Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for managing type 2 diabetes mellitus. Whilst most patients experience weight reduction as a secondary benefit, some individuals report unexpected weight gain during treatment, which can be both frustrating and concerning. Several factors may contribute to this paradoxical response, including compensatory eating patterns, reduced physical activity due to gastrointestinal side effects, concurrent medications, and individual metabolic variation. Understanding the underlying cause is essential, and discussing any weight changes with your GP ensures proper diabetes management whilst addressing your concerns about treatment outcomes.
Quick Answer: Weight gain on Ozempic can occur due to compensatory eating patterns, reduced physical activity from gastrointestinal side effects, concurrent medications, or improved glycaemic control reducing glucose loss in urine.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for managing type 2 diabetes mellitus. While it often leads to weight reduction as a secondary benefit, some individuals report unexpected weight gain during treatment, which can be both frustrating and concerning.
While most patients experience weight loss on Ozempic, weight gain can occur in some cases. Several factors may contribute to this paradoxical response. The medication works by slowing gastric emptying, enhancing insulin secretion in a glucose-dependent manner, and reducing appetite through central nervous system pathways. However, individual responses vary considerably based on metabolic factors, lifestyle habits, concurrent medications, and underlying health conditions.
It is important to recognise that weight fluctuations during the initial weeks of treatment are normal as your body adjusts to the medication. Changes in bowel habits or compensatory eating behaviours may influence the number on the scales. Additionally, some patients may experience reduced physical activity due to gastrointestinal side effects such as nausea or fatigue, which can inadvertently affect energy balance.
Understanding the underlying cause is essential. Weight gain may not always reflect true fat accumulation—it could represent muscle mass changes or measurement timing variations. If you are experiencing weight gain on Ozempic, it is crucial to discuss this with your GP rather than discontinuing the medication independently, as proper diabetes management remains the primary therapeutic goal.
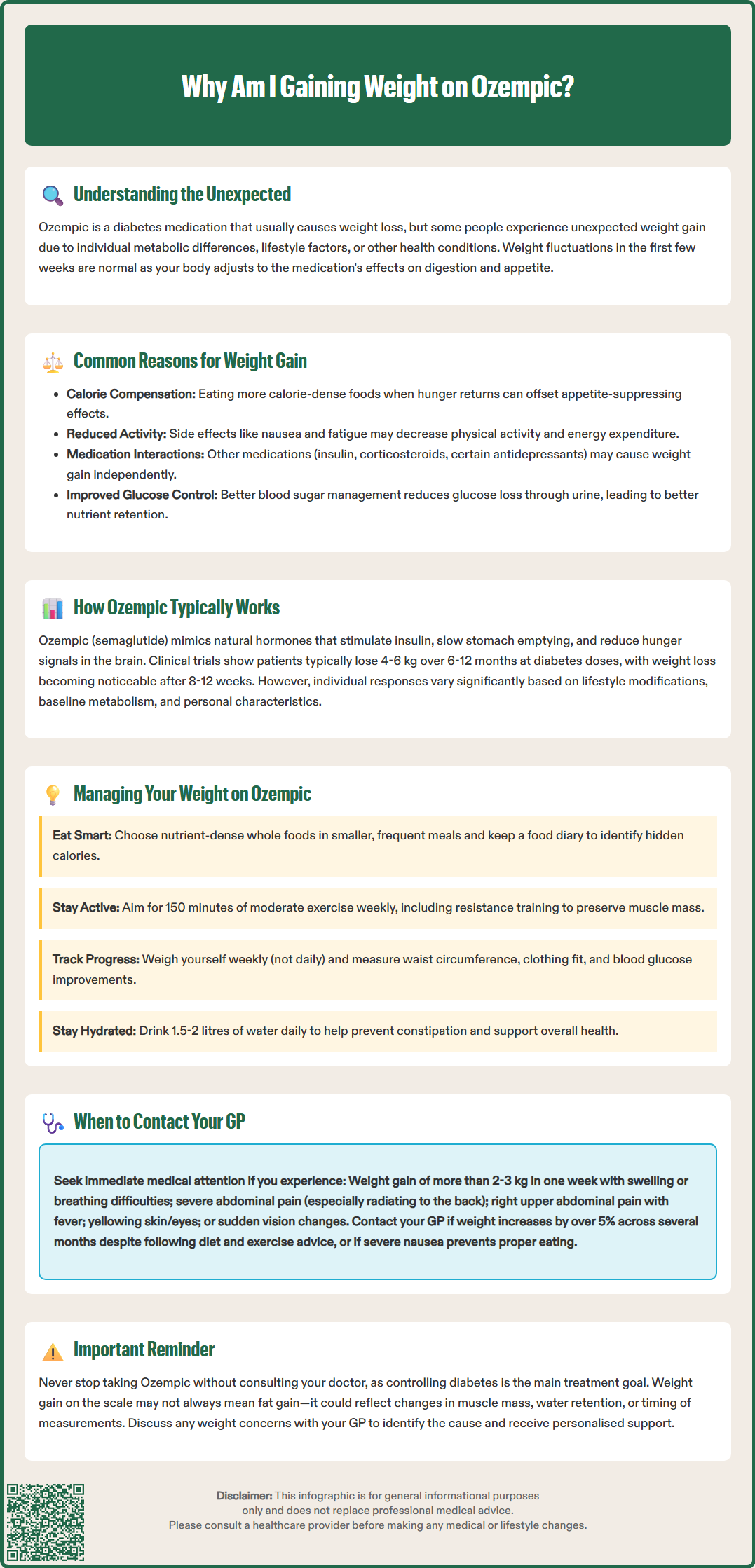
Several physiological and behavioural factors may explain weight gain during Ozempic therapy, even though the medication typically promotes weight loss.
Compensatory eating patterns represent one of the most common causes. Some patients, upon experiencing reduced appetite initially, may later develop patterns of eating more calorie-dense foods during periods when they do feel hungry. The slowed gastric emptying can lead to prolonged feelings of fullness, but when appetite returns, individuals might consume higher-calorie meals to compensate, particularly if they feel they have 'earned' extra food due to previous appetite suppression.
Reduced physical activity often accompanies the gastrointestinal side effects of Ozempic. Nausea, vomiting, diarrhoea, and abdominal discomfort—which occur in varying frequencies depending on dose (more common at higher doses and during titration)—may lead to decreased exercise and general movement. This reduction in energy expenditure can offset the appetite-suppressing effects of the medication.
Concurrent medications may also play a role. Patients taking other medications such as insulin, sulphonylureas, corticosteroids, or certain antidepressants alongside Ozempic may experience weight gain attributable to these agents rather than semaglutide itself. The British National Formulary (BNF) identifies these medications as potentially associated with weight gain.
Improved glycaemic control may reduce glycosuria (glucose loss in urine), leading to better nutrient retention and modest weight increase in some individuals, particularly early in treatment.
If you experience unexplained swelling in your ankles or feet while taking Ozempic, this warrants prompt medical review as it may indicate an underlying condition requiring assessment rather than being a direct medication effect.
To understand why weight gain might occur, it is helpful to appreciate how Ozempic normally facilitates weight reduction in most patients.
Ozempic's mechanism of action involves multiple pathways that influence body weight. As a GLP-1 receptor agonist, semaglutide mimics the action of naturally occurring incretin hormones. It stimulates insulin secretion in a glucose-dependent manner, suppresses inappropriate glucagon release, and slows gastric emptying. Crucially, it acts on appetite centres in the hypothalamus, reducing hunger signals and promoting satiety.
Clinical trials have demonstrated substantial weight loss with semaglutide. In the STEP (Semaglutide Treatment Effect in People with obesity) programme, participants using higher doses of semaglutide (2.4 mg weekly, marketed as Wegovy) achieved average weight reductions of 12-15% over 68 weeks when combined with lifestyle interventions. Even at the lower doses used for diabetes management (0.5-1 mg weekly), patients in the SUSTAIN clinical trials typically experienced 4-6 kg weight loss over 6-12 months.
The weight loss effect is gradual and dose-dependent. Most patients begin with a lower dose (0.25 mg weekly) that is titrated upwards over several weeks to minimise gastrointestinal side effects. Weight loss typically becomes noticeable after 8-12 weeks of treatment, with maximum effects often seen after 6-12 months of consistent use.
Individual variation is considerable. Some patients may experience minimal weight change despite treatment. Adherence to lifestyle modifications, baseline metabolic factors, and other individual characteristics may all influence treatment outcomes. It is worth noting that Ozempic's primary indication remains glycaemic control in type 2 diabetes, with weight loss considered a beneficial secondary effect. For weight management specifically, Wegovy (semaglutide 2.4 mg) is the licensed formulation in the UK, available under NICE guidance (TA875).
Whilst modest weight fluctuations are normal during Ozempic treatment, certain situations warrant prompt medical review.
Contact your GP if you experience:
Rapid weight gain (more than 2-3 kg within a week), particularly if accompanied by swelling in the legs, ankles, or abdomen, shortness of breath, or reduced urine output. These symptoms require urgent assessment to identify the underlying cause.
Persistent weight gain over several months (more than 5% of body weight) despite adherence to dietary and lifestyle recommendations. This may suggest that Ozempic is not the optimal treatment for you, or that other factors require investigation.
Severe or persistent abdominal pain, which may radiate to your back, with or without vomiting. This could indicate pancreatitis, a rare but serious side effect requiring immediate medical attention.
Right upper abdominal pain, fever, or yellowing of the skin/eyes, which may indicate gallbladder problems, as GLP-1 receptor agonists have been associated with an increased risk of gallstone formation.
Sudden changes in vision, particularly if you have diabetic retinopathy, as rapid improvements in blood glucose can sometimes temporarily worsen retinopathy.
Severe gastrointestinal symptoms that limit your ability to maintain adequate nutrition or hydration. Paradoxically, some patients may gain weight by consuming more easily digestible, calorie-dense foods to manage nausea.
Your GP may wish to:
Review your complete medication list to identify potential drug interactions
Assess your dietary intake and physical activity patterns
Arrange blood tests to evaluate thyroid function, kidney function, and glycaemic control
Consider whether dose adjustment or alternative diabetes medications might be more appropriate
Do not discontinue Ozempic without medical guidance, as abrupt cessation may lead to deterioration in blood glucose control. If you are also taking insulin, do not rapidly reduce your insulin dose when starting Ozempic, as this may increase the risk of diabetic ketoacidosis.
For urgent concerns outside of GP hours, contact NHS 111 or 999 in an emergency.
Report any suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Optimising weight outcomes on Ozempic requires a comprehensive approach that extends beyond medication alone.
Dietary strategies remain fundamental. Focus on nutrient-dense, whole foods including vegetables, lean proteins, whole grains, and healthy fats. Because Ozempic slows gastric emptying, eating smaller, more frequent meals may improve tolerance and prevent compensatory overeating later. Keep a food diary for 1-2 weeks to identify patterns—many patients are surprised to discover hidden calorie sources or emotional eating triggers. The NHS Eatwell Guide provides evidence-based recommendations for balanced nutrition.
Physical activity is essential for weight management and overall metabolic health. The UK Chief Medical Officers' Physical Activity Guidelines and NICE recommend at least 150 minutes of moderate-intensity activity weekly for adults with type 2 diabetes. If gastrointestinal side effects limit exercise initially, start with gentle activities such as walking and gradually increase intensity as tolerance improves. Resistance training helps preserve muscle mass during weight loss, which is particularly important for maintaining metabolic rate.
Hydration and timing can influence both weight and medication tolerance. Adequate fluid intake (1.5-2 litres daily for most people, unless advised otherwise by your doctor) helps manage constipation, a common Ozempic side effect. Taking your injection on the same day each week, preferably when you can rest if needed, may help manage any associated nausea.
Monitor progress appropriately. Weigh yourself at the same time of day, ideally weekly rather than daily, to avoid discouragement from normal fluctuations. Consider additional metrics such as waist circumference, how clothing fits, and improvements in blood glucose control and overall wellbeing.
Seek specialist support if needed. Your GP can refer you to a dietitian for personalised nutritional guidance or to a diabetes specialist nurse for medication optimisation. Many areas offer structured diabetes education programmes such as DESMOND (Diabetes Education and Self-Management for Ongoing and Newly Diagnosed), which provide evidence-based strategies for managing both diabetes and weight. Diabetes UK also offers resources and support for people using GLP-1 receptor agonists.
Remember that successful diabetes management encompasses multiple factors beyond weight alone, including cardiovascular risk reduction, prevention of complications, and quality of life.
Yes, whilst most patients experience weight loss on Ozempic, some individuals may gain weight due to compensatory eating patterns, reduced physical activity from gastrointestinal side effects, concurrent medications, or improved glycaemic control reducing glucose loss in urine.
Contact your GP if you experience rapid weight gain (more than 2-3 kg within a week), persistent weight gain over several months despite lifestyle adherence, severe abdominal pain, or swelling in the legs and ankles, as these may indicate underlying conditions requiring assessment.
Focus on nutrient-dense whole foods, eat smaller frequent meals to manage gastric emptying effects, maintain at least 150 minutes of moderate-intensity physical activity weekly, keep a food diary to identify patterns, and ensure adequate hydration to manage common side effects like constipation.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.