LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Saxenda (liraglutide 3.0 mg) is a prescription weight management medicine licensed in the UK for adults with obesity or those who are overweight with weight-related health conditions. As a once-daily injection used alongside diet and exercise, many patients wonder how long it takes to see results from Saxenda. Most people begin to notice measurable weight loss within 4 to 12 weeks of starting treatment, with more consistent results typically occurring after reaching the full maintenance dose. Understanding the timeline, factors affecting response, and how to maximise outcomes can help set realistic expectations and support successful weight management.
Quick Answer: Most patients begin to see measurable weight loss from Saxenda within 4 to 12 weeks of starting treatment, with more consistent results after reaching the full 3.0 mg maintenance dose.
Saxenda (liraglutide 3.0 mg) is a prescription medicine licensed in the UK for weight management in adults with obesity (BMI ≥30 kg/m²) or those who are overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, such as type 2 diabetes, hypertension, or dyslipidaemia. It is administered as a once-daily subcutaneous injection and is intended to be used alongside a reduced-calorie diet and increased physical activity.
Liraglutide belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists. It works by mimicking the action of GLP-1, a naturally occurring hormone released by the intestine after eating. GLP-1 acts on several areas of the body to regulate appetite and food intake. Specifically, Saxenda slows gastric emptying, which prolongs the feeling of fullness after meals, and acts on appetite centres in the brain to reduce hunger and increase satiety. This dual mechanism helps patients consume fewer calories without experiencing the intense hunger that often undermines weight loss efforts.
Unlike some weight loss medications that work primarily through stimulant effects or fat absorption inhibition, Saxenda's mechanism is more physiological, working with the body's natural appetite regulation systems. The medication does not directly burn fat or increase metabolism; rather, it facilitates adherence to a calorie-controlled diet by making it easier to eat less. Clinical trials have demonstrated that when combined with lifestyle modifications, Saxenda can lead to clinically significant weight loss compared to placebo.
Saxenda was centrally authorised in the EU in 2015 and is currently licensed in the UK. NHS access is highly restricted under NICE Technology Appraisal 664, which specifies that it should only be prescribed by specialist weight management services, with specific eligibility criteria, stopping rules, and a maximum treatment duration of 2 years.
Important safety considerations include: Saxenda is contraindicated in pregnancy and should be avoided during breastfeeding. It should not be used in combination with other GLP-1 receptor agonists. For patients with type 2 diabetes, there is a risk of hypoglycaemia when used with sulfonylureas or insulin, and dose adjustments of these medications may be needed.
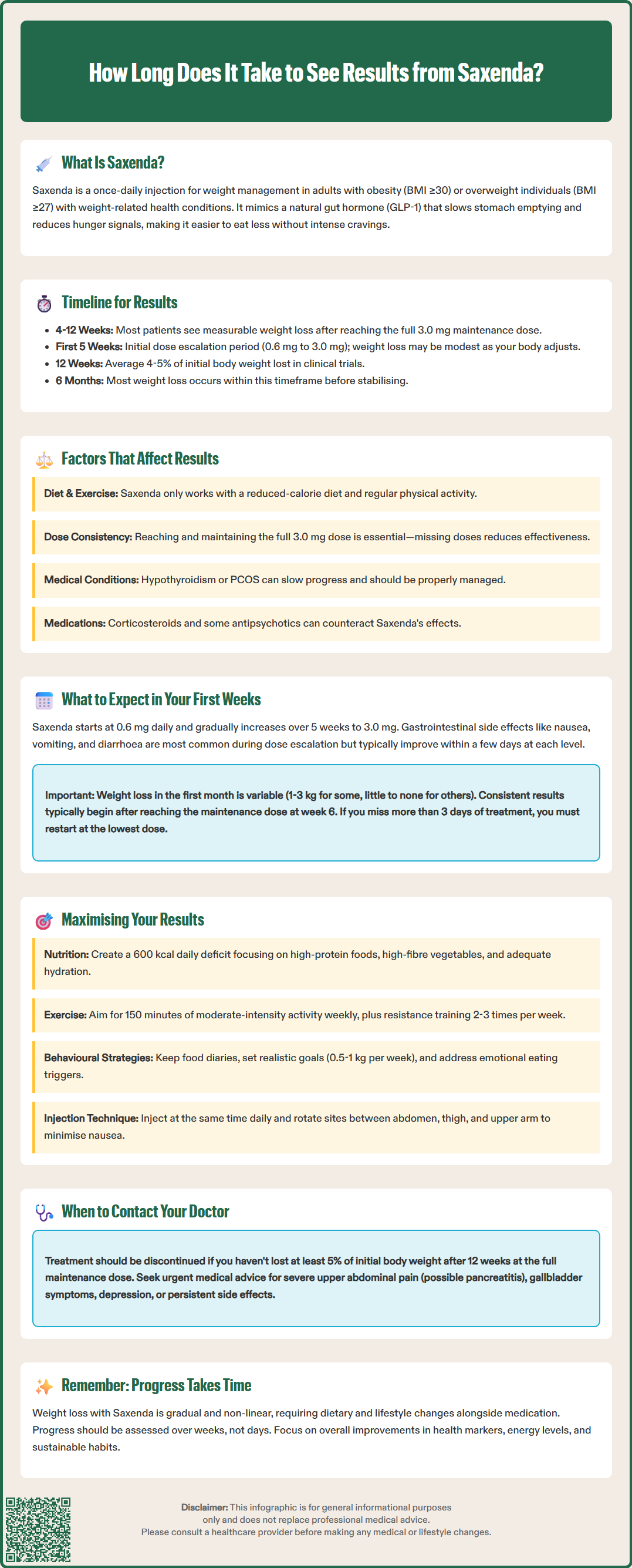
The timeline for seeing weight loss results with Saxenda varies between individuals, but most patients begin to notice measurable weight loss within 4 to 12 weeks of starting treatment, with more consistent results typically occurring after reaching the full maintenance dose. However, it is important to understand that Saxenda is not an immediate solution—weight loss occurs gradually as the medication is titrated up to the therapeutic dose and as dietary and lifestyle changes take effect.
During the initial dose escalation period (typically 5 weeks), patients gradually increase their daily dose from 0.6 mg to the full 3.0 mg maintenance dose. This titration schedule is designed to minimise gastrointestinal side effects such as nausea and vomiting. During this phase, some patients may experience modest weight loss, whilst others may see little change on the scales as their body adjusts to the medication.
Clinical trial data from the SCALE (Satiety and Clinical Adiposity—Liraglutide Evidence) programme provides useful benchmarks. In the pivotal SCALE Obesity and Prediabetes trial, participants lost an average of approximately 4-5% of their initial body weight by 12 weeks, with continued weight loss observed up to 56 weeks. The majority of weight loss typically occurs within the first 6 months of treatment, after which weight tends to stabilise if the medication and lifestyle modifications are maintained.
NICE guidance (TA664) recommends that treatment response should be assessed after 12 weeks at the full 3.0 mg maintenance dose. If a patient has not lost at least 5% of their initial body weight by this point, discontinuation of Saxenda should be considered, as further clinically meaningful weight loss is less likely. This threshold helps ensure that the medication is only continued in those who are deriving benefit from it. Patients should be aware that weight loss is rarely linear—fluctuations are normal, and progress should be assessed over weeks rather than days.
Several factors influence how quickly and effectively Saxenda produces weight loss results. Understanding these variables can help set realistic expectations and identify areas where additional support may be beneficial.
Adherence to lifestyle modifications is perhaps the most critical factor. Saxenda is licensed as an adjunct to a reduced-calorie diet and increased physical activity—it is not effective as a standalone treatment. Patients who consistently follow a structured eating plan with an appropriate calorie deficit and engage in regular physical activity typically see faster and more substantial results than those who rely on the medication alone. The medication makes it easier to adhere to these lifestyle changes by reducing hunger, but the changes themselves remain essential.
Starting weight and body composition also play a role. Individuals with higher initial BMI may lose weight more rapidly in absolute terms (kilograms lost), though percentage weight loss may be similar across BMI categories. Metabolic factors, including insulin resistance, thyroid function, and hormonal balance, can affect the rate of weight loss. Patients with untreated hypothyroidism or polycystic ovary syndrome (PCOS) may experience slower progress, and optimising management of these conditions is important for maximising benefit.
Medication adherence and dosing are crucial. Missing doses or failing to reach the full 3.0 mg maintenance dose can significantly reduce effectiveness. Some patients experience dose-limiting side effects that prevent them from reaching the therapeutic dose, which may compromise results. Concurrent medications can also be relevant—certain drugs, such as corticosteroids or some antipsychotics, can promote weight gain and may counteract Saxenda's effects. Importantly, Saxenda should not be used with other GLP-1 receptor agonists, and for patients with type 2 diabetes, dose adjustments of sulfonylureas or insulin may be needed to reduce the risk of hypoglycaemia.
Age and individual factors may contribute to variation in response. Older adults may experience slower weight loss due to reduced metabolic rate and muscle mass. Hormonal fluctuations in women (menstrual cycle, menopause) can affect water retention and perceived progress. Patients with a history of gallbladder disease or pancreatitis should be monitored closely, as GLP-1 receptor agonists have been associated with an increased risk of these conditions.
The initial weeks on Saxenda are primarily focused on dose escalation and tolerability rather than dramatic weight loss. Understanding what to expect during this period can help patients remain motivated and manage side effects effectively.
Week 1 begins with a starting dose of 0.6 mg once daily. At this low dose, most patients experience minimal appetite suppression, and weight loss is typically modest or absent. The primary goal is to allow the body to adjust to the medication. Some patients may notice mild gastrointestinal symptoms such as nausea, which is usually transient. Saxenda can be injected at any time of day, independent of meals, but it should be administered at approximately the same time each day. Many patients find that choosing a time that works with their routine helps minimise nausea.
During weeks 2 through 5, the dose is increased weekly (0.6 mg → 1.2 mg → 1.8 mg → 2.4 mg → 3.0 mg). As the dose increases, appetite suppression becomes more noticeable. Patients often report feeling fuller after smaller portions and experiencing reduced cravings between meals. Gastrointestinal side effects—including nausea, vomiting, diarrhoea, constipation, and abdominal discomfort—are most common during this escalation phase. These symptoms typically improve within a few days at each dose level. If side effects are troublesome, the titration can be slowed or the dose temporarily reduced to the previous level until tolerance improves.
Weight changes during the first month are variable. Some patients lose 1-3 kg, whilst others may see little change or even slight weight gain due to factors such as water retention or increased muscle mass from new exercise routines. This is normal and should not be cause for concern. Injection site reactions (redness, itching, bruising) may occur but are usually mild. Rotating injection sites between the abdomen, thigh, and upper arm can minimise this.
By week 6, most patients have reached the 3.0 mg maintenance dose and should begin to see more consistent weight loss, provided they are adhering to dietary and activity recommendations. If treatment is interrupted for more than 3 days, re-initiate at 0.6 mg and follow the titration schedule again to reduce the risk of gastrointestinal side effects. It is important to maintain regular contact with your prescribing clinician during this period to monitor progress, manage side effects, and adjust the treatment plan if necessary.
To achieve optimal results with Saxenda, patients should adopt a comprehensive approach that addresses diet, physical activity, behavioural factors, and ongoing medical support.
Dietary strategies are fundamental. A structured, reduced-calorie diet tailored to individual needs is essential. In line with NICE guidance (CG189), most patients benefit from a deficit of approximately 600 kcal per day below their maintenance requirements. This should be individually tailored by a healthcare professional or dietitian based on personal circumstances and medical history. Focus on:
High-protein foods (lean meats, fish, eggs, legumes) to preserve muscle mass and enhance satiety
High-fibre vegetables and whole grains to promote fullness and digestive health
Adequate hydration, especially if experiencing gastrointestinal symptoms
Limiting processed foods, added sugars, and alcohol, which provide empty calories and may trigger cravings
Physical activity should be gradually increased to at least 150 minutes of moderate-intensity exercise per week, as recommended by UK Chief Medical Officers. This might include brisk walking, cycling, swimming, or structured exercise classes. Resistance training 2-3 times weekly helps preserve lean muscle mass during weight loss, which is important for maintaining metabolic rate.
Behavioural and psychological support can significantly enhance outcomes. Consider:
Keeping a food and activity diary to identify patterns and maintain accountability
Setting realistic, specific goals (e.g., "lose 0.5-1 kg per week" rather than "lose weight quickly")
Addressing emotional eating triggers through cognitive behavioural techniques or professional counselling
Building a support network of family, friends, or weight management groups
Regular monitoring and medical follow-up are crucial. Attend scheduled appointments to assess progress, adjust treatment if needed, and screen for complications. Your healthcare provider should monitor blood pressure, blood glucose (especially if you have diabetes), and cardiovascular risk factors. If weight loss plateaus after initial success, your clinician may investigate underlying causes such as medication interactions, hormonal imbalances, or inadequate calorie deficit.
Important safety considerations: Saxenda is contraindicated in pregnancy and should be avoided during breastfeeding. It should not be used with other GLP-1 receptor agonists. For patients with type 2 diabetes using sulfonylureas or insulin, dose adjustments may be needed to prevent hypoglycaemia. Monitor for dehydration and acute kidney injury if experiencing persistent vomiting or diarrhoea.
When to seek advice: Contact your healthcare provider urgently if you experience severe or persistent upper abdominal pain radiating to the back (possible pancreatitis), signs of gallbladder disease (right upper abdominal pain, especially after fatty meals), or signs of depression or suicidal thoughts. If you have not lost at least 5% of your initial weight after 12 weeks at the full 3.0 mg dose, discuss with your prescriber whether continuing Saxenda is appropriate, as per NICE recommendations.
Suspected side effects should be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Most patients begin to notice measurable weight loss within 4 to 12 weeks of starting Saxenda, with more consistent results typically occurring after reaching the full 3.0 mg maintenance dose at week 5. Some modest weight loss may occur during the initial dose escalation period, though this varies between individuals.
NICE guidance recommends that if you have not lost at least 5% of your initial body weight after 12 weeks at the full 3.0 mg maintenance dose, discontinuation of Saxenda should be considered. Your prescriber will assess whether continuing treatment is appropriate, as further clinically meaningful weight loss is less likely if this threshold has not been met.
You cannot safely accelerate Saxenda's effects by increasing the dose beyond 3.0 mg daily, but you can optimise results by strictly adhering to a reduced-calorie diet (typically 600 kcal deficit), engaging in at least 150 minutes of moderate-intensity physical activity weekly, and addressing behavioural factors such as emotional eating. Regular medical follow-up and monitoring are essential for maximising outcomes.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.