
Constipation is a common side effect of Ozempic (semaglutide), a GLP-1 receptor agonist used to treat type 2 diabetes in the UK. This occurs because semaglutide delays gastric emptying and reduces gastrointestinal motility, slowing bowel transit times. When lifestyle measures such as increased hydration and dietary fibre prove insufficient, stool softeners can provide effective relief. This article explores the best stool softener for Ozempic users, including docusate sodium and macrogol preparations, alongside practical guidance on safe use and supportive lifestyle strategies to maintain bowel health during treatment.
Quick Answer: Docusate sodium and macrogol preparations are commonly recommended stool softeners for Ozempic-related constipation, with choice depending on individual symptoms and response.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. A different semaglutide formulation, Wegovy, is licensed for weight management. Whilst effective in improving glycaemic control, gastrointestinal side effects are among the most commonly reported adverse reactions, with constipation affecting a significant proportion of users (classified as 'common' in the SmPC).
The mechanism underlying constipation relates to semaglutide's action on the gastrointestinal tract. GLP-1 receptor agonists delay gastric emptying and can reduce GI motility, which helps regulate postprandial glucose levels and promotes satiety. This effect may contribute to slower transit times throughout the digestive system. Additionally, semaglutide influences gut motility by modulating enteric nervous system activity.
Other contributing factors include reduced food and fluid intake—common when appetite is suppressed—which decreases stool bulk and moisture content. Dehydration, whether from reduced oral intake or concurrent diuretic use in patients with comorbidities, exacerbates the problem. The risk of constipation may be dose-dependent, often emerging or worsening during dose escalation phases.
Patients should be aware that whilst constipation is an expected side effect for some, it is manageable. Persistent or severe constipation—particularly if accompanied by abdominal pain, distension, nausea, vomiting, rectal bleeding, unintentional weight loss, or anaemia—warrants urgent medical review. People aged 60+ with a change in bowel habit lasting more than 6 weeks should also seek medical advice. Understanding the pharmacological basis of this side effect empowers patients to take proactive steps in managing their bowel health whilst continuing treatment.
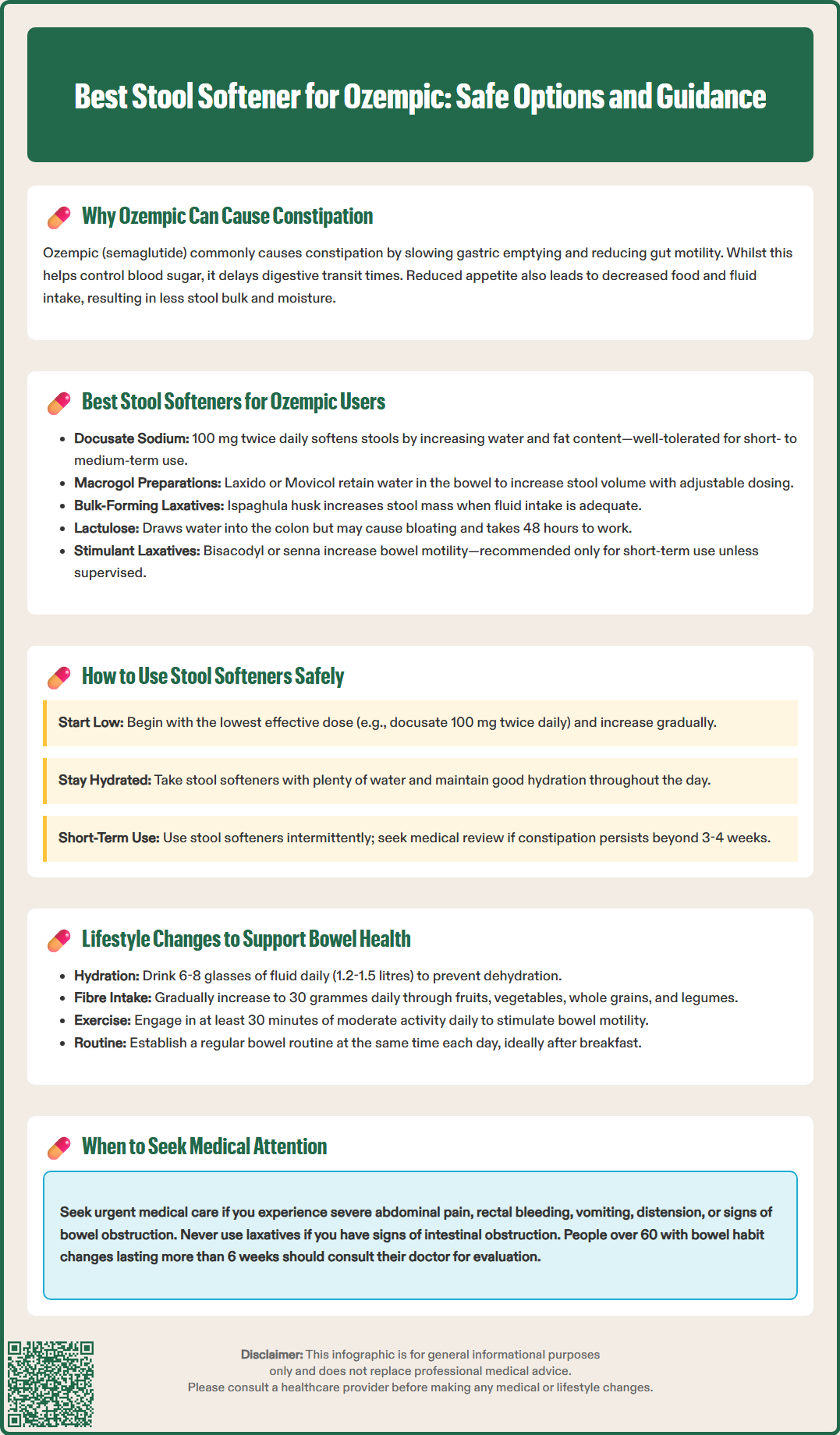
When lifestyle measures alone prove insufficient, stool softeners and laxatives can provide effective relief for Ozempic-related constipation. The choice of agent depends on individual circumstances, symptom severity, and concurrent medical conditions. In the UK, several options are available over the counter or on prescription.
Docusate sodium is a commonly recommended stool softener that works by increasing water and fat penetration into the stool, making it softer and easier to pass. According to the BNF, the typical adult oral dose is 100 mg twice daily (up to 100 mg three times daily if needed), with a maximum of 500 mg daily. It is generally well tolerated and suitable for short- to medium-term use. It is particularly useful for patients who experience hard, dry stools.
Macrogol (polyethylene glycol) preparations, such as Laxido or Movicol, are effective osmotic laxatives that retain water in the bowel, increasing stool volume and stimulating peristalsis. These are commonly used for constipation and the choice of laxative should be based on stool consistency and individual response. Macrogols are available in sachet form, dissolved in water, and dosing can be adjusted based on response.
Bulk-forming laxatives such as ispaghula husk (Fybogel) can be effective when fluid intake is adequate, particularly for small, hard stools. These work by increasing faecal mass to stimulate peristalsis.
Lactulose, another osmotic laxative, draws water into the colon and is widely used, though some patients find it causes bloating or flatulence. It may take 48 hours to produce an effect, making it less suitable for acute relief.
Bisacodyl and senna are stimulant laxatives that increase bowel motility. Whilst effective, they are generally recommended for short-term or intermittent use. They may be used longer-term under medical supervision if other options are ineffective.
Importantly, do not use laxatives if you have signs of intestinal obstruction or acute severe abdominal pain—seek urgent medical assessment instead. Patients should consult their GP or pharmacist before starting any laxative, particularly if they have underlying gastrointestinal conditions or are taking other medications.
Safe and effective use of stool softeners alongside Ozempic requires attention to dosing, timing, and monitoring for potential interactions or adverse effects. Patients should always read the patient information leaflet and seek professional advice if uncertain.
When initiating a stool softener, start with the lowest effective dose and increase gradually if needed. For example, docusate sodium may be started at 100 mg twice daily, adjusting according to response and following the patient information leaflet. Macrogol sachets can similarly be titrated—beginning with one sachet daily and adjusting based on stool consistency and frequency. The goal is to achieve soft, formed stools that pass comfortably, rather than inducing diarrhoea.
Timing of administration can influence efficacy. Stool softeners are generally taken with water, and adequate hydration throughout the day enhances their action. There are no known direct interactions between semaglutide and common laxatives. While semaglutide delays gastric emptying, this rarely causes clinically significant issues with most oral medicines. However, if you take warfarin, your INR should be monitored when starting or changing semaglutide treatment.
Duration of use should be reviewed regularly. Stool softeners are typically intended for short-term relief or intermittent use. If constipation persists beyond 3-4 weeks despite treatment, medical review is essential to exclude other causes and consider alternative management strategies.
Patients should monitor for adverse effects, including abdominal cramping, diarrhoea, or worsening nausea. Macrogols with added electrolytes have a low risk of electrolyte disturbances, but caution is advised with prolonged use of stimulant or saline osmotic laxatives. If severe abdominal pain, rectal bleeding, vomiting, distension, or signs of bowel obstruction develop, seek urgent medical attention. Pregnant or breastfeeding women, and those with inflammatory bowel disease or other gastrointestinal disorders, require individualised advice before using laxatives.
Report any suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Non-pharmacological strategies form the foundation of managing constipation in Ozempic users and should be implemented alongside or before considering stool softeners. These measures address the underlying causes of reduced bowel motility and can significantly improve symptoms.
Adequate hydration is paramount. The NHS recommends 6-8 drinks a day (approximately 1.2-1.5 litres), unless fluid restriction is medically indicated. Dehydration worsens constipation by reducing stool moisture content. Patients often reduce fluid intake inadvertently when appetite is suppressed, so conscious effort to maintain hydration is important. Herbal teas and diluted fruit juices can contribute to fluid intake, while moderate consumption of caffeinated beverages and alcohol is advised.
Dietary fibre plays a crucial role in promoting regular bowel movements. Gradually increase intake of soluble and insoluble fibre through fruits, vegetables, whole grains, legumes, and seeds. The UK Scientific Advisory Committee on Nutrition recommends 30 grams of fibre daily for adults. Soluble fibre (found in oats, apples, and beans) softens stools, whilst insoluble fibre (in wheat bran, nuts, and vegetables) adds bulk and stimulates peristalsis. Introduce fibre slowly to minimise bloating and ensure adequate fluid intake to prevent worsening constipation.
Regular physical activity stimulates bowel motility. Even moderate exercise—such as brisk walking for 30 minutes daily—can improve gastrointestinal transit times. Patients should incorporate movement into their daily routine, particularly after meals when the gastrocolic reflex naturally promotes bowel activity.
Establishing a bowel routine can be beneficial. Allocate time each day, ideally after breakfast, to sit on the toilet without rushing, allowing the body to respond to natural urges. Avoid ignoring the urge to defaecate, as this can worsen constipation over time.
Finally, review medications with your GP, as other drugs (such as opioids, anticholinergics, or iron supplements) may contribute to constipation. Seek medical advice if you experience unexplained weight loss, iron-deficiency anaemia, rectal bleeding, or a persistent change in bowel habit for more than 6 weeks (particularly if you're aged 60+). If lifestyle modifications and stool softeners fail to provide relief, or if constipation significantly impacts quality of life, discuss alternative treatment options with your healthcare provider.
Ozempic (semaglutide) delays gastric emptying and reduces gastrointestinal motility, slowing bowel transit times. Reduced food and fluid intake due to appetite suppression further decreases stool bulk and moisture, contributing to constipation.
Yes, docusate sodium is commonly used alongside Ozempic for constipation relief. There are no known direct interactions, but consult your GP or pharmacist before starting any laxative, particularly if you have underlying conditions or take other medications.
Seek urgent medical review if you experience severe abdominal pain, distension, vomiting, rectal bleeding, unintentional weight loss, or anaemia. People aged 60+ with a change in bowel habit lasting more than 6 weeks should also consult their GP.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.