
Mounjaro (tirzepatide) is a once-weekly injectable medicine licensed in the UK for treating type 2 diabetes in adults. As a dual GIP and GLP-1 receptor agonist, it improves blood sugar control through multiple mechanisms whilst often promoting weight loss. For patients with chronic kidney disease, understanding how Mounjaro interacts with kidney function is essential. Whilst no dose adjustment is required based on renal function alone, careful monitoring and awareness of potential complications remain important. This article examines the safety considerations, monitoring requirements, and practical guidance for using Mounjaro in patients with kidney disease.
Quick Answer: Mounjaro (tirzepatide) does not require dose adjustment based on kidney function alone, but patients with chronic kidney disease need careful monitoring for dehydration and gastrointestinal side effects that could worsen renal impairment.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It is not indicated for type 1 diabetes, diabetic ketoacidosis, or for use in patients under 18 years of age. Mounjaro belongs to a novel class of medications known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists. It is administered once weekly via subcutaneous injection and works through multiple complementary mechanisms to improve glycaemic control.
The drug's mechanism of action involves binding to both GIP and GLP-1 receptors, which are naturally occurring incretin hormones. When blood glucose levels rise after eating, Mounjaro enhances insulin secretion from pancreatic beta cells in a glucose-dependent manner. This means insulin release occurs primarily when blood sugar is elevated, reducing the risk of hypoglycaemia when used alone (though this risk increases when combined with insulin or sulfonylureas). Simultaneously, tirzepatide suppresses glucagon secretion from pancreatic alpha cells, which helps prevent the liver from releasing excess glucose into the bloodstream.
Beyond glucose regulation, Mounjaro slows gastric emptying, which prolongs the feeling of fullness after meals and contributes to reduced calorie intake. This delayed gastric emptying may affect the absorption of oral medications, particularly those requiring rapid absorption or with a narrow therapeutic index. Women using oral contraceptives should use additional non-oral contraceptive methods for 4 weeks after initiation and after each dose increase. Mounjaro also acts on appetite centres in the brain to decrease hunger signals. These combined effects often result in significant weight loss alongside improved blood sugar control. Clinical trials have demonstrated that Mounjaro can reduce HbA1c levels substantially whilst promoting clinically meaningful weight reduction.
For patients with type 2 diabetes, particularly those who have not achieved adequate control with other medications such as metformin or sulfonylureas, Mounjaro represents an important therapeutic option. The MHRA approved tirzepatide based on clinical evidence demonstrating its efficacy and safety profile, as detailed in the Summary of Product Characteristics (SmPC) and European Public Assessment Report (EPAR).
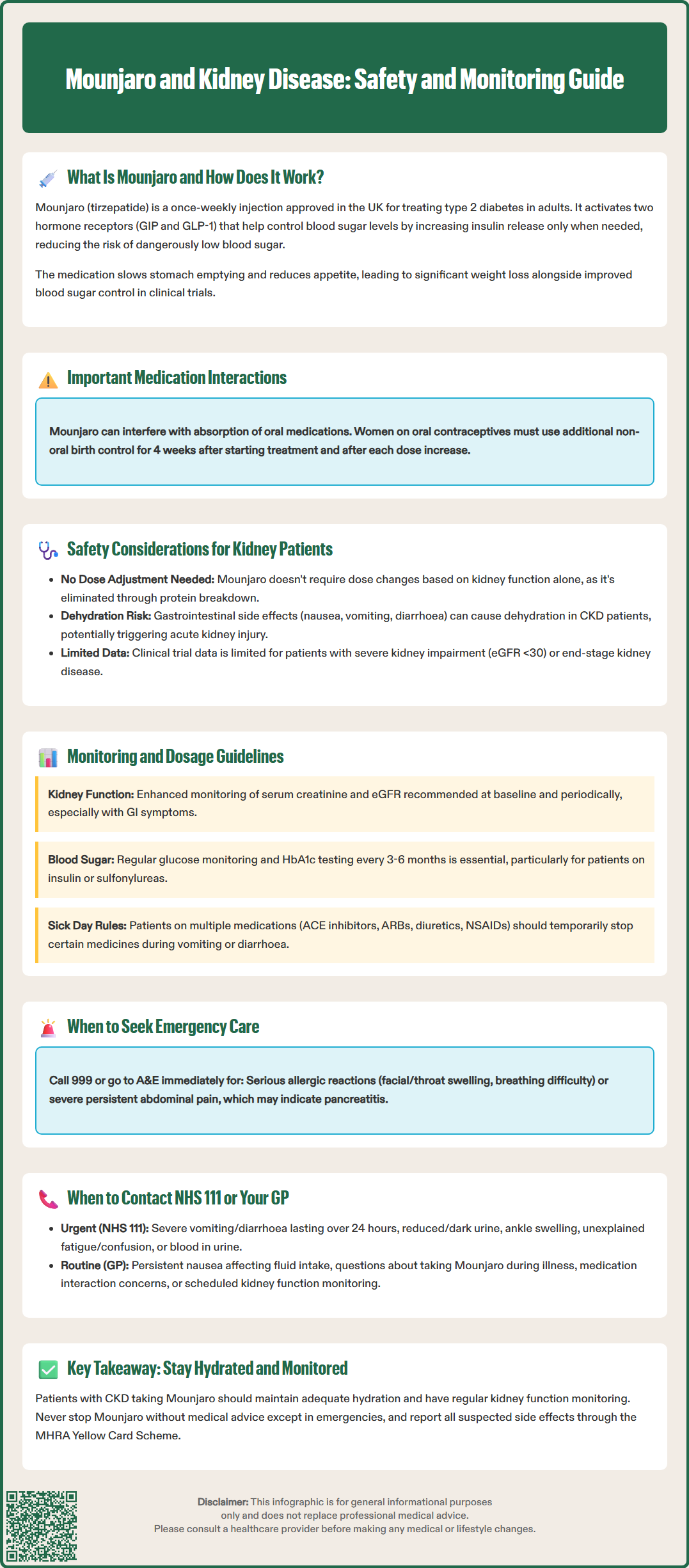
Patients with chronic kidney disease (CKD) require careful consideration when starting any new diabetes medication, and Mounjaro is no exception. According to the SmPC, tirzepatide does not require dose adjustment based solely on renal function, as the drug is primarily eliminated through protein catabolism rather than renal excretion. However, several important safety considerations remain relevant for individuals with impaired kidney function.
Gastrointestinal adverse effects are among the most commonly reported side effects of Mounjaro, including nausea, vomiting, and diarrhoea. These symptoms typically occur during treatment initiation or dose escalation and tend to diminish over time. For patients with existing kidney disease, severe or persistent gastrointestinal symptoms pose particular concern because dehydration from vomiting or diarrhoea can precipitate acute kidney injury (AKI) or worsen pre-existing renal impairment. Maintaining adequate hydration is therefore essential, and patients should be counselled about recognising early warning signs of dehydration.
While there is no established pattern of direct nephrotoxicity with tirzepatide, rare cases of AKI have been reported with GLP-1 receptor agonists, typically in the context of severe dehydration. The SmPC advises monitoring renal function in patients with renal impairment who develop severe gastrointestinal adverse events. Patients with severe renal impairment (eGFR <30 mL/min/1.73m²) or end-stage kidney disease were underrepresented in initial clinical trials, so clinical experience in these populations remains more limited.
Acute pancreatitis is a rare but serious potential adverse effect of GLP-1 receptor agonists including tirzepatide. Patients should be informed about symptoms of acute pancreatitis (severe, persistent abdominal pain, sometimes radiating to the back, with or without vomiting) and advised to seek urgent medical attention if these occur. Similarly, gallbladder disease has been reported with GLP-1 receptor agonists and may require prompt assessment.
Diabetic kidney disease (diabetic nephropathy) is a common complication of type 2 diabetes. By improving glycaemic control, Mounjaro may help slow the progression of kidney disease over time, though this requires further long-term study. Patients should understand that whilst Mounjaro can be used safely in most cases of kidney disease, individualised assessment by their healthcare team remains essential.
Suspected adverse reactions should be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
For patients with chronic kidney disease, appropriate monitoring is crucial when initiating or continuing Mounjaro therapy. According to the SmPC, no dose adjustment of tirzepatide is required based on renal function alone, including in patients with end-stage kidney disease requiring dialysis, although experience in these patients is limited. The standard dosing schedule begins at 2.5 mg once weekly, with gradual escalation every four weeks (to 5 mg, 7.5 mg, 10 mg, 12.5 mg, and maximum 15 mg) based on glycaemic response and tolerability.
Despite not requiring formal dose adjustment, enhanced monitoring is advisable for patients with moderate to severe CKD. Healthcare professionals should assess renal function (serum creatinine and estimated glomerular filtration rate) at baseline and periodically during treatment, particularly if patients experience significant gastrointestinal symptoms or dehydration. NICE guidance on chronic kidney disease (NG203) recommends monitoring eGFR and albumin-to-creatinine ratio (ACR) at least annually in people with diabetes, with increased frequency if eGFR <60 mL/min/1.73m², ACR ≥3 mg/mmol, or if there is a declining trend in renal function.
Concomitant medications warrant careful review in kidney patients taking Mounjaro. Many individuals with CKD take multiple medications, including ACE inhibitors, angiotensin receptor blockers (ARBs), diuretics, and NSAIDs, all of which can affect kidney function. The combination of dehydration from Mounjaro-related gastrointestinal effects and these medications could theoretically increase AKI risk. Patients should be advised to temporarily withhold certain medications during episodes of acute illness with vomiting or diarrhoea, following UK sick day rules guidance. These typically include SGLT2 inhibitors, ACE inhibitors, ARBs, diuretics, metformin, and NSAIDs (sometimes referred to as 'SADMANS' medicines), though local policies may vary.
Blood glucose monitoring remains important, especially for patients taking Mounjaro alongside other glucose-lowering medications such as insulin or sulfonylureas, which may require dose reduction to prevent hypoglycaemia. Regular HbA1c testing (typically every 3–6 months as per NICE guidance NG28) helps assess treatment effectiveness and guide ongoing management decisions.
Patients should be aware that Mounjaro's effect on gastric emptying may impact the absorption of oral medications, particularly those requiring rapid absorption or with a narrow therapeutic index. Women using oral contraceptives should use additional non-oral contraceptive methods for 4 weeks after initiation and after each dose increase of tirzepatide.
Patients taking Mounjaro should be aware of specific warning signs that warrant prompt medical attention, particularly those relating to kidney health. Understanding when to contact your GP or seek urgent care can prevent serious complications and ensure timely intervention.
Call 999 or go to A&E immediately if you experience:
Symptoms of a serious allergic reaction, including facial or throat swelling with difficulty breathing or swallowing
Severe, persistent abdominal pain (with or without vomiting), which may indicate acute pancreatitis
Contact NHS 111 or seek urgent medical advice if you experience:
Severe or persistent vomiting or diarrhoea lasting more than 24 hours, as this can lead to dehydration and acute kidney injury
Reduced urine output or dark, concentrated urine, which may indicate dehydration or worsening kidney function
Swelling of the ankles or legs (oedema), potentially suggesting fluid retention from kidney problems
Unexplained fatigue, confusion, or shortness of breath, which could indicate severe metabolic disturbance
Blood in the urine (haematuria) or frothy urine, which may signal kidney damage
Contact your GP or diabetes care team for routine concerns such as:
Persistent mild nausea affecting your ability to maintain adequate fluid intake
Questions about managing Mounjaro during intercurrent illness
Concerns about medication interactions, particularly if new drugs are prescribed
Scheduled monitoring appointments for kidney function tests
Patients with pre-existing kidney disease should maintain regular follow-up appointments as recommended by their healthcare team. This typically involves periodic blood tests to monitor kidney function (eGFR and creatinine), urine tests to check for protein (albumin-to-creatinine ratio), and blood pressure monitoring. According to NICE guidance (NG203), referral to nephrology services should be considered if eGFR <30 mL/min/1.73m², ACR >70 mg/mmol, there is a rapid decline in kidney function, or persistent haematuria with proteinuria is present.
Do not stop Mounjaro without medical advice. However, if you experience serious adverse effects such as suspected pancreatitis or allergic reaction, stop taking the medication and seek urgent medical care. Your healthcare team can provide appropriate advice about managing symptoms, adjusting treatment, or considering alternative therapies if necessary. Open communication with your medical professionals ensures safe, effective diabetes management whilst protecting your kidney health.
Report any suspected side effects via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
Yes, Mounjaro can be used in patients with chronic kidney disease without dose adjustment, though careful monitoring for dehydration and gastrointestinal side effects is essential. Patients with severe renal impairment should discuss individualised assessment with their healthcare team.
There is no established pattern of direct kidney damage from Mounjaro. However, severe dehydration from gastrointestinal side effects could potentially worsen existing kidney problems or precipitate acute kidney injury, making adequate hydration important.
Kidney function should be assessed at baseline and monitored periodically during treatment, particularly if gastrointestinal symptoms occur. NICE recommends at least annual monitoring for people with diabetes, with increased frequency if kidney function is already impaired.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.