
Hair loss whilst on GLP-1 medications has become an increasingly reported concern amongst patients using these treatments for type 2 diabetes or weight management. Glucagon-like peptide-1 (GLP-1) receptor agonists—including semaglutide (Ozempic®, Wegovy®), liraglutide (Saxenda®, Victoza®), and tirzepatide (Mounjaro®)—are highly effective for glycaemic control and weight reduction, but some individuals experience hair thinning during treatment. Understanding whether this represents a direct drug effect or a consequence of rapid metabolic changes is essential for appropriate management. This article examines the relationship between GLP-1 medications and hair changes, explores underlying mechanisms, and provides evidence-based guidance for patients and healthcare professionals.
Quick Answer: Hair loss whilst on GLP-1 medications is not typically a direct drug effect but may occur as telogen effluvium triggered by rapid weight loss, nutritional deficiencies, or metabolic stress, and is usually temporary and reversible.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists represent a class of medications increasingly prescribed in the UK for type 2 diabetes management and, more recently, for weight management in adults with obesity. These medicines include semaglutide (marketed as Ozempic® for diabetes and Wegovy® for weight management), liraglutide (Saxenda® for weight management, Victoza® for diabetes), dulaglutide (Trulicity® for diabetes), and tirzepatide (Mounjaro® for diabetes), which combines GLP-1 with glucose-dependent insulinotropic polypeptide (GIP) receptor agonism.
GLP-1 medications work by mimicking the action of naturally occurring incretin hormones produced in the intestine. Their primary mechanisms include:
Enhancing insulin secretion from pancreatic beta cells in response to elevated blood glucose
Suppressing glucagon release, thereby reducing hepatic glucose production
Slowing gastric emptying, which prolongs satiety and reduces appetite
Acting on appetite centres in the brain, particularly the hypothalamus, to reduce food intake
These combined effects lead to improved glycaemic control in people with type 2 diabetes and significant weight reduction in those using these medications for obesity management. Clinical trials have demonstrated varying degrees of weight loss depending on the specific agent and dosage: semaglutide 2.4mg (Wegovy®) produces approximately 15% weight loss at 68 weeks, liraglutide 3mg (Saxenda®) typically achieves 5-8% weight loss, while tirzepatide has shown up to 20% weight reduction in obesity trials.
Whilst GLP-1 receptor agonists are generally well-tolerated, they can produce various side effects. The most commonly reported adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and constipation, which typically diminish over time. However, patients and healthcare professionals have increasingly noted concerns about hair changes during treatment, prompting questions about whether these medications directly affect hair growth and follicle health.
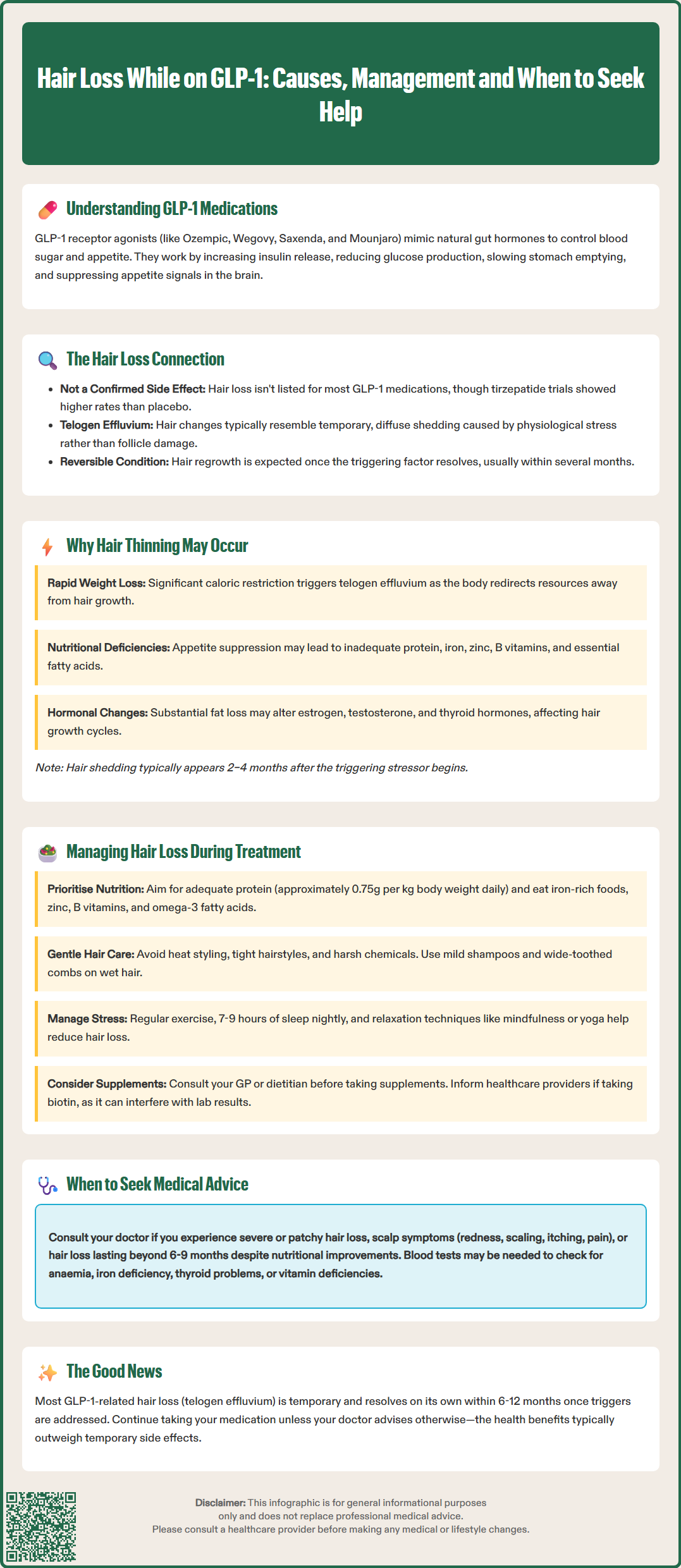
The relationship between GLP-1 receptor agonists and hair loss remains an area of ongoing investigation. While hair loss is not established as a class effect of GLP-1 medications, clinical trial data and product information vary by agent. For most GLP-1 medications, alopecia is not listed as a common adverse effect in the Summary of Product Characteristics (SmPC) approved by the Medicines and Healthcare products Regulatory Agency (MHRA). However, it's worth noting that in clinical trials for tirzepatide for weight management, alopecia was reported more frequently than with placebo.
Post-marketing surveillance and patient reports have documented cases of hair thinning or increased hair shedding amongst individuals taking GLP-1 medications, particularly those experiencing substantial weight loss. These reports have prompted healthcare professionals to consider whether hair changes represent an indirect consequence of treatment rather than a direct drug effect.
It is important to distinguish between different types of hair loss:
Telogen effluvium: A temporary condition where hair follicles prematurely enter the resting (telogen) phase, leading to diffuse hair shedding 2–3 months after a triggering event
Androgenetic alopecia: Pattern hair loss related to genetic and hormonal factors
Alopecia areata: An autoimmune condition causing patchy hair loss
The hair changes reported with GLP-1 use most commonly resemble telogen effluvium, characterised by diffuse thinning rather than discrete bald patches. This pattern suggests that if hair loss occurs during GLP-1 treatment, it likely results from physiological stress or nutritional factors rather than direct drug toxicity to hair follicles.
Patients concerned about hair changes should be reassured that telogen effluvium is typically reversible, with hair regrowth occurring once the underlying trigger resolves. Nevertheless, any significant or persistent hair loss warrants medical evaluation to exclude other contributing factors.
Several interconnected factors may explain why some individuals experience hair thinning whilst taking GLP-1 medications, even though these drugs do not directly damage hair follicles.
Rapid weight loss represents the most plausible explanation for hair changes during GLP-1 treatment. Substantial caloric restriction and rapid weight reduction—whether achieved through medication, surgery, or dietary intervention—constitute a physiological stressor that can trigger telogen effluvium. When the body experiences significant metabolic changes, it may temporarily redirect resources away from non-essential functions such as hair growth. Research suggests that significant weight loss over a short period may increase the risk of temporary hair shedding, though individual responses vary considerably.
Nutritional deficiencies may develop during GLP-1 treatment, particularly when appetite suppression leads to inadequate dietary intake. Hair follicles require specific nutrients for optimal function, including:
Protein: Essential for keratin production, the structural component of hair
Iron: Necessary for oxygen transport to follicles; deficiency commonly causes hair loss
Zinc: Supports hair tissue growth and repair
B vitamins: Important for hair health, though deficiency is relatively uncommon
Essential fatty acids: Support scalp health and hair structure
The gastrointestinal side effects of GLP-1 medications—particularly nausea, vomiting, and altered eating patterns—may further compromise nutritional status, potentially contributing to hair changes.
Hormonal fluctuations may also play a role, though this mechanism is not firmly established in GLP-1 users. Adipose tissue functions as an endocrine organ, and substantial fat loss can potentially alter levels of various hormones, including oestrogen, testosterone, and thyroid hormones, all of which influence hair growth cycles.
Finally, the psychological and physical stress of adapting to new medication, managing side effects, and experiencing body composition changes may independently trigger telogen effluvium in susceptible individuals. It is worth noting that hair loss typically manifests 2–4 months after the initiating stressor, meaning hair shedding may not coincide precisely with the start of GLP-1 treatment.
If you experience hair thinning whilst taking a GLP-1 medication, several strategies may help support hair health and potentially minimise further loss.
Optimise nutritional intake by ensuring your diet remains balanced despite reduced appetite. Focus on:
Adequate protein consumption: Aim for sufficient protein based on individual needs (the UK Reference Nutrient Intake is approximately 0.75g per kilogram of body weight daily, though requirements may be higher during weight loss). Good sources include lean meat, fish, eggs, dairy, legumes, and plant-based alternatives. Consult a registered dietitian if you have chronic kidney disease or other conditions affecting protein requirements.
Iron-rich foods: Include red meat, poultry, fish, fortified cereals, dark leafy greens, and pulses; consider pairing plant-based iron sources with vitamin C to enhance absorption
Varied, nutrient-dense meals: Prioritise foods providing zinc (shellfish, meat, seeds, nuts), B vitamins (whole grains, eggs, dairy), and omega-3 fatty acids (oily fish, walnuts, flaxseeds)
Consider nutritional supplementation if dietary intake proves insufficient, though this should ideally follow discussion with your GP or a registered dietitian. Routine supplementation without confirmed deficiency is not typically recommended. If taking biotin supplements, be aware that high doses can interfere with certain laboratory tests, including thyroid function tests and cardiac markers—inform healthcare professionals before blood tests.
Maintain gentle hair care practices:
Avoid excessive heat styling, tight hairstyles, and harsh chemical treatments
Use a wide-toothed comb and handle hair gently when wet
Choose mild, sulphate-free shampoos
Treat hair gently and avoid unnecessary manipulation
Manage stress through regular physical activity, adequate sleep (7–9 hours nightly), and relaxation techniques such as mindfulness or yoga, as chronic stress can exacerbate hair loss.
Continue your GLP-1 medication unless advised otherwise by your prescribing clinician. The benefits of improved glycaemic control or weight management typically outweigh concerns about temporary hair thinning, particularly as telogen effluvium usually resolves spontaneously within 6–12 months. Never stop a GLP-1 medication prescribed for diabetes without medical advice.
Monitor your progress by taking photographs at regular intervals, which provides more objective assessment than daily observation and can help determine whether hair density is genuinely declining or stabilising.
If you suspect your medication may be causing side effects, including hair loss, you can report this through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Whilst mild hair thinning during GLP-1 treatment may not require immediate intervention, certain circumstances warrant medical evaluation.
Contact your GP or prescribing clinician if you experience:
Severe or rapidly progressive hair loss, particularly if it occurs in patches rather than diffuse thinning
Hair loss accompanied by scalp symptoms such as redness, scaling, itching, pain, or visible inflammation (which may indicate scarring alopecia requiring urgent dermatology referral)
Signs of potential nutritional deficiency, including persistent fatigue, weakness, pallor, brittle nails, mouth ulcers, or neurological symptoms
Hair loss persisting beyond 6–9 months or worsening despite nutritional optimisation
Significant psychological distress related to hair changes affecting your quality of life
Your healthcare provider may recommend blood tests to investigate potential underlying causes, which might include:
Full blood count: To assess for anaemia
Ferritin levels: To evaluate iron stores (aim to treat iron deficiency to within the laboratory reference range)
Thyroid function tests: To exclude hypothyroidism or hyperthyroidism
Vitamin B12 and folate: Particularly relevant if dietary intake is restricted
Coeliac serology: May be considered if iron deficiency is present without obvious cause
Zinc levels: Though testing can be unreliable, may be considered in specific circumstances
Depending on findings, your GP may suggest adjusting your GLP-1 dosage, slowing the rate of weight loss, or referring you to a dermatologist for specialist assessment if hair loss appears atypical or fails to improve.
Referral to a dietitian may prove beneficial to ensure adequate nutritional intake whilst managing appetite suppression. The NHS provides access to dietetic services, and NICE guidance supports nutritional assessment for individuals experiencing significant weight changes.
It is important to maintain open communication with your healthcare team about any side effects or concerns during GLP-1 treatment. Hair changes, whilst often temporary and benign, deserve appropriate evaluation to ensure optimal management of both your underlying condition and overall wellbeing. Remember that most cases of telogen effluvium resolve spontaneously once triggering factors are addressed, and hair typically returns to its previous density within 6–12 months.
Hair loss is not listed as a common adverse effect for most GLP-1 medications in UK product information, though tirzepatide trials reported alopecia more frequently than placebo. Post-marketing reports suggest hair thinning may occur, particularly with substantial weight loss, but this likely represents telogen effluvium triggered by metabolic changes rather than direct drug toxicity.
Most cases of hair thinning during GLP-1 treatment represent telogen effluvium, which is typically reversible. Hair usually returns to its previous density within 6–12 months once triggering factors (such as rapid weight loss or nutritional deficiencies) are addressed, even if GLP-1 treatment continues.
Optimise nutritional intake by ensuring adequate protein (approximately 0.75g per kilogram body weight daily), iron-rich foods, and varied nutrient-dense meals despite reduced appetite. Maintain gentle hair care practices, manage stress, and consider consulting a registered dietitian if dietary intake proves insufficient during treatment.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.