How to prevent constipation with Ozempic is a common concern for patients prescribed this GLP-1 receptor agonist for type 2 diabetes. Constipation occurs because semaglutide slows gastric emptying and increases intestinal transit time, allowing more water reabsorption from stools. Whilst this mechanism aids glycaemic control, it can reduce bowel frequency and cause harder stools. Understanding why constipation develops enables proactive management through dietary modification, adequate hydration, regular physical activity, and establishing consistent toilet routines. This article provides evidence-based strategies to prevent and manage constipation whilst taking Ozempic, helping patients maintain treatment adherence and quality of life.
Quick Answer: Prevent constipation with Ozempic by increasing dietary fibre to 30g daily, maintaining adequate hydration of 1.5–2 litres of fluid, engaging in regular physical activity, and establishing consistent toilet routines.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. A different semaglutide formulation (Wegovy) is licensed for weight management. Whilst gastrointestinal side effects such as nausea and diarrhoea are more commonly reported, constipation is classified as a common side effect in the SmPC, particularly during dose escalation.
The mechanism underlying constipation relates to semaglutide's effect on gastric motility. GLP-1 receptor agonists slow gastric emptying and increase intestinal transit time, which is therapeutically beneficial for glycaemic control and satiety but can lead to reduced bowel frequency. This delayed transit allows more water to be reabsorbed from the stool in the colon, resulting in harder, more difficult-to-pass stools. Additionally, the appetite-suppressing effects of semaglutide may lead to reduced food and fluid intake, further contributing to constipation.
According to clinical trials, constipation occurs in a significant proportion of patients receiving semaglutide, with higher rates observed at weight management doses. The risk appears dose-dependent and is more pronounced during the initial titration phase. Patients with pre-existing bowel disorders or diabetic gastroparesis, those taking concurrent medications that slow gut motility (such as opioids, tricyclic antidepressants, calcium channel blockers, iron supplements, or antipsychotics), and older adults may be at increased risk.
Understanding this pharmacological mechanism is essential for both patients and healthcare professionals. Recognising that constipation is a predictable consequence of the drug's action—rather than an idiosyncratic reaction—enables proactive management strategies to be implemented from treatment initiation, thereby improving tolerability and adherence to therapy.
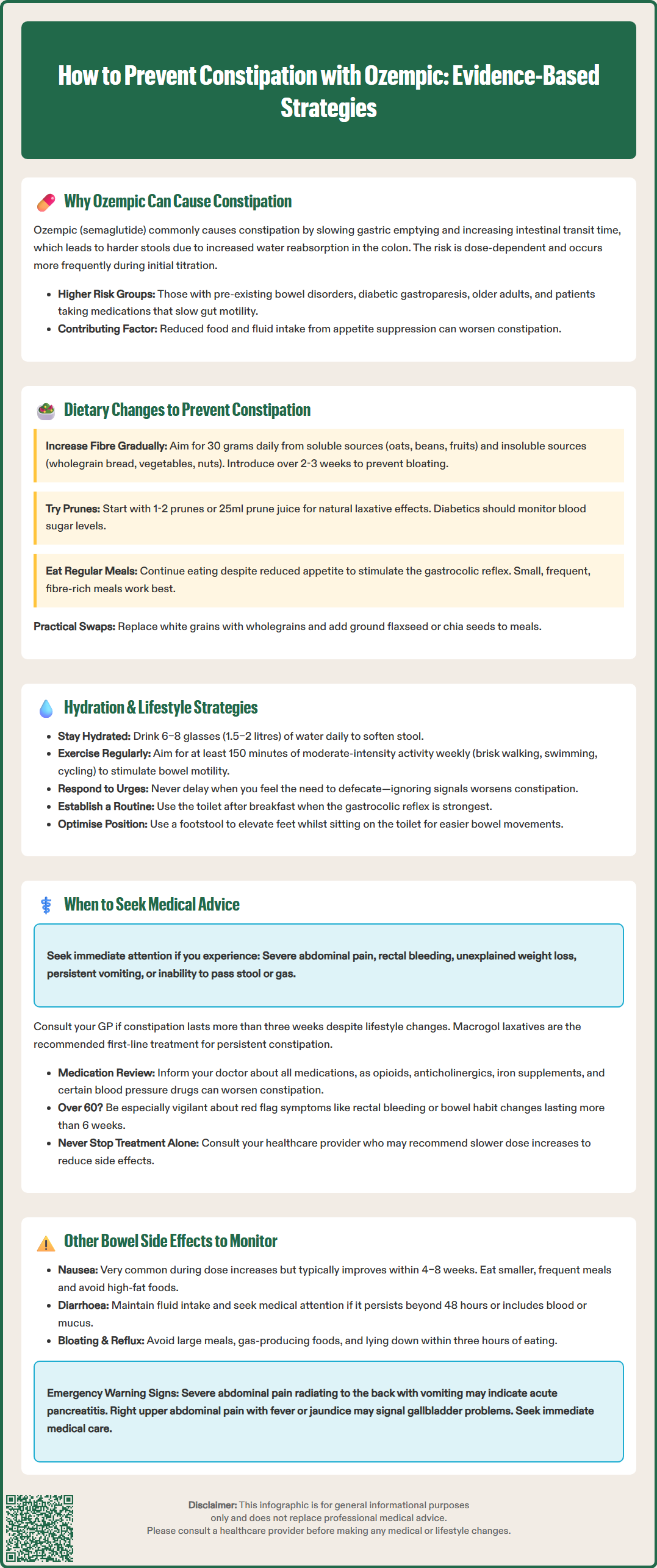
Dietary modification represents the cornerstone of constipation prevention for patients taking Ozempic. Increasing dietary fibre intake is the most evidence-based intervention, with a target of 30 grams daily recommended by the UK Scientific Advisory Committee on Nutrition (SACN) and promoted by the NHS. Soluble fibre (found in oats, beans, lentils, fruits such as apples and pears) and insoluble fibre (present in wholegrain bread, brown rice, vegetables, nuts, and seeds) both contribute to softer, bulkier stools that transit more easily through the colon.
Patients should introduce fibre gradually over 2–3 weeks to minimise bloating and abdominal discomfort, which can be exacerbated by Ozempic's effect on gastric emptying. Practical strategies include:
Replacing white bread, pasta, and rice with wholegrain alternatives
Adding a tablespoon of ground flaxseed or chia seeds to yoghurt or porridge
Consuming at least five portions of fruit and vegetables daily
Including pulses (chickpeas, lentils, kidney beans) in meals three to four times weekly
Choosing high-fibre breakfast cereals (those containing at least 6g fibre per 100g)
Prunes and prune juice may help due to their sorbitol content, which has a natural laxative effect. Starting with small amounts (1-2 prunes or 25ml of juice) and gradually increasing if needed may be beneficial. People with diabetes should be cautious with prune juice due to its sugar content and monitor blood glucose accordingly.
If dietary measures alone are insufficient, fibre supplements such as ispaghula husk may be considered, though these should be taken with plenty of fluid and may initially increase bloating.
It is important to note that whilst Ozempic reduces appetite, maintaining adequate nutritional intake remains essential. Patients should not skip meals entirely, as regular eating stimulates the gastrocolic reflex—a physiological response that promotes bowel movements. Small, frequent, fibre-rich meals may be better tolerated than larger portions and can help maintain regular bowel habits whilst managing the appetite-suppressing effects of semaglutide.
Adequate hydration is fundamental to preventing constipation in patients taking Ozempic. The NHS recommends consuming 6–8 glasses (approximately 1.5–2 litres) of fluid daily, though individual requirements vary based on body weight, activity level, and climate. Patients with conditions requiring fluid restriction (such as heart failure or kidney disease) should follow their clinician's specific advice. Water is the optimal choice, as it directly softens stool without adding calories. Patients should be particularly vigilant about fluid intake if they experience nausea or reduced appetite, as these semaglutide-related side effects may inadvertently lead to dehydration.
Timing of fluid consumption may help: drinking water upon waking might stimulate bowel activity for some people, whilst spreading fluid intake throughout the day maintains consistent hydration. Caffeinated beverages (tea, coffee) have a mild diuretic effect but can still contribute to overall fluid intake when consumed in moderation. Alcohol should be limited, as it promotes dehydration and may worsen constipation.
Regular physical activity significantly improves bowel motility and is strongly recommended for all patients on Ozempic. Exercise stimulates intestinal muscle contractions and reduces the time stool remains in the colon. The UK Chief Medical Officers' guidelines suggest at least 150 minutes of moderate-intensity activity weekly, which can be accumulated through:
Brisk walking for 30 minutes, five days per week
Swimming or cycling sessions
Gardening or active household tasks
Structured exercise classes
Establishing a regular toilet routine is equally important. Patients should respond promptly to the urge to defaecate rather than delaying, as ignoring this signal can worsen constipation. Setting aside time after breakfast, when the gastrocolic reflex is strongest, can help establish a predictable pattern. Adopting a squatting position (using a footstool to elevate the feet whilst seated on the toilet) optimises the anorectal angle and facilitates easier bowel movements.
Whilst mild constipation can often be managed with dietary and lifestyle modifications, certain symptoms warrant medical review. Patients should contact their GP or diabetes specialist nurse if constipation persists despite implementing preventative measures, particularly if it lasts more than three weeks or causes significant discomfort.
Red flag symptoms requiring urgent medical assessment include:
Severe abdominal pain or distension
Rectal bleeding (especially in those aged 60 or over)
Unexplained weight loss (beyond that expected from semaglutide therapy)
Persistent vomiting
Change in bowel habit lasting more than 6 weeks (especially in those over 60)
Symptoms suggesting bowel obstruction (severe pain, vomiting, complete inability to pass stool or gas)
These features may indicate complications or, rarely, underlying colorectal pathology requiring investigation in line with NICE suspected cancer pathways (NG12).
For persistent constipation without red flags, pharmacological management may be appropriate. Macrogol (polyethylene glycol) laxatives are generally recommended as first-line treatment. Glycerol suppositories may provide acute relief for some patients. Stimulant laxatives (senna, bisacodyl) should only be used short-term. Patients should consult a pharmacist or GP before starting any laxative, particularly if using for more than one week.
It is important to inform prescribers about all concurrent medications, as drug interactions may exacerbate constipation. Patients taking opioid analgesics, anticholinergic medications, iron supplements, or certain antihypertensives may require additional bowel management strategies. Regular medication reviews ensure that constipation is not being inadvertently worsened by polypharmacy, particularly in older adults or those with multiple comorbidities.
Patients should not alter or stop their semaglutide treatment without consulting their healthcare provider. In some cases, slower dose titration may improve tolerability whilst maintaining therapeutic benefit.
Beyond constipation, Ozempic is associated with a spectrum of gastrointestinal adverse effects that patients should be aware of. According to the SmPC, nausea is very common, affecting a significant proportion of patients, particularly during dose escalation. This typically improves over 4–8 weeks as tolerance develops. Eating smaller, more frequent meals and avoiding high-fat foods can help mitigate nausea. If severe or persistent, anti-emetic medication may be prescribed, though this should be discussed with a healthcare professional.
Diarrhoea is classified as a common side effect and may alternate with constipation in some individuals. Loose stools usually resolve within a few weeks but can lead to dehydration and electrolyte disturbances if severe. Patients experiencing diarrhoea should maintain fluid intake and consider oral rehydration solutions if symptoms persist beyond 48 hours. Persistent diarrhoea with blood, mucus, nocturnal symptoms or weight loss requires prompt medical evaluation to exclude other causes.
Abdominal pain and bloating are reported by patients taking semaglutide. These symptoms often relate to delayed gastric emptying and may be exacerbated by large meals or gas-producing foods (beans, cruciferous vegetables, carbonated drinks). Peppermint oil capsules or simethicone may provide symptomatic relief for some individuals.
Dyspepsia and gastro-oesophageal reflux can occur due to prolonged gastric retention. Patients should avoid lying down within three hours of eating and may benefit from raising the head of the bed. Persistent reflux symptoms may require proton pump inhibitor therapy.
Rarely, GLP-1 receptor agonists have been associated with acute pancreatitis. Patients should seek immediate medical attention if they develop severe, persistent abdominal pain radiating to the back, particularly if accompanied by vomiting. This serious adverse effect requires prompt recognition and discontinuation of semaglutide.
GLP-1 receptor agonists and rapid weight loss may also increase the risk of gallbladder problems. Right upper quadrant pain, especially with fever or jaundice, should prompt medical review.
Patients are encouraged to report any suspected adverse reactions to the MHRA Yellow Card Scheme. Regular monitoring and open communication with healthcare providers ensure that gastrointestinal side effects are appropriately managed, optimising both safety and treatment adherence.
Ozempic slows gastric emptying and increases intestinal transit time, allowing more water to be reabsorbed from stools in the colon, resulting in harder, more difficult-to-pass stools. The appetite-suppressing effects may also reduce food and fluid intake, further contributing to constipation.
High-fibre foods including wholegrain bread, brown rice, oats, beans, lentils, fruits, vegetables, nuts, and seeds help prevent constipation. Prunes and prune juice may also help due to their natural laxative effect from sorbitol content.
Seek medical advice if constipation persists for more than three weeks despite preventative measures, or immediately if you experience severe abdominal pain, rectal bleeding, unexplained weight loss, persistent vomiting, or symptoms suggesting bowel obstruction.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.