should be advised to rise slowly from sitting or lying positions, pausing for a few moments before standing fully. Sitting on the edge of the bed for a minute before standing in the morning can be particularly helpful. Compression stockings may benefit some individuals with significant orthostatic hypotension, but should only be used after clinical assessment and avoided if peripheral arterial disease is suspected.
Medication review is essential. Healthcare professionals should assess whether dose reductions of concurrent antihypertensive or glucose-lowering medications are appropriate. For patients on insulin or sulphonylureas, proactive dose reduction at the initiation of Mounjaro is recommended in the SmPC to minimise hypoglycaemia risk. Similarly, antihypertensive regimens may require adjustment as weight loss and metabolic improvements occur.
If vomiting or dehydration occurs, patients should follow 'sick day rules' and consider temporarily withholding certain medications (SADMAN: Sulphonylureas, ACE inhibitors/ARBs, Diuretics, Metformin, And SGLT2 inhibitors) in consultation with their healthcare team. This helps reduce the risk of acute kidney injury and diabetic ketoacidosis. If light-headedness persists despite these measures, temporarily reducing the Mounjaro dose or extending the interval between dose escalations may be considered, in consultation with the prescribing clinician. Patients should never adjust their Mounjaro dose independently without medical guidance.
Regular monitoring of blood pressure and blood glucose is essential for patients experiencing light-headedness on Mounjaro, as these parameters provide objective data to guide management decisions. Blood glucose monitoring is particularly important for individuals on combination therapy with insulin or sulphonylureas. Patients should be advised to check their blood glucose if they experience symptoms of hypoglycaemia, and routine monitoring before meals and at bedtime can help identify patterns. Target blood glucose levels should be individualised, but generally, readings below 4.0 mmol/L indicate hypoglycaemia requiring treatment with fast-acting carbohydrate (15–20g, such as glucose tablets or a small glass of fruit juice), followed by a longer-acting carbohydrate snack.
Blood pressure monitoring should include both seated and standing measurements, particularly if orthostatic hypotension is suspected. Patients can be taught to measure their own blood pressure at home using a validated device. A postural drop (measured after standing for 1–3 minutes) of ≥20 mmHg systolic or ≥10 mmHg diastolic is clinically significant. Home blood pressure monitoring allows for detection of patterns that may not be apparent during clinic visits.
Healthcare professionals should review these parameters regularly, particularly during dose escalation phases. NICE guidance (NG28) recommends that patients with type 2 diabetes have their HbA1c checked every 3–6 months, and blood pressure should be monitored at each diabetes review. For patients on Mounjaro experiencing light-headedness, more frequent monitoring may be appropriate—potentially every 2–4 weeks initially—until symptoms stabilise. Adjustments to concurrent medications should be made based on these objective measurements rather than symptoms alone.
Patients should be provided with clear guidance on target ranges and when to seek advice if readings fall outside these parameters. Those at risk of hypoglycaemia should follow DVLA guidance regarding driving safety. Maintaining a symptom and measurement diary can be invaluable for identifying triggers and patterns, facilitating more informed discussions with healthcare professionals. Patients are encouraged to report any suspected adverse reactions to Mounjaro via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Mounjaro can cause light-headedness through several mechanisms: lowering blood glucose (especially with concurrent insulin or sulphonylureas), reducing fluid intake due to gastrointestinal side effects leading to dehydration, and causing orthostatic hypotension as blood pressure falls with weight loss.
Contact your GP if light-headedness is persistent, severe, or worsening, or if accompanied by symptoms of hypoglycaemia (sweating, shaking, confusion). Seek immediate medical attention if you experience chest pain, fainting, severe headache, visual disturbances, or recurrent falls.
Maintain adequate hydration (1.5–2 litres daily), eat small frequent meals, rise slowly from sitting or lying positions, and monitor blood glucose and blood pressure regularly. Your healthcare team may need to adjust doses of concurrent antihypertensive or glucose-lowering medications.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.