
Is headache a side effect of GLP-1 medications? Yes, headache is a recognised adverse effect of GLP-1 receptor agonists, though it occurs less frequently than gastrointestinal symptoms. These medications, including semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), and dulaglutide (Trulicity), are increasingly prescribed in the UK for type 2 diabetes and weight management. Clinical trial data submitted to the MHRA and EMA document headache as common (affecting 1 in 10 to 1 in 100 people) with diabetes formulations, and very common (more than 1 in 10) with higher weight-management doses. Understanding this side effect, its potential causes, and management strategies helps patients and healthcare professionals optimise treatment whilst maintaining safety and adherence.
Quick Answer: Headache is a recognised side effect of GLP-1 receptor agonists, classified as common (1 in 10 to 1 in 100 people) for diabetes formulations and very common (more than 1 in 10) for weight-management doses.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists represent a class of medications increasingly prescribed in the UK for managing type 2 diabetes mellitus and, more recently, for weight management in specific patient populations. These medicines work by mimicking the action of naturally occurring GLP-1, a hormone produced in the intestines that plays a crucial role in glucose regulation and appetite control.
Commonly prescribed GLP-1 medications authorised in the UK include semaglutide (Ozempic for diabetes; Wegovy for weight management), dulaglutide (Trulicity for diabetes), liraglutide (Victoza for diabetes; Saxenda for weight management), and exenatide (Byetta, Bydureon for diabetes), though local availability may vary. The Medicines and Healthcare products Regulatory Agency (MHRA) has approved these medications following rigorous clinical trials demonstrating their efficacy in glycaemic control, with some agents (liraglutide, dulaglutide, and semaglutide) also showing cardiovascular benefits in specific populations.
Like all medications, GLP-1 receptor agonists can cause side effects, though not everyone experiences them. The most frequently reported adverse effects are gastrointestinal in nature, including nausea, vomiting, diarrhoea, constipation, and abdominal discomfort. These symptoms typically occur during treatment initiation or dose escalation and often diminish over time as the body adjusts to the medication.
Other commonly documented side effects include injection site reactions (redness, itching, or swelling), fatigue, and dizziness. Less common but more serious adverse effects require careful monitoring, including pancreatitis, gallbladder disease, and potential worsening of diabetic retinopathy (particularly with semaglutide when rapid HbA1c reduction occurs). Dehydration from gastrointestinal side effects may increase the risk of acute kidney injury. Understanding the full spectrum of potential side effects enables patients and healthcare professionals to make informed decisions about treatment and recognise when symptoms warrant medical attention.
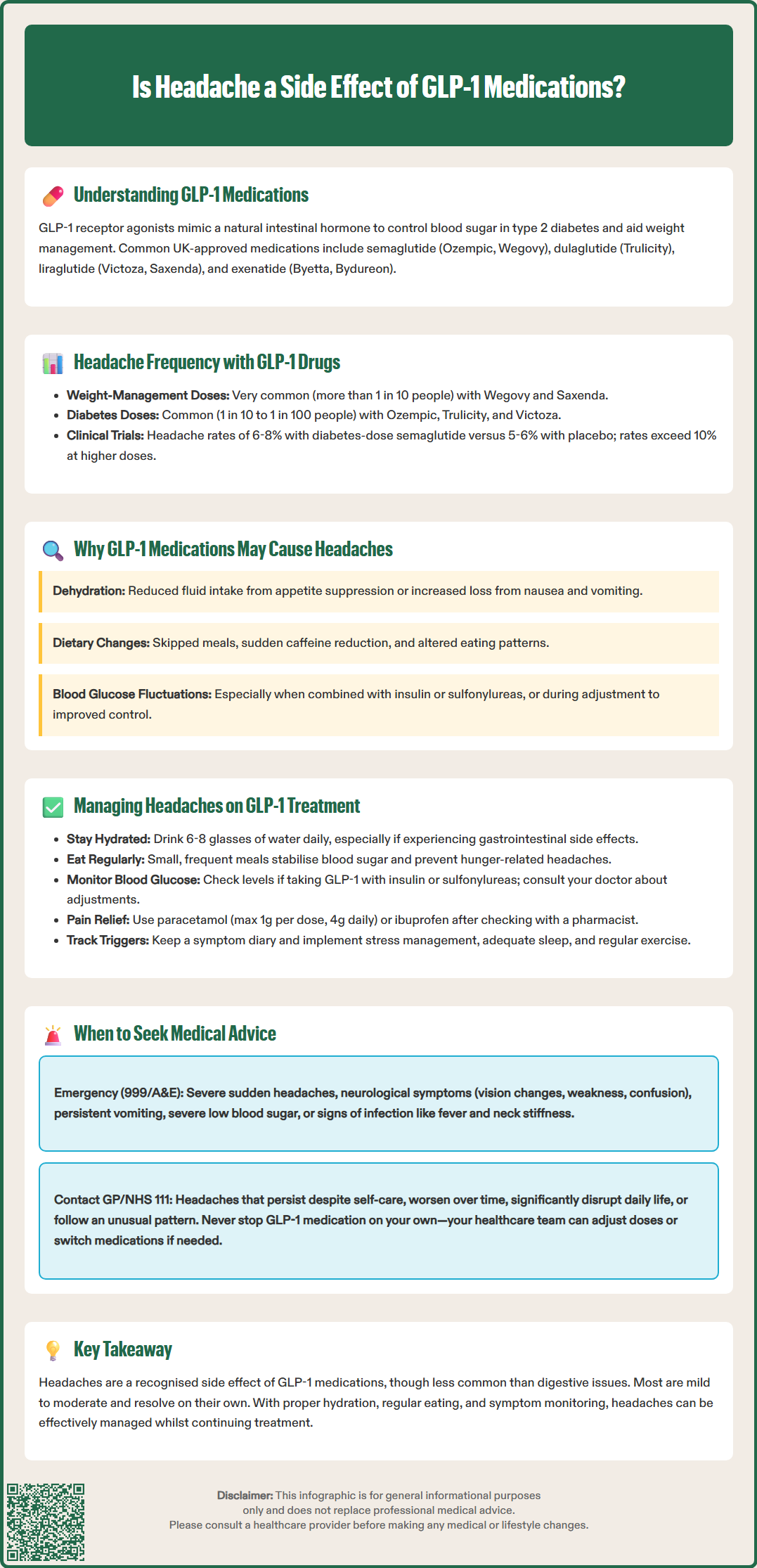
Yes, headache is recognised as a potential side effect of GLP-1 receptor agonists, though it occurs less frequently than gastrointestinal symptoms. Clinical trial data submitted to regulatory authorities, including the MHRA and European Medicines Agency (EMA), document headache as an adverse event across different GLP-1 medications, with varying frequencies depending on the specific drug and dosage.
According to the Summary of Product Characteristics (SmPC) for these medications, headache is classified as very common (affecting more than 1 in 10 people) with weight-management doses of GLP-1 receptor agonists such as Wegovy (semaglutide 2.4 mg) and Saxenda (liraglutide 3 mg). For diabetes-indicated GLP-1 medications including Ozempic, Trulicity, Victoza, Byetta, Bydureon, and Rybelsus, headache is typically classified as common (affecting between 1 in 10 and 1 in 100 people).
For instance, in pivotal trials of semaglutide for diabetes, headache was reported by approximately 6-8% of participants receiving the medication compared to 5-6% in placebo groups, suggesting a modest but measurable association. At the higher doses used for weight management, headache rates can exceed 10%.
It is important to note that headaches can occur for numerous reasons unrelated to medication, including stress, dehydration, dietary changes, caffeine withdrawal, or pre-existing conditions such as migraine or tension-type headache. Patients commencing GLP-1 therapy often simultaneously make significant lifestyle modifications—including dietary changes and increased physical activity—which may independently contribute to headache symptoms.
Most reported headaches are mild to moderate in intensity and resolve spontaneously without requiring treatment discontinuation. However, persistent or severe headaches should be medically assessed. Healthcare professionals should evaluate each case individually, considering the temporal relationship between medication initiation and symptom onset, as well as alternative explanations for headache.
The precise mechanisms by which GLP-1 receptor agonists may trigger headaches are not fully elucidated, but several plausible physiological explanations exist. Understanding these potential pathways helps contextualise the symptom and guides appropriate management strategies.
Dehydration is a well-established cause of headache and may occur with GLP-1 medications due to reduced fluid intake (from appetite suppression) or increased fluid loss (from gastrointestinal side effects such as nausea, vomiting, or diarrhoea). The NHS recommends maintaining adequate hydration (6-8 glasses of fluid daily) while taking these medications.
Changes in eating patterns and caloric intake frequently accompany GLP-1 therapy, as these medications significantly reduce appetite and promote satiety. Patients may inadvertently skip meals, reduce fluid intake, or dramatically alter their dietary composition. Irregular eating schedules and sudden reductions in caffeine consumption (often found in high-calorie beverages) are well-established headache triggers that may coincide with GLP-1 treatment.
Whilst GLP-1 receptor agonists themselves have a low risk of causing hypoglycaemia, blood glucose fluctuations may occur, particularly when these medications are combined with insulin or sulfonylureas. Some patients may experience headache as their body adapts to improved glycaemic control, especially if they were previously accustomed to higher blood glucose levels.
Gastrointestinal side effects may indirectly contribute to headache through dehydration and electrolyte disturbances. Additionally, some research suggests that GLP-1 receptors are present in the central nervous system, though the clinical significance of this in relation to headache remains unclear.
Finally, individual susceptibility factors such as pre-existing migraine disorders, stress related to managing a chronic condition, or anxiety about new medication may amplify the likelihood of experiencing headaches during GLP-1 therapy. The multifactorial nature of headache makes it challenging to attribute causation solely to the medication itself.
For patients experiencing headaches whilst taking GLP-1 medications, several practical management strategies can help alleviate symptoms without necessarily requiring treatment discontinuation. These approaches should be discussed with a healthcare professional to ensure they are appropriate for individual circumstances.
Maintaining adequate hydration is paramount. Patients should aim to drink sufficient water throughout the day, particularly if experiencing gastrointestinal side effects that may increase fluid loss. The NHS recommends approximately 6-8 glasses of fluid daily, adjusted for individual needs, activity levels, and climate.
Establishing regular eating patterns helps stabilise blood glucose levels and prevents hunger-related headaches. Even if appetite is reduced, consuming small, frequent meals or snacks ensures consistent nutrient and energy intake. Patients should avoid prolonged fasting periods and maintain a balanced diet rich in complex carbohydrates, lean proteins, and healthy fats.
Blood glucose monitoring may be advisable for patients taking GLP-1 medications alongside insulin or sulfonylureas, as these combinations increase hypoglycaemia risk. For those on GLP-1 therapy alone, routine self-monitoring is not generally recommended by NICE unless there are specific clinical indications. If headaches coincide with lower glucose readings, discussing adjustment of diabetes medications with a healthcare provider may be necessary. Patients should never alter prescribed doses without medical guidance.
Over-the-counter analgesics such as paracetamol or ibuprofen can provide symptomatic relief for mild to moderate headaches. These should be used according to package instructions and with awareness of any contraindications. Do not exceed 1 gram of paracetamol per dose or 4 grams per day. Patients should use caution with non-steroidal anti-inflammatory drugs (NSAIDs) if they have renal impairment, are dehydrated, have a history of peptic ulcer disease, or are taking anticoagulants. A pharmacist can provide personalised advice on appropriate analgesic choices.
Lifestyle modifications including stress management techniques, adequate sleep (7-9 hours nightly), regular physical activity, and limiting alcohol consumption may reduce headache frequency and severity. Keeping a symptom diary can help identify specific triggers and patterns, facilitating more targeted interventions and informing discussions with healthcare professionals about treatment optimisation.
Whilst mild headaches during GLP-1 therapy often resolve spontaneously or respond to simple measures, certain circumstances warrant prompt medical evaluation. Patients should be educated about warning signs that require professional assessment to ensure safety and appropriate management.
Call 999 or go to A&E immediately if headache is accompanied by:
Severe, sudden-onset headache (often described as "thunderclap" or the worst headache ever experienced)
Neurological symptoms such as visual disturbances, weakness, numbness, difficulty speaking, or confusion
Persistent vomiting that prevents adequate fluid or medication intake
Signs of severe hypoglycaemia including sweating, tremor, palpitations, or altered consciousness
Fever, neck stiffness, or photophobia, which may indicate serious infection
If you suspect pancreatitis (severe, persistent abdominal pain, often radiating to the back, with or without vomiting), stop taking your GLP-1 medication and seek urgent medical attention.
Contact your GP, diabetes specialist nurse, or NHS 111 if:
Headaches are persistent, worsening, or significantly impacting daily activities despite simple management measures
You experience frequent hypoglycaemic episodes (blood glucose below 4 mmol/L)
You have signs of dehydration such as reduced urine output, excessive thirst, or dizziness when standing
Side effects are affecting medication adherence or quality of life
You develop new or unusual symptoms that concern you
Headaches follow a different pattern from any pre-existing headache disorder
Healthcare professionals can assess whether headaches are likely related to GLP-1 therapy or require investigation for alternative causes. They may recommend dose adjustment, temporary treatment interruption, or switching to a different GLP-1 medication. Never discontinue prescribed medication without medical guidance, as abrupt cessation may adversely affect glycaemic control. NICE guidance emphasises individualised treatment approaches, and your healthcare team can work with you to optimise therapy whilst minimising troublesome side effects.
If you suspect an adverse reaction to your medication, you can report it through the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk, which helps monitor medication safety.
Headaches are common with diabetes formulations (affecting 1 in 10 to 1 in 100 people) and very common with weight-management doses like Wegovy (affecting more than 1 in 10 people). Clinical trials show headache rates of approximately 6-8% with diabetes doses and over 10% with higher weight-management doses.
Headaches may result from dehydration due to reduced fluid intake or gastrointestinal side effects, changes in eating patterns including meal skipping or caffeine withdrawal, blood glucose fluctuations, or individual susceptibility factors. The precise mechanisms are not fully understood.
Seek immediate medical attention (call 999) for severe sudden-onset headache, neurological symptoms, persistent vomiting, or signs of pancreatitis. Contact your GP or NHS 111 if headaches are persistent, worsening, significantly impacting daily activities, or not responding to simple management measures.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.