
Hair loss with tirzepatide has emerged as a concern for patients using this dual GIP and GLP-1 receptor agonist for type 2 diabetes and weight management. Whilst tirzepatide (marketed as Mounjaro and Zepbound in the UK) delivers substantial metabolic benefits, some individuals experience hair thinning during treatment. This shedding typically represents telogen effluvium—a temporary, reversible condition triggered by rapid weight loss rather than a direct drug effect. Understanding the mechanisms, management strategies, and when to seek medical advice enables patients and clinicians to address this concern whilst maintaining the therapeutic benefits of tirzepatide.
Quick Answer: Hair loss with tirzepatide is typically temporary telogen effluvium caused by rapid weight loss rather than direct drug toxicity, affecting fewer than 1 in 100 people and usually resolving within 6–12 months.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereTirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist licensed for the treatment of type 2 diabetes mellitus and, more recently, chronic weight management in adults with obesity or overweight with weight-related comorbidities. It is marketed in the UK as Mounjaro for diabetes and Zepbound for weight management.
The medication works through a dual mechanism of action. By activating both GIP and GLP-1 receptors, tirzepatide enhances insulin secretion in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways. This combined action results in improved glycaemic control and substantial weight reduction.
Tirzepatide is administered as a once-weekly subcutaneous injection, with doses typically starting at 2.5 mg and gradually titrated upwards through 5 mg, 7.5 mg, 10 mg, 12.5 mg to a maximum dose of 15 mg, depending on individual response and tolerability. The Medicines and Healthcare products Regulatory Agency (MHRA) approved tirzepatide in the UK in 2022.
NICE has approved tirzepatide for type 2 diabetes in adults with inadequate glycaemic control (TA848) and for weight management in adults with a BMI of at least 35 kg/m² (or at least 30 kg/m² with weight-related comorbidities) who have high cardiovascular risk (TA946).
In the SURMOUNT-1 trial of people with obesity or overweight without diabetes, tirzepatide demonstrated average weight loss of 15–22% of body weight over 72 weeks, depending on the dose used.
Whilst tirzepatide has proven effective for metabolic management, patients and clinicians have increasingly reported hair thinning or shedding during treatment. Understanding whether this represents a direct drug effect or a consequence of rapid weight loss is essential for appropriate patient counselling and management.
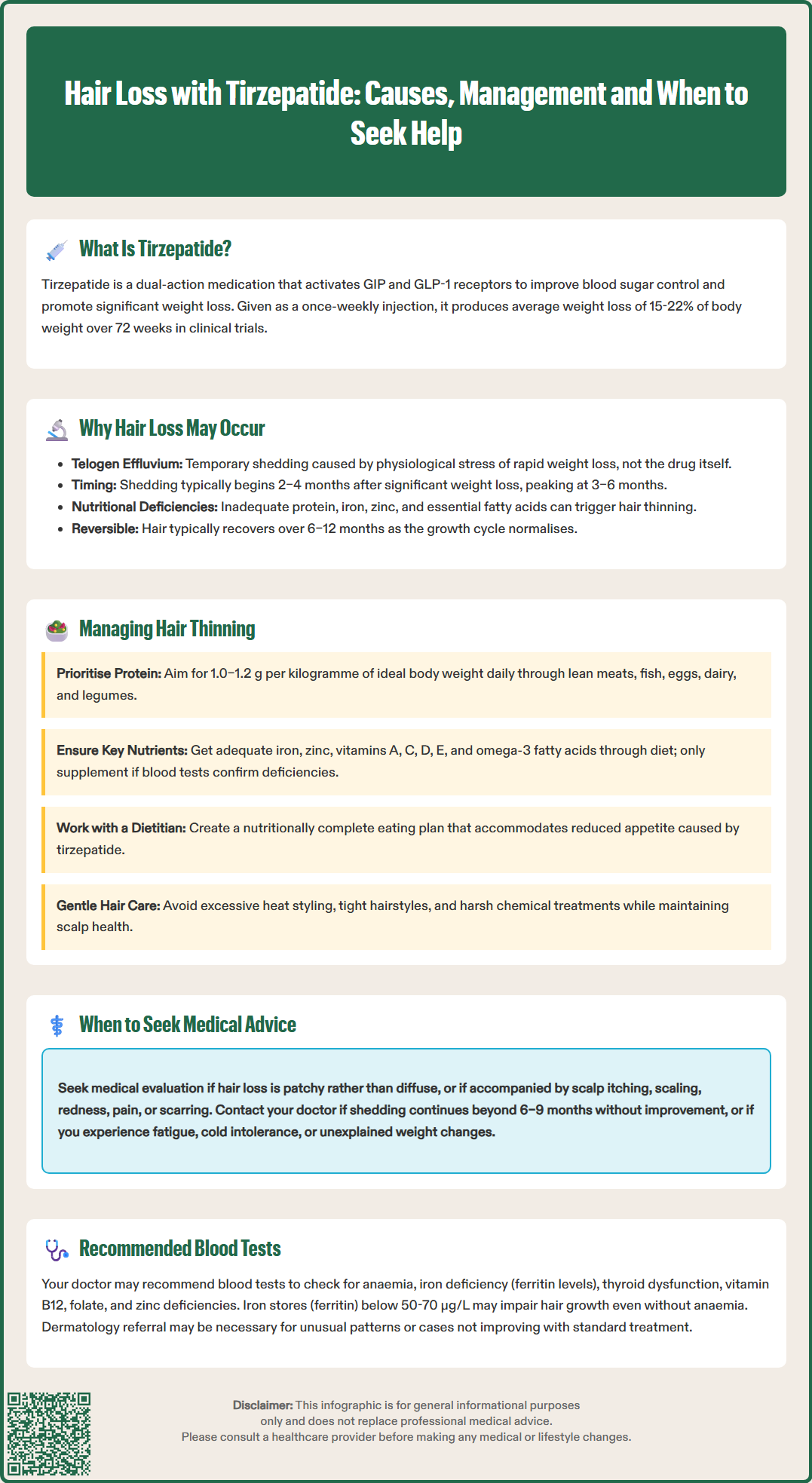
Hair loss associated with tirzepatide treatment is most commonly attributed to telogen effluvium, a form of temporary hair shedding triggered by physiological stress rather than a direct pharmacological effect of the medication itself. In the UK product information, alopecia is listed as an uncommon adverse reaction (affecting less than 1 in 100 people) for Zepbound (tirzepatide for weight management).
Telogen effluvium occurs when a significant proportion of hair follicles prematurely enter the telogen (resting) phase of the hair growth cycle, leading to diffuse shedding typically 2–4 months after the triggering event. Rapid or substantial weight loss represents a well-recognised trigger for this condition. The caloric restriction and metabolic changes associated with tirzepatide-induced weight reduction can create the physiological stress necessary to precipitate telogen effluvium.
Several mechanisms may contribute to hair thinning during weight loss treatment:
Nutritional deficiencies: Rapid weight loss may result in inadequate intake of protein, iron, zinc, and essential fatty acids—all crucial for healthy hair growth
Metabolic stress: Significant shifts in energy balance and hormonal regulation can disrupt the hair growth cycle
Reduced caloric intake: Severe energy restriction may divert bodily resources away from non-essential functions like hair growth
Protein malnutrition: Insufficient protein intake affects keratin production, the structural protein of hair
It is important to note that telogen effluvium is typically self-limiting and reversible. Hair shedding usually peaks around 3–6 months after the triggering event and gradually resolves over 6–12 months as the hair cycle normalises, even if weight loss continues at a more moderate pace.
Telogen effluvium should be distinguished from other causes of hair loss such as androgenetic alopecia (pattern hair loss), which may coexist and become more noticeable during periods of weight loss.
Patients experiencing hair thinning whilst taking tirzepatide can implement several evidence-based strategies to support hair health and potentially minimise shedding. The primary focus should be on optimising nutritional intake despite reduced appetite, which is a common effect of GLP-1 receptor agonist therapy.
Nutritional optimisation is paramount:
Protein intake: Aim for 1.0–1.2 g of protein per kilogram of ideal body weight daily as a general guide. High-quality protein sources include lean meats, fish, eggs, dairy products, legumes, and plant-based alternatives. Patients with kidney disease or other conditions may require individualised targets.
Iron: Ensure adequate iron intake through red meat, dark leafy greens, fortified cereals, and pulses. Women of reproductive age are particularly vulnerable to iron deficiency. Supplementation should only be considered if deficiency is confirmed by blood tests.
Micronutrients: Maintain sufficient levels of zinc (found in shellfish, meat, seeds), and vitamins A, C, D, and E. Avoid excessive supplementation without confirmed deficiencies.
Essential fatty acids: Include omega-3 sources such as oily fish, flaxseeds, and walnuts
Practical management strategies include:
Consider a comprehensive multivitamin supplement if dietary intake is significantly reduced, but avoid excessive doses of individual nutrients, particularly vitamin A, which can be toxic at high levels
Work with a registered dietitian to develop a nutritionally complete eating plan that accommodates reduced appetite
Avoid crash dieting or excessive caloric restriction beyond what occurs naturally with tirzepatide
Use gentle hair care practices: avoid excessive heat styling, tight hairstyles, and harsh chemical treatments
Maintain scalp health with gentle cleansing; scalp massage may provide comfort but has limited evidence for promoting hair regrowth
Patients should be reassured that hair shedding associated with weight loss is typically temporary and reversible. Continuing tirzepatide treatment as prescribed is generally appropriate, as the metabolic benefits usually outweigh the temporary cosmetic concern of hair thinning. However, if shedding is distressing, the pace of dose escalation can be discussed with the prescribing clinician.
If patients suspect hair loss may be a side effect of tirzepatide, they should report this through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Whilst telogen effluvium associated with weight loss is generally benign and self-limiting, certain presentations warrant medical evaluation to exclude alternative diagnoses or identify treatable underlying conditions. Patients should contact their GP or prescribing clinician if they experience any of the following:
Red flag features requiring assessment:
Patchy or localised hair loss rather than diffuse thinning—this may suggest alopecia areata or other dermatological conditions
Hair loss accompanied by scalp symptoms such as itching, scaling, redness, or pain, which could indicate infection or inflammatory scalp conditions
Signs of scarring alopecia including shiny scalp areas, loss of follicular openings, or permanent hair loss—these require urgent dermatology referral
Excessive or prolonged shedding continuing beyond 6–9 months without improvement
Associated symptoms including fatigue, cold intolerance, weight changes independent of tirzepatide, or other systemic features suggesting thyroid dysfunction or other endocrine disorders
Significant psychological distress affecting quality of life or treatment adherence
Recommended investigations may include:
Full blood count to assess for anaemia
Serum ferritin (iron stores)—local laboratory reference ranges should guide interpretation, though some specialists suggest levels below 50-70 μg/L may be suboptimal for hair growth even without anaemia
Thyroid function tests (TSH, free T4) to exclude hypothyroidism
Vitamin B12 and folate levels
Zinc levels if deficiency is suspected
Coeliac serology, particularly if iron deficiency is identified or hair loss persists
In women: consideration of hormonal assessment if features suggest polycystic ovary syndrome or other endocrine disorders
Clinicians should take a thorough medication history to identify other potential causes of hair loss, including recent changes to medications, and assess the pattern and duration of hair shedding. Referral to dermatology may be appropriate for atypical presentations, diagnostic uncertainty, or cases not responding to conservative management. The British Association of Dermatologists and NICE Clinical Knowledge Summaries provide guidance on investigating and managing hair loss disorders, which can inform specialist assessment when required.
No, hair loss associated with tirzepatide is typically temporary telogen effluvium that resolves within 6–12 months as the hair growth cycle normalises, even if weight loss continues at a moderate pace.
Generally no—the metabolic benefits of tirzepatide usually outweigh temporary hair thinning. Discuss concerns with your prescribing clinician, who may adjust the dose escalation pace whilst you optimise nutrition to support hair health.
Recommended investigations include full blood count, serum ferritin (iron stores), thyroid function tests, vitamin B12, folate, and potentially zinc levels or coeliac serology if deficiency or persistent hair loss is present.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.