
When is the best time to inject tirzepatide? This is a common question for patients prescribed this once-weekly medication for type 2 diabetes. Tirzepatide, marketed as Mounjaro in the UK, offers considerable flexibility in administration timing—it can be injected at any time of day, with or without meals. However, maintaining consistency by injecting on the same day each week is essential for optimal therapeutic effect. Understanding the practical considerations around timing, including strategies to manage side effects and proper injection technique, helps patients integrate this treatment safely into their daily routines whilst maximising glycaemic control and treatment adherence.
Quick Answer: Tirzepatide can be injected at any time of day, with or without meals, but must be administered consistently on the same day each week to maintain therapeutic levels.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereTirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It is administered as a once-weekly subcutaneous injection and is marketed under the brand name Mounjaro in the UK. In some non-UK jurisdictions, tirzepatide is also approved for weight management (under the brand name Zepbound in the US), but this is not currently a licensed indication in the UK.
The dual mechanism of action distinguishes tirzepatide from single GLP-1 receptor agonists. By activating both GIP and GLP-1 receptors, tirzepatide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriate glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways. This combined effect results in improved glycaemic control and substantial weight reduction in clinical trials, with mean weight loss exceeding 15% in some studies of the SURMOUNT and SURPASS trial programmes.
Tirzepatide is typically initiated at a low dose (2.5 mg weekly) and gradually titrated upwards every four weeks to minimise gastrointestinal side effects whilst optimising therapeutic benefit. Maximum doses range from 10 mg to 15 mg weekly, depending on individual response and tolerability. The medication is prescribed alongside lifestyle modifications including dietary changes and increased physical activity. NICE guidance (NG28) supports the use of GLP-1 receptor agonists in type 2 diabetes management when metformin and other oral agents prove insufficient, though specific tirzepatide guidance continues to evolve as real-world evidence accumulates.
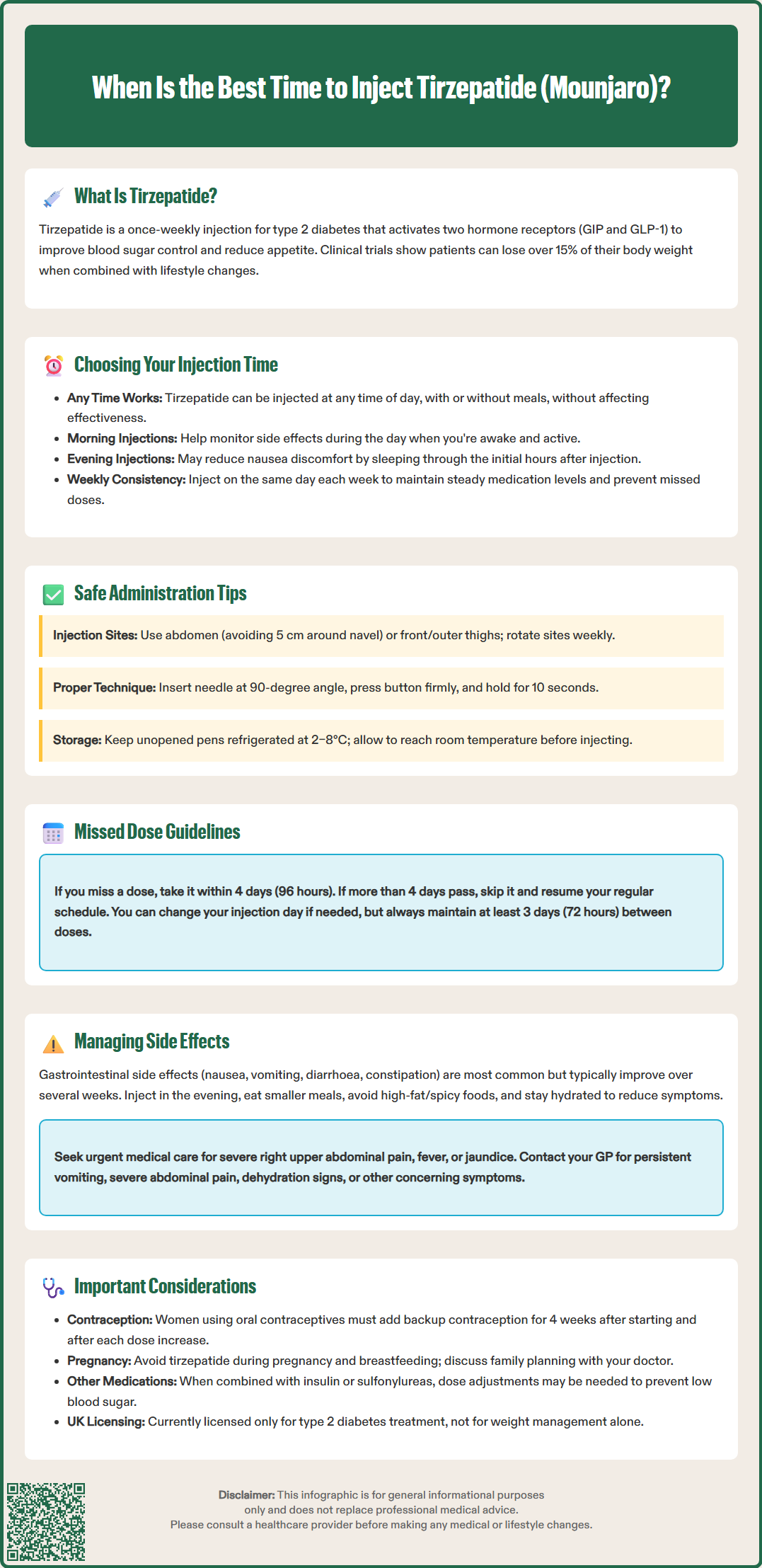
Flexibility in timing is one of tirzepatide's practical advantages. The medication can be administered at any time of day, with or without meals, providing patients considerable freedom to integrate injections into their daily routines. There is no official requirement to inject at a specific time, and clinical efficacy remains consistent regardless of whether the dose is given in the morning, afternoon, or evening.
However, consistency is paramount. Patients should aim to inject tirzepatide on the same day each week to maintain steady therapeutic levels and establish a reliable routine that reduces the risk of missed doses. Many patients find it helpful to link their injection day to a memorable weekly event or use smartphone reminders to ensure adherence.
Practical considerations may influence individual timing preferences:
Morning administration allows patients to monitor for any immediate side effects during waking hours and may align better with healthcare appointments if dose adjustments are needed.
Evening injections might be preferred by those who experience mild nausea, as sleeping through the initial hours post-injection can improve comfort.
Meal timing is not critical, but some patients prefer injecting before a lighter meal if gastrointestinal symptoms are problematic.
If a dose is missed, the UK SmPC recommends administering it as soon as possible within 4 days (96 hours) after the missed dose. If more than 4 days have passed, the missed dose should be skipped and the next dose administered on the regularly scheduled day. The injection day can be changed if necessary, ensuring at least 3 days (72 hours) between doses. Patients uncertain about missed dose management should contact their GP or diabetes specialist nurse for personalised advice.
Tirzepatide is supplied in pre-filled, single-dose pens designed for subcutaneous injection into areas with adequate subcutaneous tissue. Approved injection sites for self-administration include the abdomen (avoiding a 5 cm radius around the navel) and the front and outer aspects of the thighs. The upper outer arms may be used only when the injection is administered by a caregiver or another person. Rotating injection sites within these areas helps prevent lipodystrophy—localised changes in subcutaneous fat that can affect medication absorption and cause cosmetic concerns.
Proper injection technique is essential for optimal drug delivery and patient safety:
Preparation: Wash hands thoroughly and inspect the pen for damage or discolouration. The solution should be clear and colourless; do not use if cloudy or containing particles. Allow the pen to reach room temperature before injection if previously refrigerated.
Site selection: Choose a different injection site from the previous week, ensuring the skin is clean and dry. Avoid areas that are tender, bruised, scarred, or inflamed.
Injection process: Pinch the skin gently, insert the needle at a 90-degree angle, and press the injection button firmly. Hold for approximately 10 seconds to ensure complete dose delivery before withdrawing the needle. Ensure you inject under the skin and not into a vein or muscle.
Disposal: Place used pens immediately into a sharps container. Never share pens between patients, even if the needle is changed, due to infection risk.
Storage requirements specify that tirzepatide pens should be refrigerated at 2–8°C and protected from light. Unopened pens may be kept at room temperature (up to 30°C) for up to 21 days. Each pen is for single use only and must be discarded after injection. Never freeze tirzepatide; frozen medication must be discarded. Patients should receive comprehensive training from their diabetes specialist nurse or practice nurse before first use, with written instructions provided for home reference.
Gastrointestinal adverse effects are the most commonly reported side effects with tirzepatide, particularly during dose initiation and escalation. Nausea, vomiting, diarrhoea, constipation, and abdominal discomfort affect a significant proportion of patients, though symptoms typically diminish over several weeks as tolerance develops. The gradual dose titration schedule is specifically designed to minimise these effects.
Timing strategies to reduce side effects include:
Injecting tirzepatide in the evening may allow patients to sleep through periods when symptoms are most noticeable, which often occur around injection days, especially during dose escalation.
Eating smaller, more frequent meals rather than large portions can reduce gastrointestinal distress.
Avoiding high-fat, spicy, or heavily processed foods immediately after injection may improve tolerability.
Maintaining adequate hydration is essential, particularly if experiencing vomiting or diarrhoea.
Important safety considerations include:
Gallbladder disease: Tirzepatide may increase the risk of gallbladder problems including gallstones and inflammation. Seek urgent medical attention for severe right upper abdominal pain, fever, or jaundice.
Medication interactions: Tirzepatide slows gastric emptying, which can affect the absorption of oral medications. Users of oral hormonal contraceptives should use additional non-oral or barrier contraception for 4 weeks after starting tirzepatide and after each dose increase.
Pregnancy and breastfeeding: Tirzepatide should be avoided during pregnancy and breastfeeding. Women of childbearing potential should use effective contraception and discuss with their doctor if planning pregnancy.
Thyroid concerns: Patients should be vigilant for symptoms such as a lump in the neck, persistent hoarseness, or difficulty swallowing, and report these promptly for evaluation.
Hypoglycaemia risk increases when tirzepatide is combined with insulin or sulfonylureas; dose adjustments of these medications may be necessary. Patients should be educated on recognising and managing low blood glucose and exercise caution when driving or operating machinery if taking these combinations.
When to contact your GP: Persistent vomiting preventing fluid intake, severe abdominal pain, signs of dehydration, or any concerning symptoms warrant prompt medical review. Regular follow-up appointments are essential to monitor glycaemic control, weight changes, and tolerability, with dose adjustments made according to individual response and treatment targets.
Patients are encouraged to report any suspected side effects to the MHRA Yellow Card Scheme at yellowcard.mhra.gov.uk or via the Yellow Card app.
Yes, you can change your injection day if necessary, provided there are at least 3 days (72 hours) between doses. Consistency on the new chosen day is then important for maintaining steady therapeutic levels.
Tirzepatide can be injected with or without meals, as food does not affect its absorption. Some patients prefer injecting before a lighter meal if experiencing gastrointestinal symptoms.
If you miss a dose, administer it as soon as possible within 4 days (96 hours). If more than 4 days have passed, skip the missed dose and inject your next dose on the regularly scheduled day.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.