
Mounjaro (tirzepatide) is a GLP-1 and GIP receptor agonist used to treat type 2 diabetes in the UK. If you're scheduled for a colonoscopy, you may wonder whether to continue or pause this medication. Current UK guidance from the Centre for Perioperative Care and the Association of Anaesthetists generally does not recommend routine cessation of GLP-1 receptor agonists before endoscopic procedures. However, individual assessment is important, considering factors such as gastric emptying effects, diabetes control, and procedural safety. This article explains the considerations around Mounjaro use before colonoscopy and provides practical guidance for managing your diabetes during bowel preparation.
Quick Answer: Current UK guidance does not routinely recommend stopping Mounjaro (tirzepatide) before colonoscopy, but individual assessment by your healthcare team is essential.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) is a glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It works by enhancing insulin secretion, suppressing glucagon release, and slowing gastric emptying—an effect that is most pronounced during initial treatment and tends to attenuate with continued use. These mechanisms contribute to its glucose-lowering and weight-reduction effects.
A colonoscopy is an endoscopic examination of the large bowel that requires thorough bowel preparation to ensure clear visualisation of the colonic mucosa. Patients typically consume a bowel-cleansing solution (such as polyethylene glycol or sodium picosulfate) in the hours before the procedure, which induces diarrhoea to empty the colon. The success of the examination depends critically on adequate bowel clearance.
The interaction between Mounjaro and colonoscopy preparation relates to its effects on gastric emptying. Because tirzepatide can delay the movement of food and fluids from the stomach into the small intestine, there are theoretical considerations about how this might affect bowel preparation and procedural safety. UK endoscopy units typically allow clear fluids up to 2 hours before the procedure, and you should always follow the specific fasting instructions provided by your endoscopy unit.
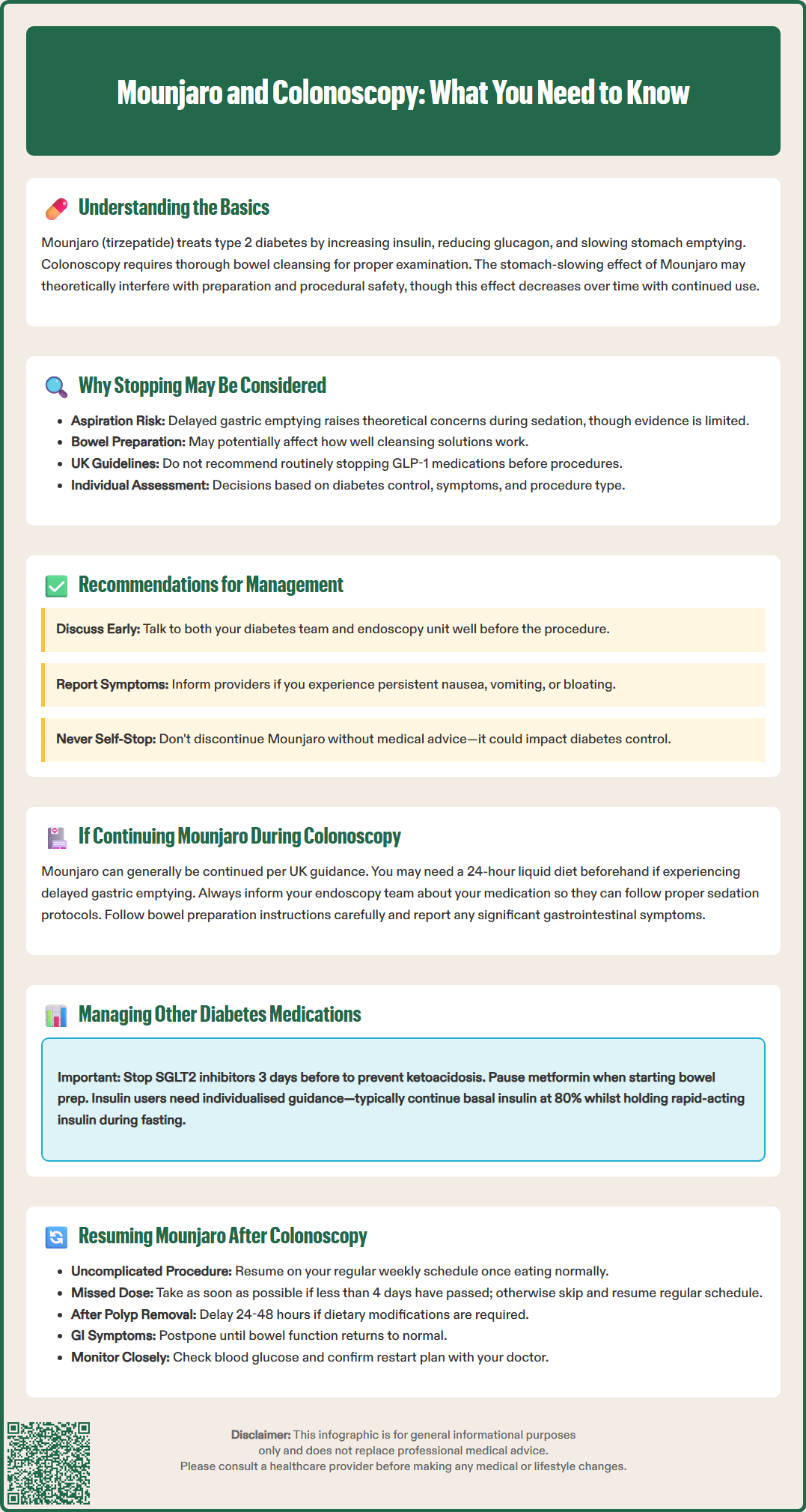
The consideration of whether to continue or pause Mounjaro before colonoscopy relates to its effect on gastric motility. GLP-1 receptor agonists, including tirzepatide, can delay gastric emptying, though this effect may diminish with ongoing treatment.
Some clinicians consider aspiration risk during sedation. During colonoscopy, patients typically receive conscious sedation or, less commonly, general anaesthesia. If the stomach contains residual food or fluid, there is a theoretical risk of regurgitation and pulmonary aspiration. However, the evidence specifically linking GLP-1 receptor agonists to increased aspiration during endoscopic procedures is limited and largely observational.
Another consideration is whether delayed gastric emptying might affect bowel preparation efficacy. If gastric contents move more slowly into the small bowel, the transit of bowel preparation solutions could potentially be affected. Some observational studies suggest variable effects on bowel preparation quality, but robust evidence is limited.
Current UK perioperative guidance from the Centre for Perioperative Care (CPOC) and the Association of Anaesthetists generally does not recommend routine cessation of GLP-1 receptor agonists before procedures. Instead, an individualised approach is recommended, taking into account the patient's diabetes control, any symptoms of significant gastric stasis, and the nature of the procedure. Patients should always discuss their medication regimen with both their diabetes team and the endoscopy team well in advance.
Current UK guidance does not generally recommend routine cessation of GLP-1 receptor agonists like Mounjaro before endoscopic procedures. The Centre for Perioperative Care (CPOC) and Association of Anaesthetists advise that these medications can usually be continued, with management decisions based on individual risk assessment.
If you are taking Mounjaro and scheduled for a colonoscopy, the following approach is recommended:
Discuss with your healthcare team: Consult both your diabetes team and the endoscopy unit about your medications well before the procedure. They will provide guidance based on your individual circumstances and local policies.
Consider your symptoms: If you experience significant gastrointestinal symptoms on Mounjaro (persistent nausea, vomiting, or abdominal distension), inform your healthcare providers as this may influence their recommendations.
Follow local guidance: Some endoscopy units may have specific protocols for patients on GLP-1/GIP receptor agonists. Always follow the instructions provided by your endoscopy unit.
If cessation is advised: In some cases, your healthcare team might recommend omitting the dose immediately preceding your procedure. This decision should be made by your clinicians based on your individual risk factors.
Factors that will be considered include:
Your current glycaemic control and HbA1c
Presence of other diabetes medications
Risk of hyperglycaemia during any interruption period
Your individual risk factors (obesity, gastro-oesophageal reflux disease)
The urgency of the colonoscopy
Never stop Mounjaro without medical guidance, as this may affect your diabetes management.
If you continue Mounjaro up to your colonoscopy, there are several considerations that your healthcare team will take into account. While the UK guidance generally supports continuing GLP-1 receptor agonists for most patients, individual assessment remains important.
Gastric emptying effects may be relevant in some patients. Although these effects typically attenuate with continued treatment, some individuals may still experience delayed gastric emptying. Your endoscopy team may recommend a 24-hour liquid diet before the procedure if there are concerns about gastric emptying.
Sedation considerations are important as conscious sedation is commonly used during colonoscopy. The endoscopy team will follow standard protocols to minimise any theoretical aspiration risk. This includes appropriate positioning during the procedure and careful monitoring.
Bowel preparation effectiveness is crucial for a successful colonoscopy. Some observational studies suggest variable effects of GLP-1 receptor agonists on bowel preparation quality, though evidence is limited. Following your bowel preparation instructions meticulously is particularly important.
From an anaesthetic perspective, your pre-assessment will include questions about your medications and any gastrointestinal symptoms. Be sure to mention if you experience significant nausea, vomiting, or abdominal fullness while taking Mounjaro.
Good communication with healthcare providers is essential. Ensure that your endoscopy team is aware of all your medications, including Mounjaro. This allows for appropriate documentation and procedural planning according to local policies.
Preparing for colonoscopy while managing diabetes requires careful planning, particularly regarding medication adjustments:
SGLT2 inhibitors (e.g., dapagliflozin, empagliflozin, canagliflozin) should be stopped 3 days before the procedure (4 days for ertugliflozin). This is important to reduce the risk of euglycaemic diabetic ketoacidosis. If you've recently been taking an SGLT2 inhibitor, monitor for symptoms of feeling unwell and check ketones if available.
Metformin should typically be omitted when you start clear fluids for bowel preparation and on the day of the procedure. This reduces the risk of dehydration and potential renal issues. Resume metformin once you are eating and drinking normally after the procedure.
If you take Mounjaro as monotherapy (without other diabetes medications), monitor your blood glucose more frequently during any period of medication adjustment—ideally before meals and at bedtime. Contact your diabetes team if readings consistently exceed 15 mmol/L or if you develop symptoms of hyperglycaemia.
On the day of the procedure, follow the fasting instructions provided by your endoscopy unit. UK guidance typically allows clear fluids up to 2 hours before the procedure. If you take morning diabetes medications, discuss with your team whether to omit or reduce doses.
Insulin users require individualised advice—basal insulin is usually continued at a reduced dose (typically 80% of normal), while rapid-acting insulin is held during fasting. The Joint British Diabetes Societies (JBDS) provide detailed guidance on perioperative insulin adjustment.
Your blood glucose will be checked before the procedure and again afterwards. During brief procedures like colonoscopy, significant metabolic disturbance is uncommon. After the procedure, you can usually resume normal eating and your regular diabetes medications once you are fully alert and tolerating oral intake.
Restarting Mounjaro after colonoscopy should be done thoughtfully, considering both procedural recovery and diabetes management needs. In most cases, you can safely resume your normal Mounjaro schedule once you have fully recovered from the procedure and are eating normally.
If your colonoscopy was uncomplicated (no biopsies requiring dietary modification, no significant findings requiring treatment), you can typically restart Mounjaro according to your usual weekly schedule. For example, if your regular injection day is Monday and your colonoscopy was on Thursday, you would resume with your next scheduled Monday dose.
If you missed a dose due to the procedure, follow the guidance in the Mounjaro Summary of Product Characteristics (SmPC): if less than 4 days (96 hours) have passed since the missed dose, administer as soon as possible. If more than 4 days have passed, skip the missed dose and administer the next dose on the regularly scheduled day.
If you underwent polypectomy (polyp removal) or biopsy, your endoscopist may recommend a modified diet for 24–48 hours. In this situation, it may be reasonable to delay restarting Mounjaro until you are back to your normal diet, as the medication's effect on gastric emptying and satiety may make dietary restrictions more challenging to tolerate.
Some patients experience temporary gastrointestinal symptoms after colonoscopy, including bloating, cramping, or altered bowel habit. If these symptoms are significant, discuss with your diabetes team whether to postpone restarting Mounjaro until your bowel function normalises.
Monitor your blood glucose closely in the days after resuming Mounjaro. Always confirm your restart plan with your prescribing clinician before the procedure. Document the interruption and resumption in your diabetes diary, and contact your GP or diabetes team if you have concerns about glycaemic control during the peri-procedural period.
Current UK guidance generally supports continuing Mounjaro before colonoscopy, but you should discuss your individual circumstances with your diabetes team and endoscopy unit. They will assess factors such as your diabetes control, any gastrointestinal symptoms, and local protocols to provide personalised advice.
SGLT2 inhibitors (such as dapagliflozin, empagliflozin, or canagliflozin) must be stopped 3 days before colonoscopy to reduce ketoacidosis risk. Metformin is typically omitted when you start clear fluids for bowel preparation and on the procedure day.
You can usually resume Mounjaro once you have fully recovered from the procedure and are eating normally, following your regular weekly schedule. If you missed a dose and less than 4 days have passed, administer as soon as possible; if more than 4 days have passed, skip the missed dose and continue with your next scheduled injection.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.