
How do you know if you have a good metabolism? Understanding your metabolic health involves recognising how efficiently your body converts food into energy and maintains essential functions. Metabolism encompasses all biochemical processes that sustain life, from breathing and circulation to cellular repair. Whilst many people associate a 'good' metabolism with rapid calorie burning, true metabolic health reflects how effectively your body utilises nutrients, regulates energy balance, and responds to lifestyle factors. This article explores the signs of efficient metabolism, factors influencing metabolic rate, and when to seek medical assessment for metabolic concerns.
Quick Answer: A good metabolism is indicated by stable body weight, consistent energy levels, appropriate appetite regulation, and efficient nutrient utilisation rather than simply burning calories quickly.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMetabolism refers to the complex network of biochemical processes that occur within your body to maintain life. These processes convert the food and drink you consume into energy, which your body uses for everything from breathing and circulating blood to repairing cells and supporting physical activity. Your metabolic rate—the speed at which these processes occur—determines how many calories your body burns at rest and during activity.
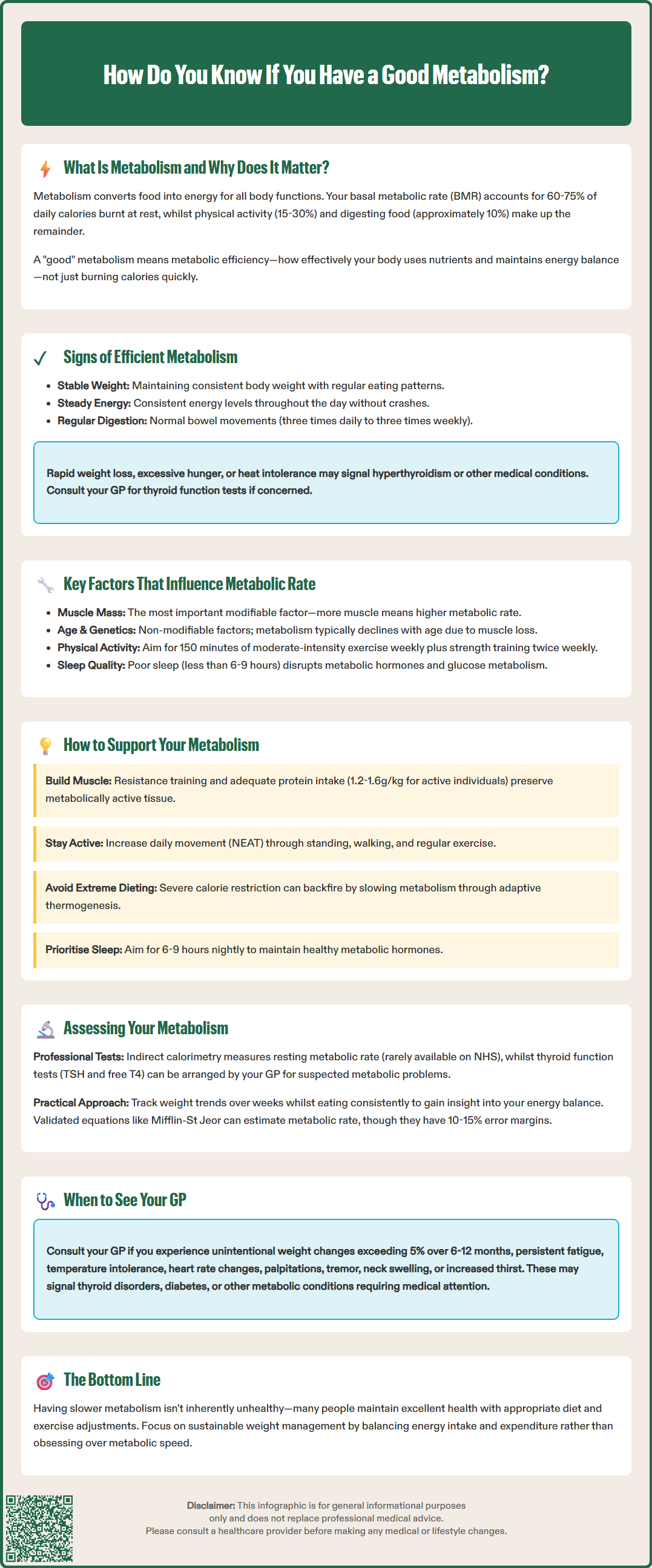
Your basal metabolic rate (BMR) accounts for approximately 60–75% of your total daily energy expenditure. This represents the minimum energy required to maintain essential physiological functions such as respiration, cardiac function, nervous system activity, and cellular metabolism. The remaining energy expenditure comes from physical activity (15–30%), including non-exercise activity thermogenesis (NEAT)—the energy expended for everything from fidgeting to standing—and the thermic effect of food—the energy required to digest, absorb, and process nutrients (approximately 10%).
Understanding your metabolism matters because it influences body weight regulation, energy levels, and overall health. A well-functioning metabolism efficiently converts nutrients into usable energy whilst maintaining stable blood glucose levels and supporting healthy body composition. Metabolic dysfunction can contribute to conditions such as obesity, type 2 diabetes, and metabolic syndrome—a cluster of conditions including increased blood pressure, elevated blood sugar, excess abdominal fat, and abnormal cholesterol levels that increase your risk of heart disease, stroke and type 2 diabetes.
Contrary to popular belief, having a 'good' metabolism is not simply about burning calories quickly. Rather, it reflects metabolic efficiency—how effectively your body utilises nutrients, maintains energy balance, and responds to dietary and lifestyle factors. The NHS emphasises that whilst metabolic rate varies between individuals, sustainable weight management depends more on the balance between energy intake and expenditure than on metabolic speed alone.
Identifying whether you have a fast or efficient metabolism involves observing several physical and physiological indicators, though it is important to note that these signs are not diagnostic and considerable individual variation exists.
Common indicators of a faster metabolic rate include:
Stable body weight despite regular food intake – If you maintain a healthy weight without significant dietary restriction, this may suggest your body efficiently balances energy intake with expenditure
Consistent energy levels throughout the day – People with efficient metabolism often experience sustained energy without dramatic peaks and troughs, particularly between meals
Body temperature perception – Some people with faster metabolism may feel warmer than others, though this is highly non-specific and can be affected by many factors unrelated to metabolic rate
Regular bowel function – Normal bowel frequency varies widely, ranging from three times a day to three times a week; persistent changes in bowel habits should be discussed with your GP, especially if accompanied by bleeding, pain or weight loss
Appetite regulation – While efficient metabolism may contribute to appropriate hunger and fullness signals, many factors influence appetite including sleep, stress, hormones and gut health
However, these observations must be interpreted cautiously. Rapid weight loss, excessive hunger, heat intolerance, or persistent high energy levels can also indicate hyperthyroidism or other endocrine disorders. Your GP can arrange thyroid function blood tests (TSH, free T4) in line with NICE guidance when clinically indicated.
Seek medical advice if you experience unexplained weight changes, palpitations, tremor, heat or cold intolerance, diarrhoea or constipation, neck swelling (goitre), or persistent fatigue. Urgent medical attention is needed for chest pain, severe breathlessness, or very fast/irregular heartbeat.
It is worth noting that having a slower metabolism is not inherently problematic. Many individuals with lower metabolic rates maintain excellent health through appropriate dietary adjustments and regular physical activity. Rather than self-diagnosing based on perceived metabolic rate, consult your GP for proper assessment if you have health concerns.
Metabolic rate is determined by a complex interplay of genetic, physiological, and lifestyle factors, many of which are modifiable through behavioural interventions.
Non-modifiable factors:
Age affects metabolism. Research suggests metabolic rate typically decreases gradually with age, largely due to loss of lean muscle mass (sarcopenia) and hormonal changes. This age-related decline partly explains why weight management often becomes more challenging with advancing years.
Biological sex influences metabolic rate, with men generally having higher BMR than women due to greater muscle mass and lower body fat percentage. However, this difference narrows after menopause when hormonal changes affect body composition in women.
Genetics play a substantial role in determining individual metabolic rates, with studies suggesting genetic factors contribute significantly to variation between individuals. Certain genetic variants affect thyroid hormone production, mitochondrial function, and fat oxidation capacity.
Modifiable factors:
Body composition is perhaps the most significant modifiable factor. Muscle tissue is metabolically active, burning more calories at rest than fat tissue. Resistance training and adequate protein intake help preserve or increase lean muscle mass.
Physical activity increases total daily energy expenditure both during exercise and afterwards. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity activity weekly, plus muscle-strengthening activities on at least two days a week. NEAT (non-exercise activity thermogenesis)—the energy expended during daily activities like standing, walking and fidgeting—can significantly impact total energy expenditure.
Dietary factors influence metabolism through several mechanisms. Severe calorie restriction can reduce metabolic rate as the body adapts to conserve energy—a phenomenon known as adaptive thermogenesis. The UK Reference Nutrient Intake (RNI) for protein is approximately 0.75g per kilogram body weight daily for adults. Higher protein intakes (1.2–1.6g/kg) may be appropriate for physically active individuals or during weight loss with resistance training, though people with kidney disease should seek medical advice before increasing protein intake.
Sleep quality and duration significantly affect metabolic hormones. Sleep deprivation disrupts leptin and ghrelin regulation, increases cortisol levels, and impairs glucose metabolism. The NHS advises that most adults need 6–9 hours of quality sleep nightly.
Thyroid function is crucial for metabolic regulation. Thyroid hormones (T3 and T4) regulate the metabolic rate of virtually every cell in the body. Both hypothyroidism and hyperthyroidism substantially alter energy expenditure and require medical management.
Several methods exist to assess metabolic rate, ranging from simple observational indicators to sophisticated laboratory testing. The appropriate approach depends on your specific concerns and whether underlying medical conditions are suspected.
Clinical assessment methods:
Indirect calorimetry represents the gold standard for measuring resting metabolic rate. This test measures oxygen consumption and carbon dioxide production whilst you rest. The results provide an accurate calculation of your BMR. However, this test is not routinely offered on the NHS unless there are specific clinical indications, and availability is limited.
Thyroid function tests are essential when metabolic dysfunction is suspected. Your GP can arrange blood tests measuring thyroid-stimulating hormone (TSH) and free T4; free T3 is measured in specific scenarios according to NICE guidance. Thyroid testing is indicated for unexplained weight changes, fatigue, or other symptoms suggesting thyroid disease. Normal TSH ranges are typically 0.4–4.0 mIU/L, though reference ranges may vary between laboratories.
Diabetes assessment may be appropriate if symptoms suggest dysglycaemia. Your GP may arrange HbA1c or fasting glucose tests if you experience symptoms such as increased thirst, frequent urination, recurrent infections, or unexplained weight loss.
Body composition analysis using bioelectrical impedance analysis (BIA) or dual-energy X-ray absorptiometry (DEXA) can assess muscle mass and body fat percentage, providing insight into metabolic capacity. Consumer BIA devices vary in accuracy and can be affected by hydration status. DEXA scanning is more accurate but is not routinely available through the NHS for metabolic assessment alone.
Practical self-assessment approaches:
You can estimate your BMR using validated equations such as the Mifflin-St Jeor formula, which considers age, sex, height, and weight. However, these calculations provide only estimates with potential error margins of 10–15%.
Monitoring your body weight trends over several weeks whilst maintaining consistent dietary intake can indicate whether your energy balance aligns with your metabolic rate. Stable weight suggests equilibrium between intake and expenditure.
When to seek medical advice:
Consult your GP if you experience unintentional weight loss or gain (more than 5% body weight over 6–12 months), persistent fatigue, heat or cold intolerance, changes in heart rate, increased thirst, frequent urination, or alterations in bowel habits. These symptoms may indicate thyroid disorders, diabetes, or other metabolic conditions requiring investigation.
The NHS provides comprehensive guidance on maintaining metabolic health through balanced nutrition, regular physical activity, adequate sleep, and stress management. Rather than focusing solely on metabolic speed, emphasis should be placed on overall metabolic health and sustainable lifestyle practices that support long-term wellbeing.
Common indicators include maintaining stable body weight despite regular food intake, consistent energy levels throughout the day, and appropriate hunger and fullness signals. However, these signs vary considerably between individuals and should be interpreted cautiously, as rapid weight loss or excessive hunger may indicate underlying medical conditions requiring GP assessment.
Whilst you can estimate basal metabolic rate using validated equations considering age, sex, height, and weight, these provide only estimates with potential error margins of 10–15%. Accurate metabolic testing requires indirect calorimetry, which measures oxygen consumption and carbon dioxide production, though this is not routinely available on the NHS unless clinically indicated.
Consult your GP if you experience unintentional weight changes exceeding 5% of body weight over 6–12 months, persistent fatigue, heat or cold intolerance, changes in heart rate, increased thirst, frequent urination, or alterations in bowel habits. These symptoms may indicate thyroid disorders, diabetes, or other metabolic conditions requiring investigation and appropriate management.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.