
Saxenda slows bowel movements through its action on the digestive system, a recognised effect of this GLP-1 receptor agonist used for weight management. Liraglutide, the active ingredient in Saxenda, delays gastric emptying and reduces gut motility, which contributes to feelings of fullness but can also lead to constipation—affecting at least 1 in 10 patients. Understanding why this occurs and how to manage it effectively allows many people to continue treatment successfully. This article explains the mechanism behind Saxenda's effect on bowel function, provides evidence-based management strategies, and outlines when medical advice should be sought.
Quick Answer: Saxenda slows bowel movements by mimicking GLP-1 hormone, which delays gastric emptying and reduces gut motility, leading to constipation in at least 1 in 10 patients.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereSaxenda (liraglutide 3.0 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities. Whilst Saxenda is effective for weight loss, it commonly affects gastrointestinal function, including bowel movements.
Mechanism of action on the digestive system: Liraglutide works by mimicking the naturally occurring hormone GLP-1, which slows gastric emptying—the rate at which food leaves the stomach and enters the small intestine. This delayed gastric emptying contributes to increased satiety and reduced appetite, supporting weight loss. However, this same mechanism can slow overall gastrointestinal transit time, potentially leading to constipation in some patients. This gastric-emptying effect is typically most pronounced during early treatment and tends to attenuate with continued use.
According to the UK Summary of Product Characteristics (SmPC), gastrointestinal adverse effects are among the most frequently reported with Saxenda. Constipation is classified as very common (affecting ≥1/10 patients), though individual experiences vary considerably. The slowing of bowel movements typically occurs because reduced gut motility allows more water to be absorbed from the stool as it passes through the colon, resulting in harder, less frequent bowel movements.
Other gastrointestinal effects commonly reported include nausea (affecting up to 40% of patients initially), diarrhoea, dyspepsia, and abdominal discomfort. These effects are usually most pronounced during the initial dose escalation phase and often improve as the body adjusts to the medication. It should be noted that Saxenda is not recommended in patients with severe gastrointestinal disease, including severe gastroparesis.
Understanding that altered bowel function is a recognised pharmacological effect of Saxenda can help patients and healthcare professionals anticipate and manage this side effect appropriately.
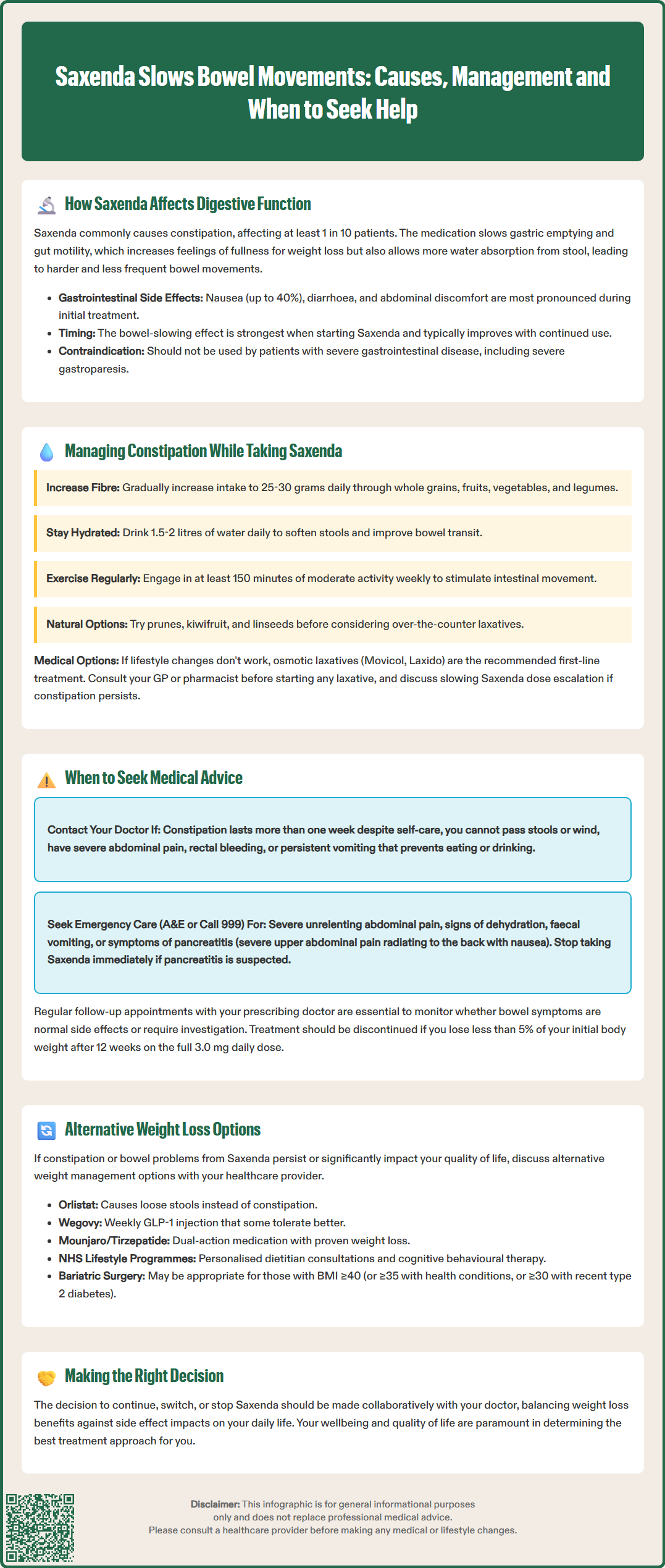
If you experience constipation whilst taking Saxenda, several evidence-based strategies can help restore regular bowel function without necessarily discontinuing treatment.
Dietary modifications form the cornerstone of constipation management:
Increase fibre intake gradually to 25–30 grams daily through wholegrain cereals, fruits, vegetables, pulses, and legumes. Sudden increases may worsen bloating, so introduce fibre-rich foods progressively.
Maintain adequate hydration by drinking 1.5–2 litres of water daily (unless you have a medical condition requiring fluid restriction). Proper hydration helps soften stools and supports normal bowel transit.
Include natural laxative foods such as prunes, kiwifruit, and linseeds, which have mild stool-softening properties.
Lifestyle adjustments also play an important role:
Regular physical activity stimulates intestinal motility. Aim for at least 150 minutes of moderate-intensity exercise weekly, as recommended by UK Chief Medical Officers' guidelines.
Establish a regular toilet routine, allowing sufficient time after meals when the gastrocolic reflex naturally stimulates bowel movements.
Respond promptly to the urge to defecate rather than delaying, which can worsen constipation.
Pharmacological options may be considered if lifestyle measures prove insufficient:
Osmotic laxatives (macrogols such as Movicol, Laxido) are generally first-line for adults with constipation according to NICE Clinical Knowledge Summaries and the BNF. They draw water into the bowel, softening stools.
Bulk-forming laxatives (ispaghula husk, methylcellulose) increase stool mass and may be suitable for those with soft stools who need increased bulk.
Stimulant laxatives (senna, bisacodyl) should be reserved for short-term use when other measures fail, particularly for hard stools when combined with a softener.
Consult your GP or pharmacist before starting any laxative, particularly if you have other medical conditions or take additional medications. If constipation persists despite these measures, discuss with your prescriber whether slowing the dose escalation of Saxenda might improve tolerability while continuing treatment.
Whilst constipation is a very common side effect of Saxenda, certain symptoms warrant prompt medical evaluation to rule out more serious complications or underlying conditions.
Contact your GP or healthcare provider if you experience:
Severe or persistent constipation lasting more than one week despite self-care measures
Complete inability to pass stools or wind, which may indicate bowel obstruction
Severe abdominal pain or distension, particularly if accompanied by vomiting
Rectal bleeding or blood in stools, which requires investigation regardless of presumed cause
Unexplained weight loss beyond expected therapeutic effects, or loss of appetite
Persistent nausea and vomiting that prevents adequate fluid or food intake
Seek urgent medical attention (A&E or call 999) if you develop:
Severe, unrelenting abdominal pain
Signs of dehydration (dizziness, reduced urination, confusion)
Faecal vomiting or inability to tolerate any oral intake
Symptoms suggesting pancreatitis (severe upper abdominal pain radiating to the back, associated with nausea)
It is important to note that Saxenda carries a warning regarding gastrointestinal adverse reactions. Rare but serious complications can include pancreatitis and gallbladder disease, both of which may present with abdominal symptoms. If pancreatitis is suspected, stop taking Saxenda immediately and seek urgent medical attention. The MHRA advises that patients should be counselled about these risks before starting treatment.
Regular follow-up with your prescribing clinician is essential when taking Saxenda. According to the SmPC and in line with NICE guidance (TA664), treatment should be discontinued if less than 5% of initial body weight is lost after 12 weeks on the maintenance dose of 3.0 mg daily. Your healthcare provider can assess whether bowel symptoms represent expected side effects or require further investigation, and can adjust your treatment plan accordingly.
If you experience any suspected side effects from Saxenda, you can report them via the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk.
If constipation or other bowel disturbances persist despite management strategies, or significantly affect your quality of life, alternative approaches to weight management should be discussed with your healthcare provider.
Alternative pharmacological options licensed in the UK include:
Orlistat (Xenical, Alli): A lipase inhibitor that reduces dietary fat absorption. Gastrointestinal effects differ from Saxenda—orlistat commonly causes loose, oily stools rather than constipation. Available on NHS prescription for eligible patients or over-the-counter at lower doses.
Wegovy (semaglutide 2.4 mg): Another GLP-1 receptor agonist, chemically similar to Saxenda but administered weekly rather than daily. Whilst it shares the same mechanism and potential for gastrointestinal effects, some patients tolerate one GLP-1 agonist better than another. NICE (TA875) has approved Wegovy for adults with a BMI of at least 35 kg/m² (or 30 kg/m² with weight-related comorbidities) and at least one weight-related condition, for use within specialist weight management services for a maximum of 2 years.
Mounjaro/Zepbound (tirzepatide): A dual GIP/GLP-1 receptor agonist recently licensed for weight management in the UK. Clinical trials show significant weight loss, though gastrointestinal side effects remain common. At the time of writing, NICE guidance on tirzepatide for weight management is in development.
Non-pharmacological approaches remain fundamental to sustainable weight management:
Structured lifestyle programmes: NICE recommends multicomponent interventions combining dietary modification, increased physical activity, and behavioural strategies. The NHS Digital Weight Management Programme provides evidence-based support for eligible patients referred by their GP.
Dietary approaches: Consultation with a registered dietitian can help develop personalised eating plans, whether low-calorie, Mediterranean-style, or other evidence-based dietary patterns.
Psychological support: Cognitive behavioural therapy (CBT) and other psychological interventions address emotional eating and support long-term behaviour change.
Bariatric surgery: For patients with BMI ≥40 kg/m² (or ≥35 kg/m² with comorbidities) who have not achieved adequate weight loss through other means, surgical options such as gastric bypass or sleeve gastrectomy may be appropriate. NICE guidance (CG189) also recommends considering surgery at lower BMI thresholds (≥30 kg/m²) for people with recent-onset type 2 diabetes. The NHS provides clear eligibility criteria for NHS-funded bariatric surgery.
The decision to continue, switch, or discontinue Saxenda should be made collaboratively with your healthcare provider, weighing the benefits of weight loss against the impact of side effects on your daily life. There is no single optimal approach—effective weight management requires individualised treatment tailored to your specific circumstances, preferences, and medical history.
Saxenda contains liraglutide, which mimics GLP-1 hormone and slows gastric emptying and gut motility. This allows more water to be absorbed from stools in the colon, resulting in harder, less frequent bowel movements.
Gradually increase fibre intake to 25–30g daily, drink 1.5–2 litres of water, engage in regular physical activity, and establish a regular toilet routine. If these measures are insufficient, osmotic laxatives such as macrogols are recommended first-line by NICE.
Contact your GP if constipation persists for more than one week despite self-care, if you cannot pass stools or wind, experience severe abdominal pain or distension, notice rectal bleeding, or develop persistent nausea and vomiting preventing adequate intake.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.