Rybelsus (semaglutide) is an oral GLP-1 receptor agonist licensed in the UK for type 2 diabetes management. For patients seeking medication similar to Rybelsus, several alternatives exist, including injectable GLP-1 agonists such as liraglutide, dulaglutide, and injectable semaglutide, as well as other diabetes medication classes like SGLT2 inhibitors and DPP-4 inhibitors. Each option differs in formulation, dosing frequency, efficacy, and side-effect profile. Understanding these alternatives helps clinicians and patients make informed, personalised treatment decisions aligned with NICE guidance, cardiovascular risk, renal function, and individual preferences. This article explores comparable medications, their mechanisms, and factors influencing treatment selection within NHS prescribing frameworks.
Quick Answer: Medications similar to Rybelsus include injectable GLP-1 receptor agonists (liraglutide, dulaglutide, injectable semaglutide, exenatide, lixisenatide) and alternative diabetes drug classes such as SGLT2 inhibitors and DPP-4 inhibitors.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereRybelsus (semaglutide) is an oral medication licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of medicines called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone that helps regulate blood glucose levels.
The mechanism of action involves several complementary pathways. Rybelsus stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning it only promotes insulin release when blood glucose levels are elevated. This reduces the risk of hypoglycaemia compared to some other diabetes medications. Simultaneously, it suppresses the release of glucagon, a hormone that raises blood glucose, particularly after meals. Additionally, GLP-1 receptor agonists slow gastric emptying, which moderates the rate at which glucose enters the bloodstream following food intake.
What distinguishes Rybelsus from other GLP-1 medications is its oral formulation. It was the first GLP-1 receptor agonist available as a tablet, receiving marketing authorisation in the UK in 2020. The active ingredient, semaglutide, is combined with an absorption enhancer (salcaprozate sodium, or SNAC) that facilitates uptake through the stomach lining. This innovation addresses a significant limitation of earlier GLP-1 therapies, which required subcutaneous injection.
Patients typically start on a low dose (3 mg once daily) for the first month, which may be increased to 7 mg or 14 mg depending on glycaemic control and tolerability. The tablet must be taken with no more than 120 ml of water, on an empty stomach, at least 30 minutes before any food, drink, or other oral medicines, and swallowed whole. If a dose is missed, the missed tablet should be skipped and the next dose taken the following day.
Common adverse effects include nausea, vomiting, diarrhoea, constipation, abdominal pain and decreased appetite, particularly during dose escalation. The risk of hypoglycaemia increases when Rybelsus is used with sulfonylureas or insulin; dose reductions of these medications may be needed. Patients with diabetic retinopathy should be monitored closely, as rapid improvements in glucose control may temporarily worsen retinopathy. Rybelsus should not be used during pregnancy or breastfeeding, and women of childbearing potential should use effective contraception.
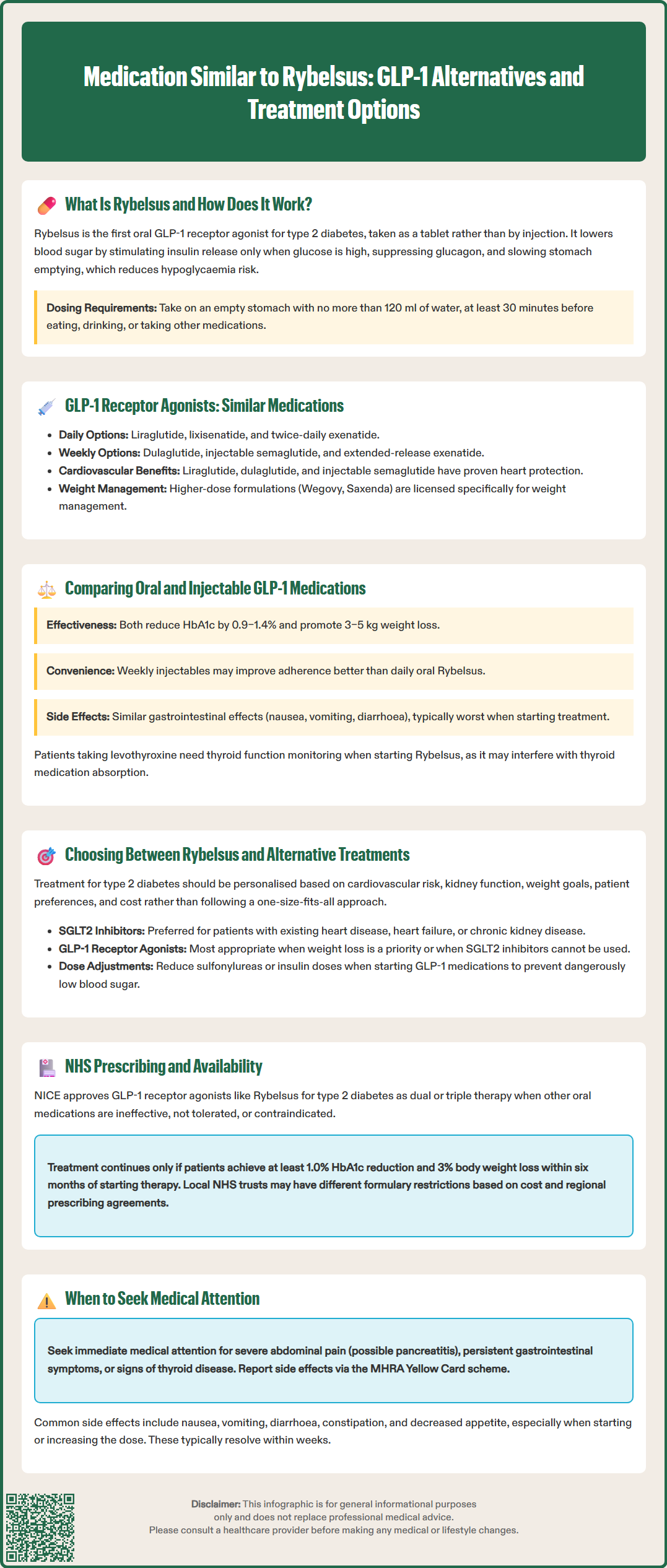
Several other GLP-1 receptor agonists are available in the UK, each with distinct characteristics regarding formulation, dosing frequency, and licensed indications. Understanding these alternatives helps clinicians and patients make informed treatment decisions.
Injectable GLP-1 receptor agonists include:
Liraglutide (Victoza): Administered once daily via subcutaneous injection. It has been available since 2009 and has an established safety profile. A higher-dose formulation (Saxenda) is licensed specifically for weight management, not for glycaemic control in diabetes.
Dulaglutide (Trulicity): A once-weekly injection that offers convenience for patients who prefer less frequent dosing. It comes in a pre-filled pen device designed for ease of use.
Exenatide: Available in both short-acting (twice-daily, Byetta) and extended-release (once-weekly, Bydureon) formulations. Exenatide was among the first GLP-1 agonists introduced to clinical practice.
Semaglutide injection (Ozempic): The injectable form of the same active ingredient found in Rybelsus, administered once weekly. A higher-dose version (Wegovy) is licensed for weight management in specific patient groups, not for treating hyperglycaemia in diabetes.
Lixisenatide (Lyxumia): A once-daily injectable GLP-1 receptor agonist also available in the UK.
All GLP-1 receptor agonists share a common mechanism of action but differ in their pharmacokinetic properties, which influence dosing schedules and side-effect profiles. Longer-acting formulations generally provide more stable drug levels and may offer improved glycaemic control with potentially better adherence due to reduced dosing frequency, though individual responses vary.
These medications are typically considered when metformin alone provides inadequate glycaemic control, or as part of combination therapy. NICE guidance supports their use particularly in specific patient groups according to NG28 criteria. Importantly, cardiovascular outcome trials have shown differences between agents: liraglutide (LEADER trial), dulaglutide (REWIND trial), and injectable semaglutide (SUSTAIN-6 trial) have demonstrated cardiovascular benefits, while exenatide (EXSCEL) and lixisenatide (ELIXA) showed cardiovascular safety but not superiority.
The choice between oral Rybelsus and injectable GLP-1 receptor agonists involves weighing several clinical and practical considerations. Both formulations offer effective glycaemic control, but patient preferences, lifestyle factors, and individual response patterns play important roles in treatment selection.
Efficacy considerations: Clinical trial data suggest that injectable semaglutide (Ozempic) may provide slightly greater HbA1c reductions compared to oral Rybelsus at equivalent doses, though both formulations demonstrate clinically meaningful improvements. The PIONEER trial programme, which evaluated oral semaglutide, showed HbA1c reductions of 0.9–1.4% (10–15 mmol/mol) depending on dose. Weight loss effects are observed with both formulations, typically ranging from 3–5 kg, though individual responses vary considerably.
Administration and adherence: The oral route eliminates injection-related barriers, which may be particularly relevant for patients with needle phobia or those who find injections inconvenient. However, Rybelsus requires strict administration guidelines—taken with no more than 120 ml of water, on an empty stomach, at least 30 minutes before any food, drink, or other oral medicines, and swallowed whole. This regimen may prove challenging for some patients. Injectable formulations, particularly once-weekly options like dulaglutide or injectable semaglutide, may offer better adherence through reduced dosing frequency.
Side-effect profiles: Gastrointestinal adverse effects (nausea, vomiting, diarrhoea) are common across all GLP-1 medications, typically most pronounced during initiation and dose escalation. These effects are generally transient, resolving within several weeks. Data from the PIONEER and SUSTAIN programmes suggest broadly similar tolerability profiles between oral and injectable formulations, though individual patient experiences vary.
Practical considerations include cost-effectiveness, which influences NHS formulary decisions, and patient preference, which significantly impacts long-term adherence and treatment success. Patients taking levothyroxine should be monitored for changes in thyroid function when starting Rybelsus, as it may affect absorption.
Treatment selection for type 2 diabetes should follow a personalised approach, considering multiple factors including glycaemic control targets, cardiovascular risk profile, renal function, body weight, patient preferences, and cost-effectiveness.
NICE guidance (NG28) recommends a stepwise approach to diabetes management. After lifestyle modification and metformin, treatment intensification depends on individual circumstances:
Cardiovascular disease, heart failure or chronic kidney disease: SGLT2 inhibitors are generally preferred first-line options for these patients. GLP-1 receptor agonists with proven cardiovascular benefit (such as liraglutide, dulaglutide, or injectable semaglutide) may be considered when SGLT2 inhibitors are not appropriate or as add-on therapy.
Chronic kidney disease: SGLT2 inhibitors have demonstrated renoprotective effects and are generally preferred, though GLP-1 agonists remain appropriate alternatives in certain circumstances.
Body weight concerns: When weight loss is a treatment priority, GLP-1 receptor agonists (including Rybelsus) offer advantages over medications associated with weight gain, such as sulphonylureas or insulin.
Alternative medication classes that may be considered instead of or alongside GLP-1 agonists include:
SGLT2 inhibitors (dapagliflozin, empagliflozin, canagliflozin): These offer cardiovascular and renal benefits with a different mechanism of action, promoting glucose excretion through urine.
DPP-4 inhibitors (sitagliptin, linagliptin): These enhance incretin activity through a different pathway, are generally well-tolerated, but provide more modest glycaemic improvements.
Insulin therapy: Reserved for patients requiring more intensive glycaemic control or those with significant beta-cell dysfunction.
When initiating GLP-1 receptor agonists in patients already taking sulfonylureas or insulin, consider reducing the doses of these medications to mitigate hypoglycaemia risk. HbA1c should be rechecked approximately 3 months after treatment changes, with regular monitoring of renal function and weight.
Patients should be counselled about realistic expectations, potential adverse effects, and the importance of continued lifestyle modification. Shared decision-making is essential, incorporating patient values and preferences into the treatment plan.
Access to GLP-1 receptor agonists, including Rybelsus, within the NHS is governed by NICE technology appraisals and local formulary decisions, which consider clinical effectiveness and cost-effectiveness.
NICE recommendations support GLP-1 receptor agonist use in specific circumstances:
As dual therapy with metformin when triple therapy with metformin and two other oral drugs is not effective, not tolerated or contraindicated, and when a GLP-1 receptor agonist is appropriate.
As triple therapy in combination with metformin and another oral agent when glycaemic control remains inadequate.
Treatment should be continued only if there is a beneficial metabolic response, defined as a reduction of at least 11 mmol/mol (1.0%) in HbA1c and weight loss of at least 3% of initial body weight at six months.
Rybelsus received NICE approval (TA775) in 2022 as an option for treating type 2 diabetes within these parameters. However, local formulary restrictions may vary, with some NHS trusts preferring specific GLP-1 agents based on cost considerations or local prescribing agreements.
Prescribing is typically managed according to local formulary and shared care protocols, which may vary across different NHS regions. Patients require appropriate counselling about administration technique (particularly for Rybelsus), recognition of adverse effects, and when to seek medical advice.
Supply considerations: Recent years have seen intermittent supply challenges for some GLP-1 medications due to increased global demand, particularly following publicity around weight-loss effects. The Department of Health and Social Care and NHS England have issued guidance prioritising supply for licensed diabetes indications.
Patients experiencing persistent gastrointestinal symptoms, signs of pancreatitis (severe abdominal pain), or symptoms of thyroid disease should contact their GP promptly. Patients should be advised to report any suspected side effects to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
Injectable GLP-1 receptor agonists similar to Rybelsus include liraglutide (once daily), dulaglutide (once weekly), injectable semaglutide (once weekly), exenatide (twice daily or once weekly), and lixisenatide (once daily). All share the same mechanism of action but differ in dosing frequency and pharmacokinetic profiles.
SGLT2 inhibitors (dapagliflozin, empagliflozin, canagliflozin) are alternative diabetes medications with a different mechanism, promoting glucose excretion through urine. They are particularly preferred for patients with cardiovascular disease, heart failure, or chronic kidney disease due to proven cardio-renal protective effects.
Choice depends on patient preference, lifestyle factors, and clinical considerations. Oral Rybelsus eliminates injection-related barriers but requires strict administration guidelines, whilst once-weekly injectables may offer better adherence through reduced dosing frequency. Both formulations provide effective glycaemic control with similar side-effect profiles.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.