Injecting tirzepatide in the stomach is a straightforward process that many patients with type 2 diabetes or obesity perform weekly at home. Tirzepatide, available as Mounjaro for diabetes and under licence for weight management, is a dual GIP and GLP-1 receptor agonist administered subcutaneously via a pre-filled pen device. Proper injection technique, including correct site selection on the abdomen and systematic rotation, ensures optimal medication absorption whilst minimising discomfort and complications. This guide provides evidence-based advice on safe administration, site selection, managing side effects, and practical tips to improve your injection experience, aligned with UK prescribing information and NHS guidance.
Quick Answer: Tirzepatide should be injected subcutaneously into the abdomen at least 5 cm away from the navel, using proper technique with a pre-filled pen device once weekly.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereTirzepatide is a once-weekly injectable medication licensed in the UK for the treatment of type 2 diabetes mellitus (as Mounjaro) and, more recently, for weight management in adults with obesity or overweight with weight-related comorbidities (as Wegovy). It represents a novel class of medication known as a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist.
The mechanism of action of tirzepatide involves simultaneous activation of both GIP and GLP-1 receptors, which are naturally occurring incretin hormones that play crucial roles in glucose homeostasis and appetite regulation. By stimulating GLP-1 receptors, tirzepatide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriately elevated glucagon secretion, and slows gastric emptying. The additional GIP receptor activation may contribute to its effects, though the precise mechanisms of GIP action in humans are still being elucidated.
Clinical trials have demonstrated that tirzepatide produces significant reductions in HbA1c levels (a measure of long-term blood glucose control) and substantial weight loss. The SURPASS clinical trial programme for type 2 diabetes showed HbA1c reductions of up to 2.5% and weight loss averaging 7–12 kg, depending on the dose used. The medication is administered subcutaneously (under the skin) once weekly, with doses ranging from 2.5 mg to 15 mg, with 2.5 mg being a starting dose to improve tolerability rather than for glycaemic efficacy.
Importantly, tirzepatide is not indicated for type 1 diabetes or diabetic ketoacidosis and should not be used in combination with other GLP-1 receptor agonists. The MHRA-approved prescribing information emphasises that tirzepatide should be used alongside a reduced-calorie diet and increased physical activity for optimal therapeutic benefit.
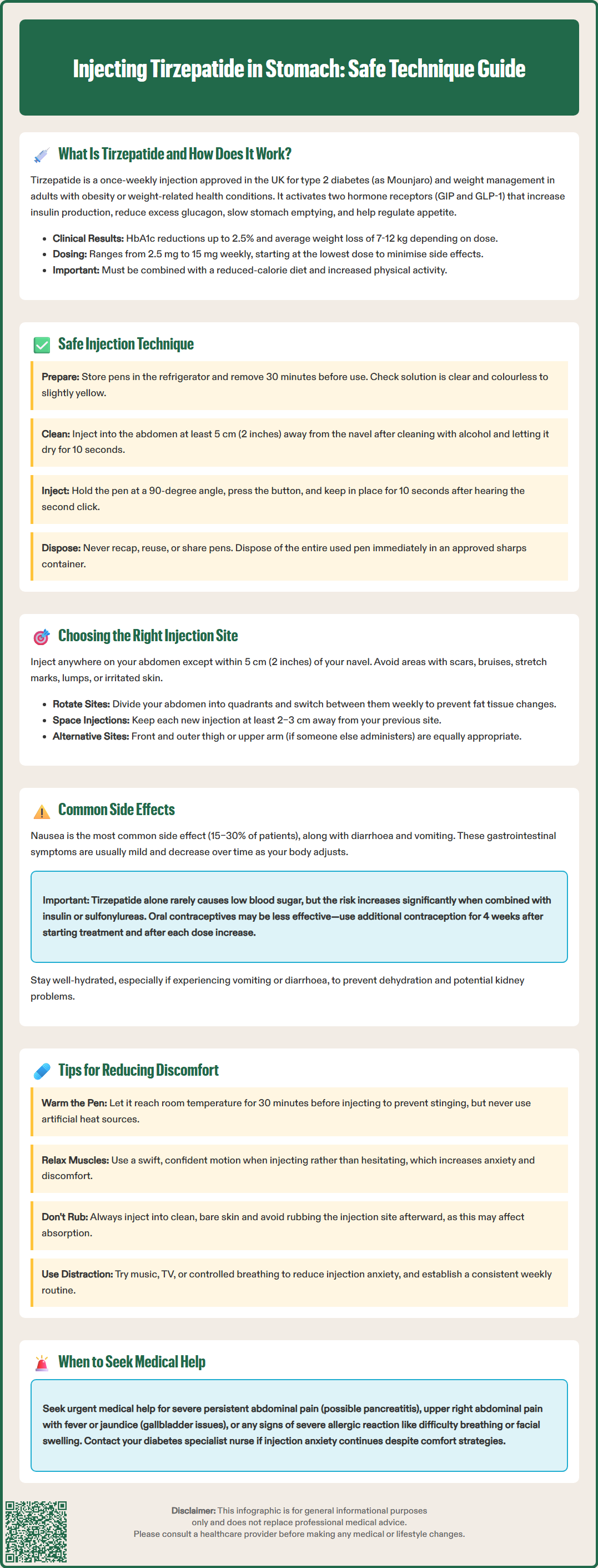
Administering tirzepatide via subcutaneous injection into the abdominal area is a straightforward process, but proper technique is essential to ensure medication efficacy and minimise complications. Tirzepatide is supplied in a pre-filled, single-dose pen device that simplifies the injection process for patients self-administering at home.
Step-by-step injection technique:
Prepare your materials: Gather your tirzepatide pen (stored in the refrigerator until 30 minutes before use), an alcohol wipe, and a sharps disposal container. Wash your hands thoroughly with soap and water.
Inspect the medication: Check the solution through the pen window—it should be clear and colourless to slightly yellow. Do not use if the liquid appears cloudy, discoloured, or contains particles.
Clean the injection site: Select an area on your abdomen at least 5 cm (2 inches) away from your navel. Wipe the area with an alcohol swab and allow it to dry completely (approximately 10 seconds).
Administer the injection: Remove the pen cap, place the pen firmly against your skin at a 90-degree angle, and press the injection button. Hold the pen in place until you hear the second click and/or see the plunger indicator has moved completely, then continue holding for about 10 seconds to ensure the full dose has been delivered.
Dispose safely: Do not recap the pen. Place the entire used pen directly into an approved sharps container. Never reuse pens or share them with others, even if the needle is changed.
The NHS advises that if you miss a dose and it has been less than four days since your scheduled injection, administer it as soon as you remember. If more than four days have passed, skip the missed dose and resume your regular schedule. Contact your GP or diabetes specialist nurse if you have questions about missed doses or injection technique.
For sharps disposal, obtain a proper sharps bin from your GP, pharmacy, or local council, and follow local guidelines for returning filled containers.
Selecting appropriate injection sites on your abdomen is crucial for optimal medication absorption, comfort, and prevention of injection-site complications. The abdomen is a commonly used injection site for tirzepatide due to its large surface area, consistent subcutaneous fat layer, and convenient accessibility for self-administration.
Recommended abdominal injection zones:
The ideal injection area encompasses the entire abdomen, excluding a 5 cm (2-inch) radius around the navel (umbilicus). This exclusion zone is important because the tissue near the navel has different vascularity and may result in unpredictable absorption. The best sites are typically in the lower abdomen or the sides (flanks), where there is adequate subcutaneous fat tissue. Avoid areas with scars, bruises, stretch marks, lipohypertrophy (lumps of fatty tissue), lipoatrophy (loss of fat tissue), or any skin that is tender, hardened, inflamed, or infected, as these may affect medication absorption or cause discomfort.
Site rotation strategy:
Systematic rotation of injection sites is essential to prevent lipohypertrophy or lipoatrophy, both of which can impair medication absorption and glycaemic control. Healthcare professionals recommend dividing your abdomen into quadrants and rotating between them weekly. For example, if you inject on the right lower abdomen one week, move to the left lower abdomen the following week, then to the right upper abdomen, and so forth. Keep each new injection at least 2–3 cm away from the previous site.
Alternative injection sites include the thigh (front and outer aspects) and the upper arm (if administered by another person). According to the UK prescribing information, all these sites are appropriate for tirzepatide administration. NICE guidance on injectable diabetes medications emphasises the importance of proper injection technique training, which should be provided by your diabetes specialist nurse or practice nurse at initiation and reviewed periodically to ensure continued competence and prevent complications.
Like all medications, tirzepatide can cause side effects, though not everyone experiences them. Understanding potential adverse effects helps patients recognise normal responses versus concerning symptoms requiring medical attention. The most frequently reported side effects are gastrointestinal in nature and typically occur during dose initiation or escalation.
Gastrointestinal effects:
Nausea is the most common side effect, affecting approximately 15–30% of patients in clinical trials, particularly during the first few weeks of treatment. Other frequent gastrointestinal symptoms include diarrhoea (13–22%), vomiting (6–10%), constipation, abdominal pain, and reduced appetite. These effects are generally mild to moderate in severity and tend to diminish over time as the body adjusts to the medication. The MHRA-approved prescribing information recommends starting at the lowest dose (2.5 mg) and gradually increasing every four weeks to improve tolerability.
Injection-site reactions:
Local reactions at the injection site are relatively uncommon but may include redness, itching, swelling, or mild discomfort. These typically resolve within a few days without intervention. Proper injection technique and site rotation significantly reduce the likelihood of persistent local reactions.
Hypoglycaemia risk:
When used as monotherapy, tirzepatide carries a low risk of hypoglycaemia (low blood sugar) due to its glucose-dependent mechanism of action. However, the risk increases substantially when combined with insulin or sulfonylureas. Your doctor may need to reduce the doses of these medications when starting or increasing tirzepatide. Patients should be educated about hypoglycaemia symptoms (trembling, sweating, confusion, rapid heartbeat) and management strategies.
Important warnings:
Tirzepatide may reduce the absorption of oral medications, including oral contraceptives. If you use oral contraceptives, additional contraceptive methods are advised for 4 weeks after starting tirzepatide and after each dose increase.
Maintain adequate hydration while taking tirzepatide, especially if experiencing vomiting or diarrhoea, to reduce the risk of dehydration and potential kidney problems.
If you have diabetic retinopathy, rapid improvements in blood glucose may temporarily worsen this condition; regular eye examinations are important.
Tirzepatide should be avoided during pregnancy and breastfeeding; effective contraception is recommended during treatment.
When to seek medical advice:
Stop taking tirzepatide and contact your GP or diabetes team urgently if you experience severe, persistent abdominal pain (which may indicate pancreatitis), signs of gallbladder disease (pain in the upper right abdomen, fever, yellowing of skin or eyes), or symptoms of thyroid issues (lump in the neck, difficulty swallowing, persistent hoarseness). Call 999 or go to A&E immediately for signs of severe allergic reaction, including difficulty breathing, severe rash, or facial swelling. For other urgent concerns, contact NHS 111 for advice.
Report any suspected side effects to the MHRA Yellow Card Scheme at yellowcard.mhra.gov.uk or via the Yellow Card app.
Many patients initially feel apprehensive about self-injecting medication, but with proper technique and practical strategies, the process can become routine and virtually painless. Implementing evidence-based comfort measures significantly improves the injection experience and promotes long-term treatment adherence.
Temperature considerations:
Allow your tirzepatide pen to reach room temperature before injecting, as cold medication can cause stinging or discomfort. Remove the pen from the refrigerator approximately 30 minutes before your scheduled injection time. According to the UK SmPC, tirzepatide can be stored at room temperature (below 30°C) for up to the period specified in the product information, which may be helpful for travel or convenience. Never attempt to warm the pen artificially using hot water, microwaves, or direct sunlight, as this may damage the medication.
Injection technique refinements:
Relax your abdominal muscles: Tension increases discomfort. Sit or stand in a comfortable position and take several deep breaths before injecting.
Use a swift, confident motion: Hesitation often increases anxiety and discomfort. Once you've positioned the pen, press it firmly against your skin and activate the injection button decisively.
Consider a gentle skin fold: For very lean individuals, creating a gentle skin fold may help ensure the medication is delivered into subcutaneous tissue rather than muscle. However, for most people using auto-injector pens, this is not necessary—simply hold the pen flat against the skin.
Don't inject through clothing: Always inject into clean, bare skin to ensure proper medication delivery and reduce infection risk.
Post-injection care:
Avoid rubbing the injection site immediately after administration, as this may affect medication absorption. If minor bleeding occurs, apply gentle pressure with a clean tissue or gauze. A small amount of bleeding or bruising is normal and not concerning.
Psychological strategies:
Distraction techniques such as listening to music, watching television, or focusing on controlled breathing can reduce injection anxiety. Some patients find it helpful to establish a consistent routine, injecting at the same time and place each week. If injection anxiety persists despite these measures, discuss your concerns with your diabetes specialist nurse, who can provide additional support and may suggest alternative administration techniques or psychological interventions to improve your comfort and confidence.
Inject tirzepatide at least 5 cm (2 inches) away from your navel to ensure proper absorption. The tissue near the umbilicus has different vascularity that may result in unpredictable medication absorption.
Yes, systematic rotation between abdominal quadrants is essential to prevent lipohypertrophy or lipoatrophy. Keep each new injection at least 2–3 cm away from the previous site and rotate weekly between different areas of your abdomen.
Nausea is common, affecting 15–30% of patients, particularly during initial treatment. It typically diminishes over time as your body adjusts. Maintain adequate hydration, eat smaller meals, and contact your GP or diabetes team if symptoms are severe or persistent.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.