Mounjaro (tirzepatide) is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes, whilst Zepbound (also tirzepatide) is approved for weight management. Patients with Graves' disease, an autoimmune thyroid condition causing hyperthyroidism, may wonder whether they can safely use tirzepatide. Whilst there is no absolute contraindication to combining Mounjaro and Graves' disease, individualised assessment is essential. This article explores the considerations, potential interactions, and monitoring requirements for patients with thyroid conditions who are prescribed tirzepatide, helping you make informed decisions in consultation with your healthcare team.
Quick Answer: There is no official contraindication to using Mounjaro (tirzepatide) in patients with Graves' disease, but individualised assessment and stable thyroid function are essential before initiation.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus. For weight management in adults with obesity or overweight with weight-related comorbidities, tirzepatide is licensed under the brand name Zepbound. Both are administered as once-weekly subcutaneous injections and belong to a novel class of medications known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists.
The mechanism of action involves mimicking two naturally occurring incretin hormones that play crucial roles in glucose regulation and appetite control. By activating both GIP and GLP-1 receptors, tirzepatide enhances insulin secretion in a glucose-dependent manner, suppresses inappropriate glucagon release, slows gastric emptying, and reduces appetite. This dual action results in improved glycaemic control and significant weight loss in clinical trials.
Tirzepatide is typically initiated at a low dose (2.5 mg weekly) and gradually titrated upwards every four weeks to minimise gastrointestinal side effects. The maintenance dose ranges from 5 mg to 15 mg weekly, depending on individual response and tolerability. Common adverse effects include nausea, vomiting, diarrhoea, constipation, and abdominal discomfort, which tend to be most pronounced during dose escalation.
Important safety considerations include the risk of acute pancreatitis (stop treatment if suspected), gallbladder disease, acute kidney injury from dehydration, and potential worsening of diabetic retinopathy in patients with pre-existing disease. Tirzepatide is not indicated for type 1 diabetes or diabetic ketoacidosis.
The Medicines and Healthcare products Regulatory Agency (MHRA) has approved tirzepatide for use in the UK, and NICE guidance supports its use in specific patient populations. For weight management, NICE recommends Zepbound for adults with a BMI of at least 35 kg/m² (or ≥30 kg/m² with weight-related comorbidities) who have at least one weight-related comorbidity and have completed a tier 3 weight management programme.
Patients should report any suspected side effects via the MHRA Yellow Card Scheme.
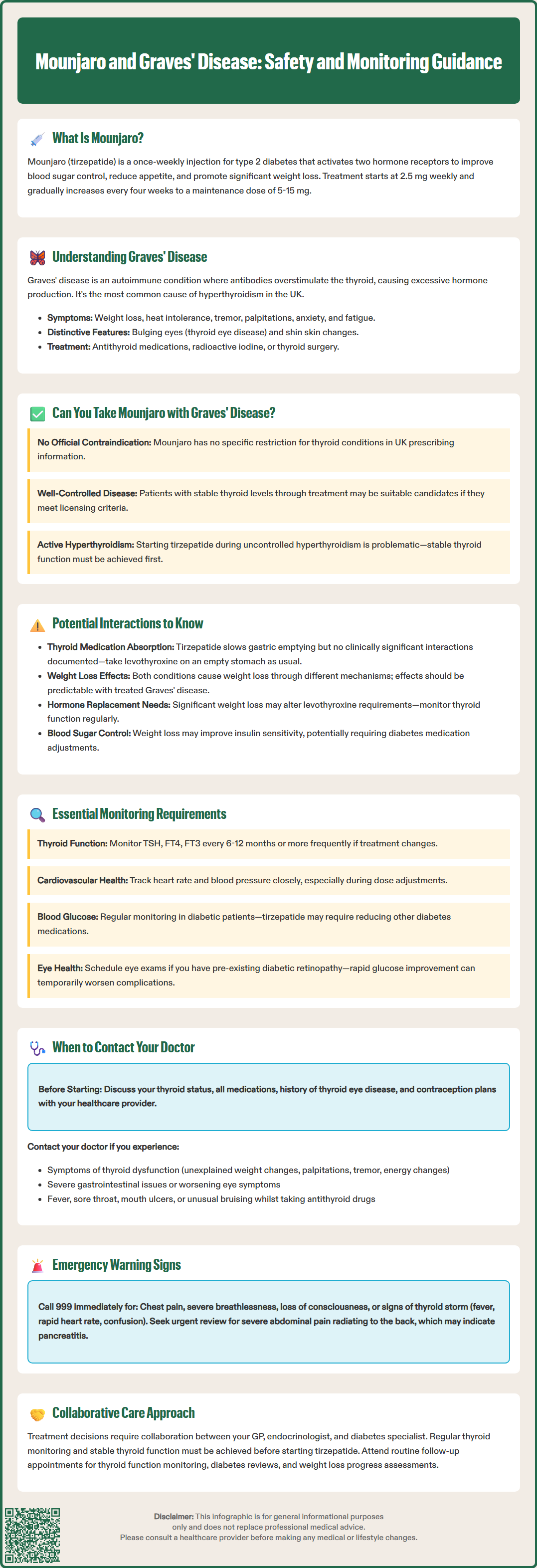
Graves' disease is an autoimmune condition and the most common cause of hyperthyroidism (overactive thyroid) in the UK, affecting approximately 2–3% of women and 0.5% of men during their lifetime, according to the British Thyroid Foundation. In this condition, the immune system produces antibodies—specifically thyroid-stimulating immunoglobulins (TSI)—that bind to and activate the thyroid-stimulating hormone (TSH) receptor on thyroid cells, causing excessive production and release of thyroid hormones (thyroxine and triiodothyronine).
The clinical features of Graves' disease reflect the effects of excess thyroid hormone on multiple organ systems. Patients commonly experience weight loss despite increased appetite, heat intolerance, tremor, palpitations, anxiety, fatigue, and muscle weakness. Distinctive features include thyroid eye disease (Graves' orbitopathy), which can cause bulging eyes, double vision, and eye discomfort, and occasionally pretibial myxoedema (skin changes on the shins).
Diagnosis is typically confirmed through blood tests showing suppressed TSH levels with elevated free thyroxine (FT4) and/or free triiodothyronine (FT3), alongside positive TSH receptor antibodies (TRAb). NICE guidance (NG145) recommends that all patients with suspected hyperthyroidism should have thyroid function tests. TRAb testing is recommended to determine the cause of hyperthyroidism, with thyroid ultrasound or scintigraphy considered when the diagnosis remains unclear.
Treatment options for Graves' disease include antithyroid medications (such as carbimazole or propylthiouracil), radioactive iodine therapy, or thyroid surgery. Many patients require long-term management, and some may eventually develop hypothyroidism (underactive thyroid) following treatment. Regular monitoring of thyroid function is essential throughout the disease course to ensure optimal hormone levels and adjust treatment accordingly.
There is no official contraindication to using Mounjaro or Zepbound in patients with Graves' disease or other thyroid conditions according to the UK Summary of Product Characteristics (SmPC). The prescribing information for tirzepatide does not list thyroid disorders as absolute contraindications. However, this does not mean the combination is without considerations, and individualised assessment is essential.
Patients with well-controlled Graves' disease—those whose thyroid function has been stabilised with antithyroid medication, radioactive iodine, or surgery—may be suitable candidates for tirzepatide if they meet the licensing criteria for type 2 diabetes or weight management. The key consideration is ensuring that thyroid hormone levels are within the target range and that the patient is under appropriate endocrine follow-up.
For individuals with active, uncontrolled hyperthyroidism, initiating tirzepatide may be less straightforward. Hyperthyroidism itself causes increased metabolic rate and weight loss, which could complicate the assessment of tirzepatide's effects and tolerability. NICE guidance (NG145) emphasises the importance of achieving stable thyroid function before initiating other treatments. Additionally, the gastrointestinal side effects of tirzepatide might be more poorly tolerated in patients already experiencing symptoms from thyroid dysfunction.
Clinical judgement is paramount. Healthcare professionals should consider the patient's overall clinical picture, including:
Current thyroid status and stability of thyroid function
Concurrent medications and potential interactions
Presence of other autoimmune conditions
Individual treatment goals and priorities
A collaborative approach involving the patient's GP, endocrinologist, and diabetes specialist (where applicable) ensures comprehensive care. Patients should be counselled about the importance of maintaining regular thyroid monitoring and reporting any new or worsening symptoms promptly.
While direct pharmacological interactions between tirzepatide and thyroid hormones or antithyroid medications are not well-documented, several indirect considerations warrant attention. Understanding these potential interactions helps clinicians and patients make informed decisions about concurrent use.
Gastric emptying and medication absorption represent one theoretical concern. Tirzepatide slows gastric emptying as part of its mechanism of action, which could potentially affect the absorption of oral medications, including levothyroxine (used to treat hypothyroidism) or antithyroid drugs like carbimazole. Although there is no robust clinical evidence suggesting clinically significant interactions with thyroid medications specifically, the UK SmPC for tirzepatide notes an important interaction with oral contraceptives. Women using oral contraceptives should use additional non-oral/barrier contraception for 4 weeks after initiation and following each dose escalation due to reduced contraceptive efficacy. For levothyroxine, patients should continue to take it on an empty stomach, at least 30 minutes before food or other medications, which should minimise any potential impact.
Metabolic effects also merit consideration. Both hyperthyroidism and tirzepatide can influence appetite, weight, and metabolic rate, though in different ways. Hyperthyroidism typically increases metabolic rate and causes weight loss, whilst tirzepatide promotes weight loss through appetite suppression and improved glucose metabolism. In patients with treated Graves' disease who have achieved euthyroidism (normal thyroid function), the weight loss effects of tirzepatide should be more predictable.
Thyroid function monitoring remains essential. Some case reports in the literature have suggested that significant weight loss from any cause can occasionally affect thyroid hormone requirements in patients on thyroid replacement therapy. Conversely, weight loss might improve insulin sensitivity and glycaemic control, potentially requiring adjustments to diabetes medications.
There is no evidence that tirzepatide directly affects thyroid hormone production, thyroid antibody levels, or the autoimmune process underlying Graves' disease. However, the absence of evidence is not evidence of absence, and post-marketing surveillance continues to monitor for unexpected effects.
Patients with Graves' disease who are prescribed tirzepatide require comprehensive monitoring to ensure both conditions are optimally managed and to detect any potential complications early. A structured approach to monitoring enhances patient safety and treatment outcomes.
Thyroid function tests should be performed regularly according to the patient's clinical status. For those with stable, treated Graves' disease, thyroid function (TSH, FT4, and FT3) is typically monitored every 6–12 months, or more frequently if treatment has recently been adjusted. Patients initiating tirzepatide should maintain their usual thyroid monitoring schedule and report any symptoms suggestive of thyroid dysfunction, such as:
Unexplained weight changes beyond those expected from tirzepatide
New or worsening palpitations, tremor, or anxiety
Changes in energy levels or temperature tolerance
Alterations in bowel habit (beyond expected gastrointestinal effects of tirzepatide)
Cardiovascular monitoring is particularly important, as both hyperthyroidism and GLP-1 receptor agonists can affect heart rate. Patients should be advised to report palpitations, chest pain, or breathlessness. Blood pressure should be monitored regularly, especially during tirzepatide dose titration.
Gastrointestinal symptoms require careful assessment. Whilst nausea, vomiting, and diarrhoea are common with tirzepatide, severe or persistent symptoms warrant medical review to exclude other causes and ensure adequate hydration and nutrition. Severe, persistent abdominal pain (especially if radiating to the back) with or without vomiting may indicate acute pancreatitis, which requires immediate medical attention and discontinuation of tirzepatide. Patients should be counselled on managing these side effects, including eating smaller meals and avoiding high-fat foods.
Additional safety monitoring should include:
Signs of gallbladder disease (right upper quadrant pain, jaundice)
Symptoms of dehydration and potential acute kidney injury, especially during gastrointestinal side effects
For patients with diabetes and pre-existing retinopathy, eye examinations as rapid improvement in glucose control may temporarily worsen diabetic retinopathy
Blood glucose monitoring is essential for patients with diabetes. Tirzepatide can significantly lower blood glucose, and concurrent medications (particularly insulin or sulphonylureas) may require dose reduction to prevent hypoglycaemia. Patients should be educated on recognising and managing low blood sugar.
Weight and body composition should be tracked regularly to assess treatment response and ensure weight loss is occurring at a safe, sustainable rate. Rapid or excessive weight loss may necessitate review of both tirzepatide and thyroid medication dosing.
Patients with Graves' disease considering or taking tirzepatide should maintain open communication with their healthcare team and seek medical advice in specific circumstances. Knowing when to contact your GP or endocrinologist ensures timely intervention and optimal management of both conditions.
Before starting tirzepatide, patients should discuss their thyroid condition with the prescribing clinician. This conversation should cover:
Current thyroid status and recent thyroid function test results
All medications, including antithyroid drugs, beta-blockers, or thyroid hormone replacement
History of thyroid eye disease or other complications of Graves' disease
Any other autoimmune conditions or relevant medical history
Contraception plans if of childbearing potential (tirzepatide is not recommended during pregnancy and requires effective contraception during treatment)
During treatment, contact your healthcare provider if you experience:
Symptoms of thyroid dysfunction: unexplained weight changes, persistent palpitations, new tremor, significant changes in energy levels, or worsening anxiety
Severe gastrointestinal symptoms: persistent vomiting, severe abdominal pain (especially if radiating to the back), or signs of dehydration (dark urine, dizziness, reduced urination)
Hypoglycaemia symptoms (for patients with diabetes): shakiness, sweating, confusion, or difficulty concentrating
Cardiovascular concerns: chest pain, irregular heartbeat, or breathlessness
Eye symptoms: if you have thyroid eye disease, report any worsening of eye symptoms, vision changes, or increased eye discomfort
If taking carbimazole or propylthiouracil, seek urgent medical review if you develop fever, sore throat, mouth ulcers, or unusual bruising, as these may indicate agranulocytosis, a rare but serious side effect requiring immediate blood tests.
Routine follow-up appointments should be attended as scheduled. These typically include thyroid function monitoring every 6–12 months for stable patients, more frequent diabetes reviews if applicable, and regular assessment of weight loss progress and medication tolerability.
Emergency medical attention is required for severe symptoms: call 999 or attend A&E for chest pain, severe breathlessness, loss of consciousness, or signs of thyroid storm (a rare but life-threatening complication of severe hyperthyroidism characterised by fever, rapid heart rate, and confusion). For urgent but non-emergency concerns, contact NHS 111 for advice.
Report any suspected side effects from tirzepatide via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Your healthcare team can provide personalised guidance based on your individual circumstances, ensuring that both your thyroid condition and any metabolic concerns are managed safely and effectively whilst taking tirzepatide.
There is no official contraindication to using Mounjaro in patients with Graves' disease. However, thyroid function should be stable and well-controlled before starting tirzepatide, and individualised assessment by your healthcare team is essential.
Direct pharmacological interactions between tirzepatide and thyroid medications are not well-documented. Tirzepatide slows gastric emptying, which could theoretically affect absorption of oral medications, though clinically significant interactions with thyroid drugs have not been established.
Patients with stable, treated Graves' disease typically require thyroid function tests (TSH, FT4, FT3) every 6–12 months, or more frequently if treatment has recently been adjusted. Maintain your usual monitoring schedule and report any symptoms of thyroid dysfunction promptly.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.