Patients who have undergone gastric bypass surgery may experience weight regain or inadequate weight loss, prompting questions about additional treatment options. Ozempic (semaglutide), a GLP-1 receptor agonist licensed for type 2 diabetes management, can be prescribed after bariatric surgery, though this requires careful specialist assessment. The decision to combine these interventions depends on multiple factors including time since surgery, degree of weight regain, presence of comorbidities, and nutritional status. This article examines the clinical considerations, safety profile, and outcomes when Ozempic is used following gastric bypass surgery, alongside NHS guidance for post-bariatric medication management.
Quick Answer: Ozempic can be prescribed after gastric bypass surgery for patients with type 2 diabetes, though this requires specialist assessment and careful monitoring for gastrointestinal effects and nutritional deficiencies.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) can be prescribed after gastric bypass surgery, though this decision requires careful clinical assessment by a specialist or GP. It's important to note that Ozempic is licensed specifically for type 2 diabetes management, not for obesity alone, so its use for post-bariatric weight regain would be considered off-label in the UK.
The decision to initiate Ozempic post-bariatric surgery depends on several factors:
Time since surgery – typically considered after weight stabilisation, which varies between centres but often occurs 12–18 months post-operatively
Degree of weight regain – evidence of significant weight regain or failure to achieve target weight loss
Presence of comorbidities – persistent or recurrent type 2 diabetes, hypertension, or other obesity-related conditions
Nutritional status – adequate vitamin and mineral levels, as gastric bypass affects nutrient absorption and Ozempic can reduce appetite
While there is no absolute contraindication to using Ozempic after gastric bypass, the MHRA/EMC SmPC notes several important cautions, including history of pancreatitis, gallbladder disease, diabetic retinopathy, and severe gastrointestinal disease. Ozempic is not recommended during pregnancy or breastfeeding.
The subcutaneous injection route of Ozempic bypasses concerns about oral medication absorption, which can be problematic after bariatric surgery. However, the effects on gastric emptying and satiety require monitoring.
Patients should be under the care of a multidisciplinary team, ideally including a bariatric surgeon, endocrinologist, dietitian, and specialist nurse. This ensures comprehensive assessment of nutritional status, medication appropriateness, and ongoing monitoring for adverse effects. Referral to Tier 3/4 weight management services may be required for specialist assessment.
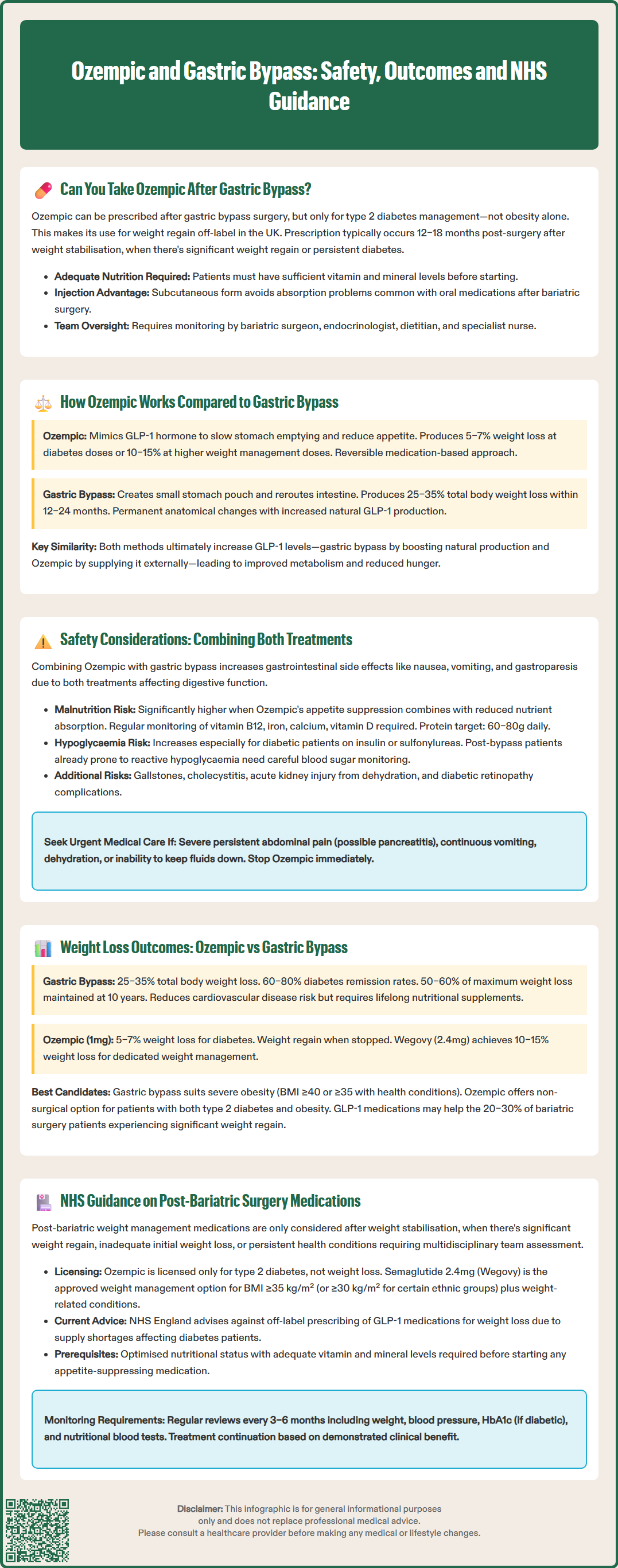
Ozempic and gastric bypass achieve weight loss through fundamentally different mechanisms, though both ultimately affect appetite regulation and metabolic function.
Ozempic (semaglutide) mechanism of action:
Ozempic is a glucagon-like peptide-1 (GLP-1) receptor agonist that mimics the naturally occurring incretin hormone GLP-1. It works by:
Slowing gastric emptying – food remains in the stomach longer, promoting satiety
Reducing appetite – acting on brain receptors in the hypothalamus to decrease hunger signals
Enhancing insulin secretion – glucose-dependent insulin release improves glycaemic control
Suppressing glucagon – reduces hepatic glucose production
Promoting weight loss – typically 5–7% of body weight at licensed doses (0.5–1mg) for type 2 diabetes in the SUSTAIN clinical trials
It's important to note that semaglutide 2.4mg (Wegovy), licensed specifically for weight management, achieves greater weight loss (10–15% in the STEP trials) than the lower Ozempic doses used for diabetes.
Gastric bypass (Roux-en-Y) mechanism:
Gastric bypass is a surgical procedure that creates a small stomach pouch and reroutes the small intestine. Weight loss occurs through:
Mechanical restriction – the smaller stomach pouch limits food intake capacity
Malabsorption – bypassing portions of the small intestine reduces calorie and nutrient absorption
Hormonal changes – altered gut hormone profiles, including increased endogenous GLP-1, PYY, and decreased ghrelin
Metabolic effects – improvements in insulin sensitivity often occur before significant weight loss
Greater weight loss – typically 25–35% of total body weight within 12–24 months
The key distinction is that gastric bypass produces permanent anatomical changes with more substantial weight loss, whilst Ozempic offers a reversible, pharmacological approach. Interestingly, both interventions increase GLP-1 levels—gastric bypass through enhanced endogenous production, and Ozempic through exogenous administration.
Combining Ozempic with previous gastric bypass surgery requires careful monitoring for several potential safety concerns, though serious complications are uncommon when appropriately managed.
Gastrointestinal adverse effects:
Both gastric bypass and Ozempic affect gastrointestinal function, potentially leading to:
Nausea and vomiting – the most common side effects of Ozempic, which may be more pronounced in post-bariatric patients with altered anatomy
Gastroparesis – Ozempic slows gastric emptying; the SmPC advises caution in patients with pre-existing gastroparesis or severe gastrointestinal disease
Dumping syndrome – post-bypass patients may experience early or late dumping syndrome; the effects of GLP-1 receptor agonists on these symptoms vary between patients
Important safety warnings from the SmPC:
Pancreatitis – stop Ozempic immediately and seek urgent medical advice if severe, persistent abdominal pain (possibly radiating to the back) occurs
Gallbladder disease – increased risk of gallstones and cholecystitis
Dehydration – may occur with gastrointestinal side effects, potentially leading to acute kidney injury
Diabetic retinopathy – risk of complications, particularly with rapid improvement in glucose control
Nutritional and metabolic concerns:
Malnutrition risk is heightened when appetite suppression from Ozempic combines with reduced absorption from gastric bypass. Regular monitoring should include:
Vitamin B12, folate, iron, calcium, and vitamin D levels
Protein intake assessment (target 60–80g daily as per BOMSS guidance)
Thiamine status, particularly if vomiting occurs
Bone density screening as appropriate
Hypoglycaemia can occur, especially in patients with type 2 diabetes taking other glucose-lowering medications. Insulin or sulfonylurea doses may need reduction when starting Ozempic. Post-bariatric patients may already experience reactive hypoglycaemia, which requires careful monitoring.
Patients should stop taking Ozempic and contact NHS 111, their GP, or attend A&E immediately if they experience persistent vomiting, inability to maintain hydration, severe abdominal pain (especially if radiating to the back), signs of hypoglycaemia, or symptoms of nutritional deficiency. Suspected side effects should be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Gastric bypass surgery typically produces greater and more sustained weight loss compared to Ozempic monotherapy, though both interventions demonstrate clinically significant benefits for appropriate patients.
Gastric bypass outcomes:
Clinical evidence demonstrates that Roux-en-Y gastric bypass achieves:
Total body weight loss of 25–35% within 12–24 months post-surgery
Excess weight loss of 60–70% in most patients
Long-term maintenance – approximately 50–60% of maximum weight loss maintained at 10 years, according to the Swedish Obese Subjects (SOS) study
Diabetes remission – 60–80% of patients with type 2 diabetes achieve remission or significant improvement, though definitions of remission vary between studies
Cardiovascular benefits – reduced risk of myocardial infarction, stroke, and cardiovascular mortality
Ozempic outcomes:
The SUSTAIN clinical trial programme for semaglutide at diabetes doses (0.5–1mg weekly) showed:
Mean weight loss of 5–7% of body weight over 30–56 weeks
HbA1c reductions of approximately 1.0–1.5% in patients with type 2 diabetes
Weight regain – typically occurs if medication is discontinued, as the pharmacological effect is reversible
By comparison, semaglutide 2.4mg weekly (Wegovy), specifically licensed for weight management, achieved 10–15% weight loss in the STEP trials.
Comparative considerations:
Gastric bypass is generally more effective for patients with severe obesity (BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities) who meet surgical criteria as outlined in NICE CG189. However, it carries surgical risks, requires lifelong nutritional supplementation, and involves permanent anatomical changes.
Ozempic offers a non-surgical alternative suitable for patients with type 2 diabetes and obesity. For those seeking weight management without diabetes, semaglutide 2.4mg (Wegovy) is the licensed option, subject to NICE TA875 eligibility criteria.
For post-bariatric patients experiencing weight regain, limited observational evidence suggests GLP-1 receptor agonists may provide additional weight loss, helping to restore some of the initial surgical benefit. This represents a potential therapeutic option for the estimated 20–30% of bariatric patients who experience significant weight regain.
The NHS provides structured guidance for managing patients after bariatric surgery, including considerations for additional weight management medications, though specific protocols may vary between bariatric centres.
NICE guidance framework:
Relevant NICE recommendations include:
CG189 (Obesity: identification, assessment and management) – includes bariatric surgery indications and follow-up principles
NG28 (Type 2 diabetes in adults) – supports GLP-1 agonist use for glycaemic control and weight management in suitable patients with diabetes
TA875 (Semaglutide for managing weight) – recommends semaglutide 2.4mg (Wegovy) for adults with at least one weight-related condition and a BMI of at least 35 kg/m² (or 30 kg/m² for certain ethnic groups), within specialist weight management services
Post-bariatric medication principles:
NHS bariatric services typically follow these principles when considering additional medications:
Timing – generally not initiated until weight stabilisation occurs, which varies between centres
Indication – clear clinical need, such as significant weight regain, inadequate initial weight loss, or persistent comorbidities
Multidisciplinary assessment – review by bariatric team including surgeon, physician, dietitian, and psychologist
Nutritional optimisation – ensuring adequate vitamin and mineral status before initiating appetite-suppressing medications
Monitoring protocols – regular follow-up for efficacy, adverse effects, and nutritional parameters
Prescribing considerations:
Ozempic is currently licensed for type 2 diabetes, not obesity alone. For weight management, semaglutide 2.4mg (Wegovy) is the licensed option, subject to NICE TA875 criteria. NHS prescription typically requires:
For Ozempic: diagnosis of type 2 diabetes
For Wegovy: specialist recommendation through tier 3/4 weight management services and meeting NICE TA875 criteria
Meeting local commissioning criteria
It's important to note that current NHS England guidance advises against off-label prescribing of GLP-1 receptor agonists for weight loss due to supply constraints affecting patients with diabetes.
Patients should expect regular monitoring appointments (typically every 3–6 months) including weight, HbA1c (if diabetic), blood pressure, and nutritional blood tests. Treatment continuation depends on demonstrating clinical benefit according to local or NICE criteria.
Access to post-bariatric medications varies across NHS regions due to commissioning decisions. Patients experiencing weight regain or inadequate weight loss should discuss options with their bariatric team or GP, who can refer to specialist services if appropriate.
Ozempic can be safely prescribed after gastric bypass surgery with appropriate specialist monitoring, though patients require careful assessment for gastrointestinal side effects, nutritional deficiencies, and potential complications such as pancreatitis or gallbladder disease. Multidisciplinary team oversight is essential to ensure adequate vitamin and mineral status alongside medication management.
Gastric bypass surgery typically produces greater weight loss (25–35% of total body weight) compared to Ozempic at diabetes doses (5–7% body weight loss). Gastric bypass creates permanent anatomical changes with long-term results, whilst Ozempic offers a reversible pharmacological approach that requires ongoing treatment to maintain benefits.
NHS prescription of Ozempic after gastric bypass requires a diagnosis of type 2 diabetes, as it is licensed for diabetes management rather than obesity alone. For weight management specifically, semaglutide 2.4mg (Wegovy) may be available through specialist tier 3/4 weight management services if you meet NICE TA875 eligibility criteria and local commissioning arrangements.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.