
Glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide and liraglutide are increasingly prescribed in the UK for type 2 diabetes and weight management. Whilst these medications effectively facilitate weight reduction, patients may notice skin changes including increased laxity or apparent thinning. Understanding how to prevent skin thinning during a GLP-1 regimen requires recognising that these changes typically result from rapid fat loss rather than direct drug effects on dermal tissue. This article examines evidence-based strategies to support skin health during GLP-1 therapy, including optimised nutrition, appropriate exercise, and skincare practices aligned with UK clinical guidance.
Quick Answer: Preventing skin thinning during GLP-1 regimen involves optimising weight loss rate, maintaining adequate protein intake, performing resistance exercise, and supporting dermal health through hydration and sun protection.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists, including semaglutide (Ozempic, Wegovy) and liraglutide (Saxenda, Victoza), have become increasingly prescribed for type 2 diabetes management and weight management in the UK. These medications work by mimicking the action of naturally occurring GLP-1 hormone, which enhances insulin secretion, suppresses glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways. Whilst these agents are effective for glycaemic control and weight management in indicated groups, patients and clinicians have observed various dermatological changes during treatment.
Skin alterations reported during GLP-1 therapy are likely multifactorial. Evidence suggests they are predominantly secondary to the substantial and often rapid weight loss these agents facilitate, rather than a direct pharmacological effect on skin tissue. The MHRA product information for GLP-1 receptor agonists does not list skin thinning as a recognised adverse drug reaction, though other skin-related effects are noted, including injection site reactions, rash, pruritus, and alopecia (with semaglutide for weight management).
Patients may notice changes in skin texture, increased laxity, or apparent thinning, particularly in areas where subcutaneous fat has diminished significantly. These observations have led to colloquial terms such as 'Ozempic face' in popular media, though such terminology lacks clinical precision. Understanding the distinction between true dermal thinning and the appearance of skin changes secondary to fat loss is essential for appropriate management. Healthcare professionals should counsel patients that whilst these cosmetic concerns are valid, they represent a common consequence of therapeutic weight reduction rather than a direct drug effect on skin structure.
To minimise injection site reactions, patients should rotate injection sites according to the manufacturer's instructions and speak to their healthcare provider if they experience persistent skin issues.
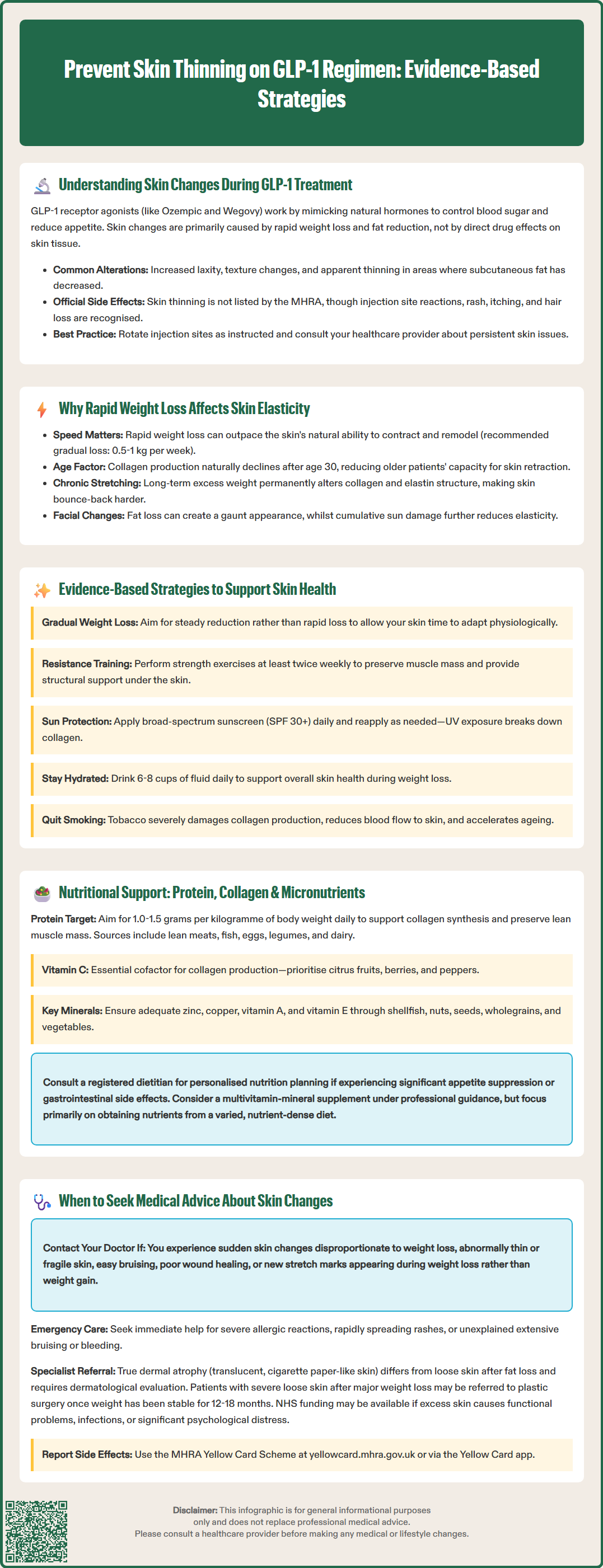
The skin is a dynamic organ with remarkable adaptive capacity, but this adaptation requires time. When weight loss occurs gradually—typically 0.5 to 1 kg per week as recommended by NHS guidance—the dermis can remodel and contract in response to reduced underlying tissue volume. However, GLP-1 receptor agonists often facilitate more rapid weight reduction, particularly in the initial months of treatment, which may outpace the skin's natural remodelling capacity.
The dermis contains a structural matrix of collagen and elastin fibres that provide strength and elasticity. During periods of weight gain, this matrix stretches to accommodate increased subcutaneous adipose tissue. When fat volume decreases rapidly, the dermal scaffold may not contract proportionally, resulting in redundant skin that appears loose or thin. This effect is particularly pronounced in individuals who have carried excess weight for extended periods, as chronic stretching may significantly alter dermal architecture.
Several physiological factors influence skin elasticity during weight loss. Age is a critical determinant, as dermal collagen production naturally declines with age, with studies suggesting a gradual reduction after age 30. Older patients therefore have reduced capacity for skin retraction following fat loss. Additionally, the anatomical distribution of weight loss matters: facial fat pads provide structural support and volume, and their reduction can create a gaunt appearance that emphasises skin laxity.
Cumulative ultraviolet radiation exposure significantly contributes to reduced skin elasticity and can exacerbate the appearance of skin laxity during weight loss. Nutritional status during weight loss also profoundly affects skin health. Caloric restriction, whilst necessary for weight reduction, may inadvertently limit intake of essential nutrients required for collagen synthesis and dermal maintenance. Protein-energy malnutrition, micronutrient deficiencies (particularly vitamin C, zinc, and copper), and inadequate hydration can all compromise skin integrity during periods of rapid weight change.
Whilst there is limited specific research on preventing skin changes during GLP-1 therapy, established dermatological principles and weight management guidance provide a framework for supportive care. The cornerstone approach involves optimising the rate of weight loss to allow physiological adaptation. Clinicians should work with patients to achieve steady, sustainable weight reduction rather than maximising speed of loss, which may involve dose titration strategies that balance metabolic benefits with tolerability.
Resistance training and strength-based exercise play a crucial role in preserving lean body mass during weight loss. The UK Chief Medical Officers' Physical Activity Guidelines recommend muscle-strengthening activities on at least two days per week. Maintaining muscle mass beneath the skin provides structural support and may reduce the appearance of skin laxity. Patients should be encouraged to engage in resistance exercises targeting major muscle groups, alongside regular aerobic activity.
Topical skincare regimens, whilst unable to reverse significant structural changes, can support dermal health. Daily application of broad-spectrum sunscreen (SPF 30 or higher with high UVA protection) is essential, as ultraviolet radiation accelerates collagen degradation and impairs skin elasticity. Reapply as directed, especially after swimming or sweating. Moisturisers containing humectants (such as hyaluronic acid or glycerin) help maintain skin hydration, whilst those with retinoids may stimulate collagen production, though evidence for their efficacy in this specific context remains limited. Retinoid products should be avoided during pregnancy and introduced gradually to minimise irritation; consult a pharmacist or clinician before use.
Adequate hydration is fundamental to skin health. The NHS recommends 6-8 cups of fluid daily (approximately 1.2 litres), adjusted for individual factors such as activity level and climate. Smoking cessation is imperative, as tobacco use significantly impairs collagen synthesis, reduces dermal blood flow, and accelerates skin ageing. Healthcare professionals should offer smoking cessation support as a priority intervention for any patient concerned about skin health during weight loss.
Nutritional optimisation is paramount for maintaining skin integrity during GLP-1 therapy. The appetite-suppressing effects of these medications can inadvertently lead to inadequate nutrient intake if dietary quality is not prioritised. Protein intake deserves particular attention, as amino acids serve as building blocks for collagen synthesis and are essential for maintaining lean body mass. Current evidence suggests that individuals undergoing weight loss may benefit from consuming approximately 1.0 to 1.5 grams of protein per kilogram of body weight daily, distributed across meals to optimise muscle protein synthesis. This should be tailored with input from a registered dietitian, particularly for those with kidney disease or other conditions where higher protein intake may be inappropriate.
High-quality protein sources include lean meats, fish, eggs, dairy products, legumes, and soy-based foods. For patients struggling with reduced appetite, protein supplementation may be appropriate, though whole food sources are preferable when tolerated. Collagen peptide supplements have gained popularity for skin health support; whilst some studies suggest potential benefits for skin elasticity and hydration, the evidence base remains modest and further research is needed to establish definitive recommendations.
Micronutrients critical for collagen synthesis and skin health include:
Vitamin C: Essential cofactor for collagen hydroxylation; found in citrus fruits, berries, peppers, and leafy greens
Zinc: Required for collagen synthesis and wound healing; sources include shellfish, meat, seeds, and legumes
Copper: Necessary for cross-linking collagen and elastin fibres; present in nuts, seeds, and wholegrains
Vitamin A: Supports skin cell turnover and differentiation; obtained from dairy and orange vegetables (note: liver and liver products contain very high levels of vitamin A and should be avoided during pregnancy; excessive vitamin A supplementation should be avoided)
Vitamin E: Provides antioxidant protection against oxidative damage; found in nuts, seeds, and vegetable oils
Patients on GLP-1 therapy should be assessed for nutritional adequacy, particularly if experiencing significant gastrointestinal side effects that limit food intake. Referral to a registered dietitian may be beneficial for personalised nutritional planning. Supplementation with a multivitamin-mineral preparation may be considered under clinician or dietitian guidance during periods of rapid weight loss, particularly when dietary intake is limited, though this should not replace a varied, nutrient-dense diet.
Whilst cosmetic skin changes during weight loss are generally benign, certain presentations warrant medical evaluation. Patients should contact their GP or prescribing clinician if they experience:
Sudden onset of skin changes disproportionate to weight loss
Areas of skin that appear abnormally thin, fragile, or prone to tearing
Easy bruising or poor wound healing
Development of striae (stretch marks) during weight loss rather than weight gain
Skin changes accompanied by other symptoms such as muscle weakness, fatigue, or mood disturbances
Purple/wide striae with easy bruising and proximal muscle weakness (which may suggest Cushing's syndrome)
Seek same-day care or emergency help for severe allergic reactions, rapidly spreading rash, or unexplained extensive bruising or bleeding.
These features may indicate underlying conditions requiring investigation, such as nutritional deficiencies, endocrine disorders (particularly hypercortisolism), or connective tissue diseases. True dermal atrophy—characterised by visible loss of skin thickness with a translucent, cigarette paper-like appearance—differs from the redundant skin associated with fat loss and requires dermatological assessment.
Patients experiencing significant psychological distress related to skin changes should be offered appropriate support. Body image concerns are valid and can affect quality of life and treatment adherence. Discussion of realistic expectations before initiating GLP-1 therapy is important, acknowledging that substantial weight loss will result in visible body composition changes.
For individuals with severe skin laxity following major weight loss, referral to plastic surgery services may be appropriate once weight has stabilised for at least 12 to 18 months. The NHS may fund body contouring procedures in specific circumstances, typically when excess skin causes functional impairment, recurrent infections, or significant psychological distress, though criteria vary by integrated care board (ICB) and local NHS policies.
Regular monitoring during GLP-1 therapy should include assessment of nutritional status, physical function, and overall wellbeing, not solely metabolic parameters. A holistic approach ensures that the benefits of weight loss and improved glycaemic control are achieved whilst minimising adverse effects on skin health and patient quality of life.
Patients are encouraged to report any suspected side effects from GLP-1 medications via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
GLP-1 receptor agonists do not directly cause dermal thinning. Observed skin changes typically result from rapid weight loss and subcutaneous fat reduction, which can outpace the skin's natural capacity to contract and remodel.
Adequate protein intake (approximately 1.0–1.5 g/kg daily) supports collagen synthesis, whilst ensuring sufficient vitamin C, zinc, copper, and hydration (6–8 cups fluid daily) maintains dermal integrity during weight loss.
Contact your GP if you experience disproportionate skin thinning, easy bruising, poor wound healing, or skin changes accompanied by muscle weakness, fatigue, or other systemic symptoms that may indicate underlying nutritional or endocrine conditions.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.