LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for treating type 2 diabetes mellitus. Whilst not licensed specifically for blood pressure reduction, clinical evidence demonstrates that Ozempic typically produces modest decreases in systolic blood pressure, often 2–5 mmHg. These reductions appear to result from weight loss, improved insulin sensitivity, and potentially increased sodium excretion. Individual responses vary considerably, with more pronounced effects observed in patients with obesity and baseline hypertension. Understanding how Ozempic affects blood pressure is essential for safe prescribing and optimal cardiovascular risk management in patients with type 2 diabetes.
Quick Answer: Ozempic typically reduces systolic blood pressure by 2–5 mmHg in patients with type 2 diabetes, though it is not licensed for hypertension treatment.
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It is important to note that Ozempic is not licensed to treat hypertension or to reduce cardiovascular risk specifically. Beyond its primary role in glycaemic control, Ozempic has been associated with beneficial effects on blood pressure in many patients.
The drug works by mimicking the action of endogenous GLP-1, a hormone that regulates insulin secretion, appetite, and gastric emptying. Clinical data from the SUSTAIN programme suggest that Ozempic typically produces modest reductions in systolic blood pressure, often in the range of 2–5 mmHg. These reductions are thought to result from several interconnected mechanisms: weight loss (which reduces cardiac workload and peripheral resistance), improved insulin sensitivity, and potentially other factors. Some proposed mechanisms include reduced inflammation and effects on the cardiovascular system including natriuresis (increased sodium excretion by the kidneys), though these require further research confirmation.
It is important to note that whilst many patients experience blood pressure reductions, individual responses vary considerably. Some patients may see minimal changes, whilst others—particularly those with obesity and hypertension at baseline—may experience more substantial improvements. The blood pressure-lowering effect is generally considered beneficial for patients with type 2 diabetes, who frequently have comorbid hypertension and elevated cardiovascular risk. However, patients already taking antihypertensive medications may require dose adjustments to prevent hypotension as treatment progresses and weight loss occurs.
Patients should be aware that Ozempic can cause gastrointestinal side effects including nausea, vomiting and diarrhoea, which may lead to dehydration. This dehydration can potentially cause dizziness or hypotension. It is important to maintain adequate fluid intake whilst taking Ozempic and to contact a healthcare professional if experiencing persistent gastrointestinal symptoms.
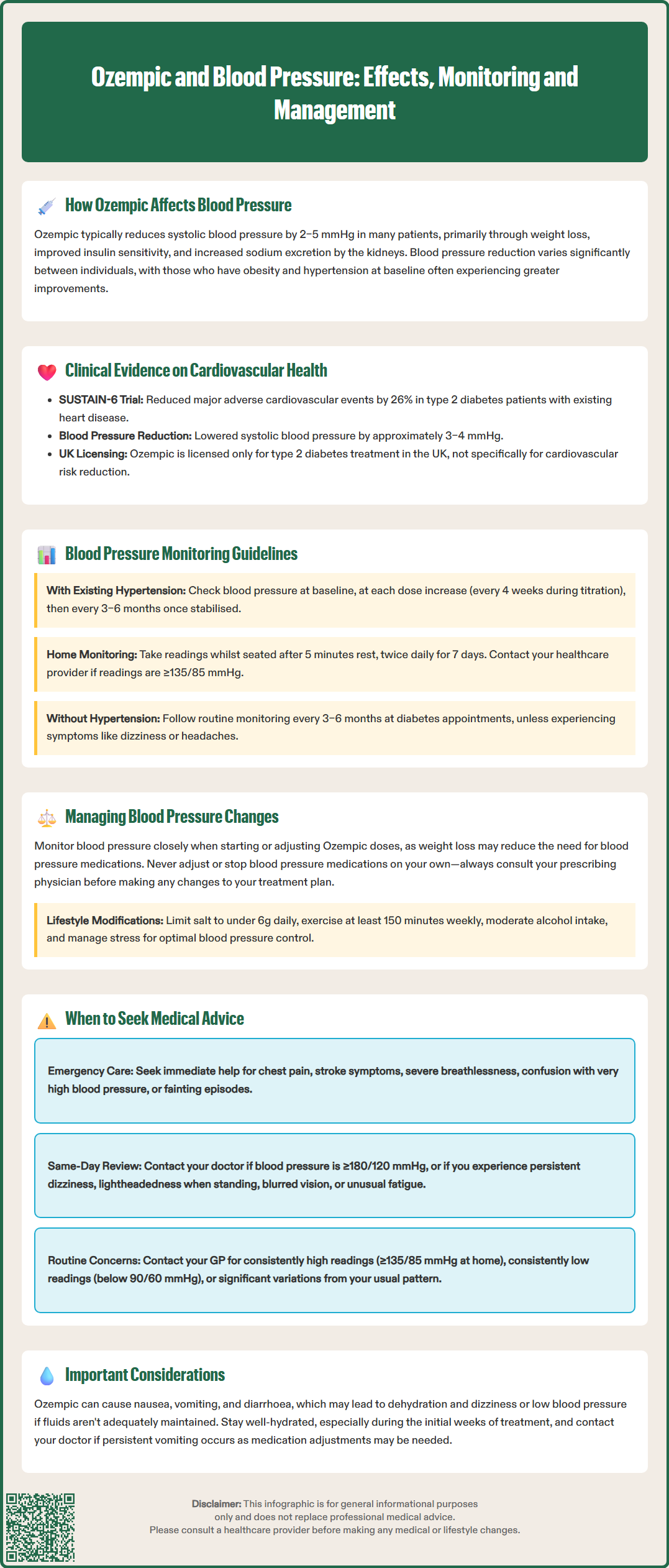
The cardiovascular effects of Ozempic have been evaluated in the SUSTAIN clinical trial programme, most notably the SUSTAIN-6 cardiovascular outcomes trial. This study demonstrated that semaglutide significantly reduced the risk of major adverse cardiovascular events (MACE) by 26% compared with placebo in patients with type 2 diabetes and established cardiovascular disease or multiple cardiovascular risk factors.
Within the SUSTAIN-6 trial, systolic blood pressure reductions of approximately 3–4 mmHg were observed in the semaglutide groups compared with placebo. Importantly, statistical analyses suggested that the cardiovascular benefits extended beyond what could be attributed to blood pressure reduction alone, indicating that Ozempic may influence cardiovascular outcomes through multiple pathways including improved glycaemic control, weight reduction, and effects on lipid profiles.
The Ozempic Summary of Product Characteristics (SmPC) includes the cardiovascular outcomes data from clinical trials. However, it should be emphasised that Ozempic is not licensed in the UK specifically to reduce cardiovascular risk. NICE guidance (NG28) on the management of type 2 diabetes recommends SGLT2 inhibitors with proven cardiovascular benefit as the preferred option for patients with established atherosclerotic cardiovascular disease. GLP-1 receptor agonists, including semaglutide, are options for glycaemic control and weight management where specific criteria are met (as outlined in the relevant NICE Technology Appraisal).
It should be noted that whilst the evidence supports cardiovascular effects, individual patient responses vary. The blood pressure effects appear most pronounced in patients with higher baseline blood pressure and greater degrees of obesity. Patients without hypertension at baseline typically experience minimal blood pressure changes. While Ozempic generally does not cause clinically significant hypotension in normotensive individuals when used as monotherapy, patients should be aware that dehydration from gastrointestinal side effects could potentially lead to reduced blood pressure in some cases.
Regular blood pressure monitoring is advisable for all patients commencing Ozempic, particularly those with pre-existing hypertension or those taking antihypertensive medications. The frequency and intensity of monitoring should be individualised based on baseline cardiovascular risk, concurrent medications, and the presence of comorbidities.
For patients with established hypertension, blood pressure should ideally be measured at baseline before starting Ozempic, then reassessed at each dose escalation (typically every 4 weeks during the titration phase). Once the maintenance dose is achieved and blood pressure readings stabilise, monitoring frequency may be reduced to align with standard hypertension management protocols—generally every 3–6 months, or as recommended by NICE guidelines for hypertension management.
Home blood pressure monitoring can be particularly valuable for patients on Ozempic. Self-monitoring allows for more frequent readings and helps identify trends that might necessitate adjustment of antihypertensive therapy. Patients should be educated on proper technique: measurements should be taken whilst seated after 5 minutes of rest, with the cuff at heart level, and ideally two readings should be taken 1–2 minutes apart. The NHS recommends a standardised approach of twice-daily readings for 7 days, with the average of days 2-7 used for clinical decisions. Home readings of ≥135/85 mmHg (equivalent to clinic readings of ≥140/90 mmHg) should prompt discussion with a healthcare professional.
For patients without baseline hypertension, routine monitoring at regular diabetes review appointments (typically every 3–6 months) is generally sufficient. However, any patient experiencing symptoms potentially related to blood pressure changes—such as dizziness, lightheadedness, or headaches—should have their blood pressure checked promptly. If persistent vomiting or diarrhoea occurs, patients should seek medical advice as these may lead to dehydration, hypotension, and potentially affect kidney function. Healthcare professionals should maintain clear documentation of blood pressure trends to facilitate appropriate medication adjustments and ensure optimal cardiovascular risk management throughout the treatment course.
Proactive management of blood pressure changes is essential when initiating or titrating Ozempic, particularly in patients receiving concurrent antihypertensive therapy. As weight loss progresses and metabolic parameters improve, the need for blood pressure medications may decrease, necessitating careful dose adjustments to prevent hypotension.
For patients taking multiple antihypertensive agents, an individualised approach to medication adjustment is recommended. The decision about which medication to adjust first should be made by the prescribing clinician based on the patient's comorbidities, indications for specific medications (such as nephroprotection), and adverse effect profiles. Medications with additional benefits beyond blood pressure control (such as ACE inhibitors or angiotensin receptor blockers in patients with diabetic nephropathy) are often maintained if well-tolerated. Any medication adjustments should be made in consultation with the prescribing physician and should never be undertaken by patients independently.
Lifestyle modifications remain fundamental to blood pressure management and should be reinforced throughout Ozempic treatment. These include:
Maintaining a balanced diet rich in fruits, vegetables, and whole grains whilst limiting salt intake to less than 6g per day (approximately 2.4g sodium)
Engaging in regular physical activity (at least 150 minutes of moderate-intensity exercise weekly, as tolerated)
Limiting alcohol consumption in line with UK Chief Medical Officers' guidelines
Achieving and maintaining a healthy weight (facilitated by Ozempic's effects on appetite and satiety)
Managing stress through appropriate techniques
Patients should be counselled that blood pressure improvements may develop gradually over several months as weight loss accumulates. Conversely, if blood pressure remains elevated despite Ozempic therapy and lifestyle measures, intensification of antihypertensive treatment may still be necessary. Patients should maintain adequate fluid intake, particularly if experiencing gastrointestinal side effects, and seek medical advice if unwell with persistent vomiting or diarrhoea. In such situations, temporary adjustments to interacting medicines (such as diuretics) may be necessary to reduce the risk of dehydration and acute kidney injury. Regular review ensures that blood pressure management is optimised alongside diabetes control, providing comprehensive cardiovascular risk reduction.
Patients taking Ozempic should be educated about specific circumstances that warrant prompt medical attention regarding blood pressure changes. Whilst modest blood pressure reductions are generally beneficial and expected, certain situations require professional evaluation to ensure patient safety and optimal treatment outcomes.
Seek emergency care (call 999 or go to A&E) if you experience:
Chest pain, stroke symptoms (face drooping, arm weakness, speech difficulties)
Severe breathlessness
Confusion or severe acute headache with very high blood pressure
Fainting episodes
Arrange same-day clinical review if:
Your blood pressure reading is ≥180/120 mmHg, even without symptoms
You have symptoms of hypotension: persistent dizziness, lightheadedness (especially upon standing), blurred vision, or unusual fatigue
You have postural symptoms: feeling faint or dizzy when moving from sitting to standing
Contact your GP or diabetes specialist nurse for routine concerns such as:
Home blood pressure readings consistently at or above 135/85 mmHg (or clinic readings ≥140/90 mmHg)
Home readings consistently below 90/60 mmHg
Blood pressure readings that show significant variation from your usual pattern
New or worsening symptoms that might be blood pressure-related, even if readings appear normal
Persistent gastrointestinal symptoms (nausea, vomiting, diarrhoea) that may lead to dehydration
Questions about adjusting antihypertensive medications as weight loss progresses
Regular scheduled reviews with your healthcare team are essential for monitoring blood pressure trends and making appropriate medication adjustments. Between appointments, maintain a blood pressure diary if you are monitoring at home, as this provides valuable information for clinical decision-making. Remember that blood pressure management is individualised—your target blood pressure and monitoring frequency should be determined by your healthcare provider based on your age, comorbidities, and overall cardiovascular risk profile. Never discontinue or adjust prescribed medications without professional guidance, as abrupt changes can lead to rebound hypertension or other complications.
If you experience any suspected side effects from Ozempic, these can be reported to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk), which helps monitor the safety of medicines in the UK.
Yes, Ozempic typically produces modest reductions in systolic blood pressure of 2–5 mmHg, though individual responses vary. These reductions result from weight loss, improved insulin sensitivity, and potentially increased sodium excretion, though Ozempic is not licensed specifically for blood pressure reduction in the UK.
Patients with established hypertension should have blood pressure measured at baseline and at each dose escalation (typically every 4 weeks during titration), then every 3–6 months once stabilised. Those without baseline hypertension generally require monitoring only at routine diabetes reviews every 3–6 months, unless symptoms develop.
Ozempic generally does not cause clinically significant hypotension in normotensive individuals when used as monotherapy. However, patients taking antihypertensive medications may require dose adjustments as weight loss progresses, and dehydration from gastrointestinal side effects can potentially lead to reduced blood pressure in some cases.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.