
Mounjaro (tirzepatide) may be prescribed after gastric sleeve surgery in selected cases, though this requires careful evaluation by your bariatric team. Whilst there is no absolute contraindication, combining this dual incretin receptor agonist with previous bariatric surgery demands individualised assessment. Some patients experience weight regain or fail to reach target weight loss following sleeve gastrectomy, prompting consideration of additional interventions. Mounjaro is licensed in the UK for weight management in adults with a BMI ≥30 kg/m², or ≥27 kg/m² with weight-related comorbidities, alongside diet and exercise. Any decision to use Mounjaro post-operatively must align with NICE guidance on multidisciplinary obesity management and your overall care plan.
Quick Answer: Mounjaro (tirzepatide) can be prescribed after gastric sleeve surgery in selected cases, but requires careful evaluation by your bariatric team based on weight loss progress, metabolic health, and individual clinical circumstances.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMounjaro (tirzepatide) can potentially be prescribed after gastric sleeve surgery, though this decision requires careful evaluation by your bariatric team and prescribing clinician. There is no absolute contraindication to using Mounjaro following sleeve gastrectomy, but the combination requires individualised assessment based on your weight loss progress, metabolic health, and specific clinical circumstances.
Gastric sleeve surgery (sleeve gastrectomy) is a highly effective bariatric procedure that typically results in significant weight loss during the first 12–24 months post-operatively. However, some patients experience weight regain or fail to achieve their target weight loss, which may prompt consideration of additional interventions. Mounjaro, a glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist, has demonstrated substantial weight loss efficacy in clinical trials.
In the UK, Mounjaro is licensed for weight management in adults with an initial BMI of ≥30 kg/m², or ≥27 kg/m² with at least one weight-related comorbidity, and must be used as an adjunct to a reduced-calorie diet and increased physical activity. It's important to note that NHS access may be restricted pending NICE guidance and local commissioning decisions.
The decision to add Mounjaro after bariatric surgery is not routine and should only be made following comprehensive assessment. NICE guidance on obesity management emphasises a multidisciplinary approach, and any pharmacological intervention post-bariatric surgery must be considered within the context of your overall care plan. Factors influencing this decision include the time elapsed since surgery, adherence to dietary and lifestyle modifications, presence of weight-related comorbidities such as type 2 diabetes, and whether you have reached a weight loss plateau despite optimal behavioural interventions.
It is essential to understand that Mounjaro is not a substitute for the lifestyle changes required after gastric sleeve surgery, but rather a potential adjunct therapy in selected cases where additional metabolic support may be beneficial. Importantly, Mounjaro should not be used concurrently with other GLP-1 receptor agonists.
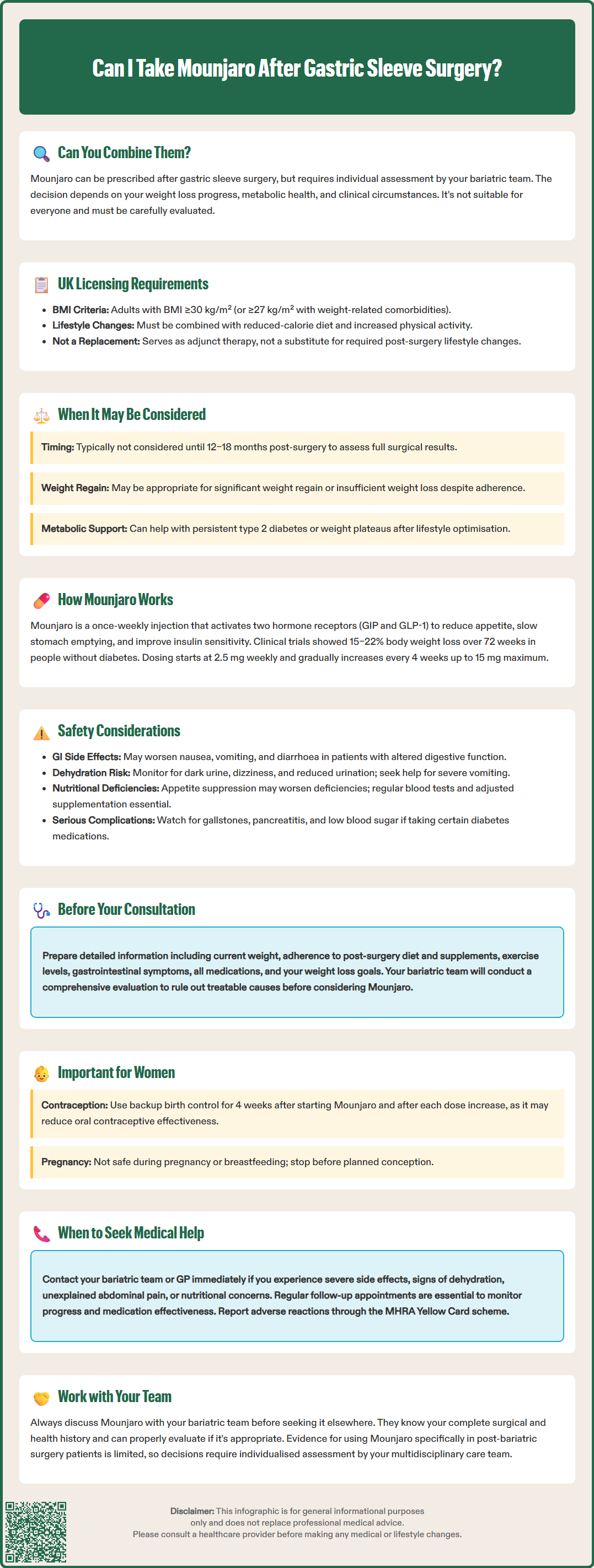
Mounjaro (tirzepatide) is a dual incretin receptor agonist that activates both GIP (glucose-dependent insulinotropic polypeptide) and GLP-1 (glucagon-like peptide-1) receptors. This dual mechanism distinguishes it from other medications in the incretin class and contributes to its effects on weight loss and glycaemic control. The medication is administered as a once-weekly subcutaneous injection, with doses typically starting at 2.5 mg for 4 weeks, then increasing by 2.5 mg every 4 weeks as tolerated, potentially up to 15 mg.
The weight loss mechanisms of Mounjaro are multifaceted. It reduces appetite and food intake by acting on areas of the brain that regulate hunger and satiety, particularly the hypothalamus. Additionally, it slows gastric emptying, which prolongs the sensation of fullness after meals and reduces overall caloric intake. Tirzepatide also improves insulin sensitivity and glucose metabolism, which can be particularly beneficial for patients with type 2 diabetes or prediabetes.
In clinical trials such as the SURMOUNT programme, participants without diabetes achieved average weight loss of 15–22% of their initial body weight over 72 weeks, depending on the dose used. For individuals with type 2 diabetes in the SURPASS trials, weight loss ranged from 7–13% alongside significant improvements in HbA1c levels. These results suggest substantial efficacy, though direct head-to-head comparisons with all other weight loss medications are limited.
Following gastric sleeve surgery, patients already experience changes in gut hormone secretion, including increased GLP-1 levels, which contribute to post-operative weight loss. The addition of Mounjaro theoretically provides supplementary incretin activity, though the clinical benefit of this combination requires careful evaluation. There is currently limited published evidence specifically examining tirzepatide use in post-bariatric surgery populations, making individualised clinical judgement essential.
Importantly, women using oral contraceptives should be aware that Mounjaro's effect on gastric emptying may reduce contraceptive efficacy. Additional contraceptive measures are recommended for 4 weeks after initiation and following each dose increase.
Safety considerations are paramount when contemplating Mounjaro use after gastric sleeve surgery, as both the medication and the surgical procedure affect gastrointestinal function and nutrient absorption. The most common adverse effects of Mounjaro include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, constipation, and abdominal discomfort. These effects are typically most pronounced during dose initiation and escalation, and they may be more problematic in patients who have undergone bariatric surgery and already experience altered gastrointestinal function.
One significant concern is the risk of dehydration and electrolyte disturbances. Both gastric sleeve surgery and Mounjaro can independently cause nausea and vomiting. When combined, there may be an increased risk of inadequate fluid intake, particularly during the early weeks of Mounjaro treatment. Patients must be counselled on maintaining adequate hydration and recognising signs of dehydration, including dark urine, dizziness, reduced urine output, and persistent dry mouth. Severe dehydration can lead to acute kidney injury; renal function should be monitored if significant gastrointestinal losses occur. If severe vomiting occurs, contact your GP or NHS 111, or seek emergency care if symptoms are severe.
Nutritional deficiencies represent another important consideration. Gastric sleeve patients already require lifelong vitamin and mineral supplementation due to reduced food intake and potential malabsorption. The appetite-suppressing effects of Mounjaro may further reduce nutritional intake, potentially exacerbating deficiencies in iron, vitamin B12, folate, calcium, and vitamin D. Regular monitoring of nutritional status through blood tests is essential, and supplementation regimens may need adjustment.
There is also a concern regarding gastroparesis (delayed gastric emptying). Whilst Mounjaro's slowing of gastric emptying is part of its therapeutic mechanism, excessive delay could potentially cause problematic symptoms in post-surgical patients. The SmPC advises caution in patients with severe gastrointestinal disease.
Additional safety considerations include:
Gallbladder disease: Tirzepatide and weight loss can increase the risk of gallstones. Report right upper abdominal pain, fever, or jaundice promptly.
Pancreatitis: The MHRA advises caution with GLP-1 receptor agonists in patients with a history of pancreatitis. Any unexplained severe abdominal pain should prompt immediate medical evaluation.
Hypoglycaemia: If you take insulin or sulfonylureas, these may need dose reduction when starting Mounjaro to prevent low blood glucose.
Pregnancy and breastfeeding: Mounjaro is not recommended during pregnancy or breastfeeding and should be discontinued before planned pregnancy.
Suspected adverse reactions should be reported via the MHRA Yellow Card scheme.
The timing and rationale for introducing Mounjaro after gastric sleeve surgery must be carefully considered within the framework of your overall bariatric care pathway. Generally, pharmacological interventions are not considered during the initial post-operative period when weight loss is typically most rapid. Most bariatric programmes would not contemplate additional weight loss medication until at least 12–18 months post-surgery, allowing adequate time to assess the full effect of the surgical intervention and establish stable eating patterns.
Specific scenarios where Mounjaro might be considered include:
Insufficient weight loss: Patients who have not achieved expected weight loss by 12–18 months post-operatively despite adherence to dietary and lifestyle recommendations (some services use thresholds such as 50% excess weight loss, though criteria vary)
Weight regain: Individuals experiencing significant weight regain after initial successful weight loss
Persistent type 2 diabetes: Patients whose diabetes has not achieved remission or adequate control following surgery, particularly if weight loss has been suboptimal
Weight loss plateau: Those who have reached a plateau well above their target weight despite continued adherence to behavioural modifications
Before considering Mounjaro, your bariatric team will typically conduct a comprehensive reassessment including evaluation of dietary adherence, physical activity levels, psychological factors affecting eating behaviours, and potential surgical complications such as gastric sleeve dilation. It is crucial to exclude treatable causes of inadequate weight loss, such as undiagnosed eating disorders, medication-induced weight gain, or endocrine disorders like hypothyroidism or Cushing's syndrome.
NICE guidance emphasises that pharmacological interventions for obesity should only be used as part of a comprehensive weight management programme. This principle applies equally to post-bariatric surgery patients, meaning Mounjaro would be considered alongside continued dietary counselling, physical activity support, and behavioural therapy rather than as a standalone intervention.
It's important to note that robust evidence specifically examining tirzepatide in post-bariatric surgery populations is currently limited, and decisions should be guided by multidisciplinary team assessment of individual risk-benefit profiles.
Open communication with your bariatric team is essential if you are considering Mounjaro after gastric sleeve surgery. Your multidisciplinary team, which typically includes a bariatric surgeon, specialist nurse, dietitian, and potentially a psychologist, is best positioned to evaluate whether this medication is appropriate for your individual circumstances. It is important to initiate this conversation rather than seeking Mounjaro through alternative routes, as your bariatric team has comprehensive knowledge of your surgical history, weight loss trajectory, and overall health status.
When discussing Mounjaro with your team, be prepared to provide detailed information about:
Your current weight and weight history since surgery
Adherence to post-operative dietary guidelines and vitamin supplementation
Physical activity levels and any barriers to exercise
Any symptoms you are experiencing, particularly gastrointestinal issues
Medications you are currently taking, including over-the-counter supplements
Your weight loss goals and expectations from additional treatment
Your team will need to assess whether you meet the licensing criteria for Mounjaro, which in the UK includes having a body mass index (BMI) of 30 kg/m² or above, or 27 kg/m² or above with at least one weight-related comorbidity, and must be used alongside a reduced-calorie diet and increased physical activity. They will also evaluate potential contraindications and precautions, including hypersensitivity to tirzepatide or any of the excipients, and cautions such as history of pancreatitis.
Practical considerations will also be discussed, including the cost of treatment (as Mounjaro may not be routinely funded through the NHS for post-bariatric surgery patients), the need for enhanced monitoring of nutritional status, and realistic expectations regarding additional weight loss. Your team may recommend a trial period with clearly defined goals and review points to assess efficacy and tolerability.
If you are a woman of childbearing potential, discuss contraception as Mounjaro is not recommended during pregnancy or breastfeeding. If using oral contraceptives, additional contraceptive measures are advised for 4 weeks after starting Mounjaro and after each dose increase due to potential reduced absorption.
If Mounjaro is deemed appropriate, your bariatric team will coordinate with your GP or an appropriate prescriber to initiate treatment, ensuring proper monitoring protocols are in place. You should contact your bariatric team or GP promptly if you experience severe or persistent side effects, signs of dehydration, unexplained abdominal pain, or any concerns about your nutritional status whilst taking Mounjaro. For urgent concerns, contact NHS 111 or call 999 in an emergency. Regular follow-up appointments will be necessary to monitor your progress, adjust dosing if needed, and ensure the medication is providing meaningful benefit without unacceptable adverse effects.
Most bariatric programmes would not consider Mounjaro until at least 12–18 months post-surgery, allowing adequate time to assess the full effect of the surgical intervention and establish stable eating patterns before introducing additional pharmacological treatment.
Key risks include increased gastrointestinal side effects (nausea, vomiting), dehydration and electrolyte disturbances, worsening nutritional deficiencies, and potential for excessive gastric emptying delay. Regular monitoring of hydration, renal function, and nutritional status is essential.
NHS funding for Mounjaro post-bariatric surgery is not routine and depends on local commissioning decisions and pending NICE guidance. Many patients may need to fund treatment privately, and this should be discussed with your bariatric team and GP.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.