
Wegovy and gastric bypass represent two distinct approaches to managing obesity, each with unique mechanisms and clinical applications. Wegovy (semaglutide 2.4 mg) is a once-weekly GLP-1 receptor agonist injection that reduces appetite and promotes weight loss through hormonal regulation. Gastric bypass surgery permanently alters the stomach and intestine to restrict food intake and reduce nutrient absorption. Understanding how these treatments may be used together—whether Wegovy can support patients before surgery or address weight regain afterwards—is crucial for safe, effective weight management. Both interventions require specialist supervision within multidisciplinary services, as recommended by NICE guidance, to optimise outcomes and minimise risks.
Quick Answer: Wegovy can potentially be used before gastric bypass to optimise pre-operative weight loss or after surgery to manage weight regain, though post-surgical use is off-label and both scenarios require specialist medical supervision.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWegovy (semaglutide 2.4 mg) is a once-weekly subcutaneous injection licensed by the MHRA for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, as an adjunct to a reduced-calorie diet and increased physical activity. It belongs to the glucagon-like peptide-1 (GLP-1) receptor agonist class and works by mimicking the natural hormone GLP-1, which regulates appetite and food intake. Semaglutide acts on receptors in the brain to reduce hunger, increase feelings of fullness, and slow gastric emptying, leading to reduced calorie intake and subsequent weight loss.
Gastric bypass surgery, specifically Roux-en-Y gastric bypass (RYGB), is a bariatric surgical procedure that creates a small stomach pouch and reroutes the small intestine. This dual mechanism restricts the amount of food that can be consumed and reduces nutrient absorption. According to NICE guidance (CG189), bariatric surgery is recommended for adults with a BMI of 40 kg/m² or more, or between 35–40 kg/m² with significant obesity-related comorbidities, provided non-surgical measures have been unsuccessful.
Both interventions aim to achieve substantial, sustained weight loss and improve metabolic health, including type 2 diabetes, hypertension, and dyslipidaemia. However, they differ fundamentally in approach: Wegovy is a pharmacological intervention requiring ongoing administration, whilst gastric bypass is a permanent surgical alteration of the gastrointestinal anatomy. NICE Technology Appraisal 875 recommends semaglutide only within specialist weight management services (tier 3 or 4). Understanding how these two treatments may interact or complement each other is essential for patients and clinicians considering combined or sequential approaches to weight management.
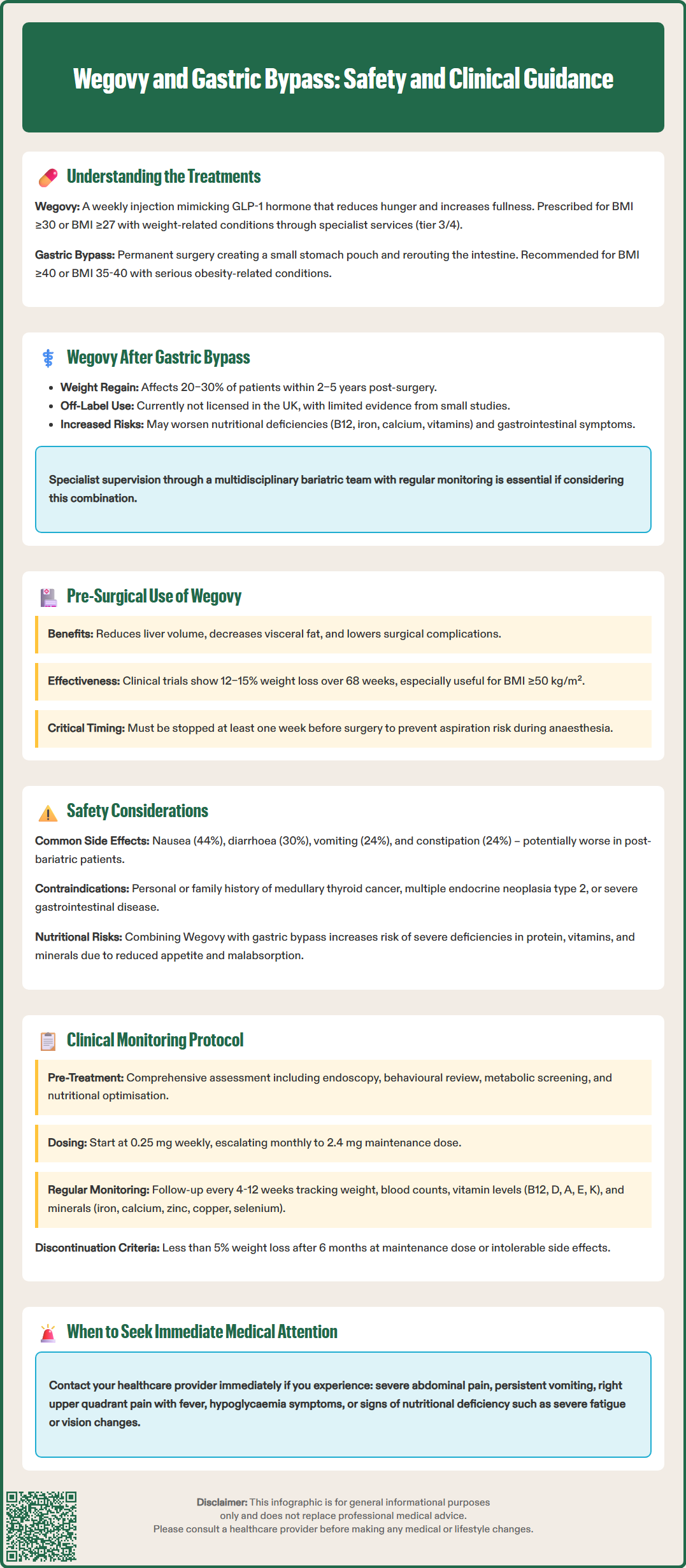
The question of whether Wegovy can be used following gastric bypass surgery is clinically relevant, particularly for patients who experience weight regain or insufficient weight loss after their procedure. Weight regain affects a significant proportion of bariatric surgery patients, with studies suggesting rates of approximately 20–30% within 2–5 years post-operatively, though figures vary by definition and study methodology. Common causes include anatomical changes (such as pouch or anastomosis dilation), behavioural factors, or metabolic adaptation.
It is important to note that using semaglutide after gastric bypass surgery is currently off-label in the UK, as this specific scenario is not included in the MHRA-approved indication. The altered gastrointestinal anatomy does not necessarily preclude the use of subcutaneous GLP-1 receptor agonists, as Wegovy is administered by injection and does not rely on oral absorption. Limited clinical evidence from small observational studies suggests that GLP-1 agonists may have some efficacy in managing post-bariatric weight regain, though robust randomised controlled trials are lacking.
Specialist supervision is essential. Post-bariatric patients have unique physiological considerations, including altered gut hormone profiles, changes in gastric emptying, and potential nutritional deficiencies. The British Obesity and Metabolic Surgery Society (BOMSS) guidelines emphasise monitoring for deficiencies in vitamin B12, iron, calcium, fat-soluble vitamins (A, D, E, K), and trace elements (zinc, copper, selenium). The addition of Wegovy, which further delays gastric emptying and reduces appetite, may exacerbate nutritional risks or gastrointestinal symptoms such as nausea and vomiting.
Patients considering Wegovy after gastric bypass should be managed within a multidisciplinary bariatric service that includes dietitians, bariatric physicians, and surgeons. Regular monitoring of nutritional status, weight trajectory, and tolerability is crucial to optimise outcomes and minimise adverse effects.
Using Wegovy before gastric bypass surgery represents a different clinical scenario, where pharmacological weight loss may serve as part of pre-operative optimisation. NICE guidance (CG189) recommends that patients engage with weight management services before bariatric surgery and suggests that pre-operative weight loss can be beneficial, though it does not mandate a specific amount of weight loss before surgery.
Pre-operative weight loss has been associated with several potential benefits, including:
Reduced liver volume, which improves surgical access and visualisation during laparoscopic procedures
Decreased visceral adiposity, facilitating safer dissection and reducing operative time
Improved metabolic parameters, such as glycaemic control and blood pressure
Lower peri-operative complications, including wound infections and thromboembolic events
Wegovy may be particularly valuable for patients with very high BMI (≥50 kg/m²) or those who struggle to achieve adequate weight loss through diet and exercise alone. The STEP clinical trial programme demonstrated that semaglutide 2.4 mg produces average weight loss of 12–15% over 68 weeks, which could meaningfully reduce surgical risk.
However, there are important considerations. According to the Association of Anaesthetists guidance (2023), Wegovy should be discontinued before surgery, typically at least one week prior to the procedure, due to its effects on gastric emptying, which could increase aspiration risk during anaesthesia. Additionally, the cost-effectiveness of using Wegovy as a pre-surgical intervention has not been formally evaluated in the UK context. The decision should be individualised, considering surgical waiting times, patient risk profile, and local commissioning arrangements.
The effectiveness of combining or sequencing Wegovy with gastric bypass depends on the clinical context. For post-bariatric weight regain, preliminary data suggest that semaglutide may produce additional weight loss, though robust randomised controlled trials are still needed. For pre-operative use, Wegovy's efficacy in achieving clinically meaningful weight loss is well-established from the STEP trial programme, though its specific impact on bariatric surgical outcomes requires further investigation.
Safety considerations are paramount when combining these interventions. According to the Wegovy SmPC, common adverse effects include:
Gastrointestinal symptoms: nausea (44%), diarrhoea (30%), vomiting (24%), constipation (24%), and abdominal pain
Hypoglycaemia risk: particularly in patients with type 2 diabetes on concurrent glucose-lowering medications
Gallbladder disease: increased risk of cholelithiasis and cholecystitis
Pancreatitis: rare but serious adverse effect requiring immediate discontinuation
In post-bariatric patients, these risks may be amplified. The combination of surgically altered anatomy and pharmacologically delayed gastric emptying could worsen gastrointestinal tolerance. Nutritional deficiencies represent a particular concern, as reduced food intake from Wegovy may compound the malabsorptive effects of gastric bypass, potentially leading to protein-energy malnutrition, anaemia, or metabolic bone disease.
Contraindications to Wegovy include personal or family history of medullary thyroid carcinoma, multiple endocrine neoplasia syndrome type 2, and severe gastrointestinal disease. Caution is advised in patients with diabetic retinopathy, renal impairment, or history of pancreatitis. Regular monitoring should include weight, nutritional markers (full blood count, vitamin B12, folate, ferritin, calcium, vitamin D, zinc, copper, selenium, vitamins A, E and K), liver function, and assessment of gastrointestinal symptoms.
The use of Wegovy in relation to gastric bypass surgery should occur only under specialist medical supervision within an established bariatric or weight management service. NICE guidance emphasises that both pharmacological and surgical obesity treatments require comprehensive multidisciplinary support, including dietary counselling, psychological assessment, and long-term follow-up.
For patients considering Wegovy after gastric bypass (noting this is off-label use), the clinical pathway should include:
Comprehensive assessment of weight regain causes, including anatomical evaluation (endoscopy or imaging to assess pouch size and anastomosis), behavioural factors, and metabolic screening
Nutritional optimisation before initiating Wegovy, ensuring adequate protein intake and correction of existing deficiencies
Dose titration following the standard schedule (starting at 0.25 mg weekly, escalating monthly to 2.4 mg), with careful monitoring of tolerance
Regular follow-up every 4–12 weeks to assess weight response, nutritional status, and adverse effects
Discontinuation criteria: if <5% weight loss after 6 months at maintenance dose (as per NICE TA875), or if intolerable side effects occur
For pre-operative use, coordination between the prescribing physician and bariatric surgical team is essential to ensure appropriate timing of discontinuation and to integrate pharmacological weight loss into the overall surgical preparation pathway.
Patients should contact their GP or specialist immediately if they experience severe abdominal pain (possible pancreatitis or gallstones), right upper quadrant pain with fever (cholecystitis), persistent vomiting preventing adequate nutrition or hydration, signs of hypoglycaemia, or symptoms of nutritional deficiency such as severe fatigue, paraesthesia, or visual changes. Adverse effects should be reported through the MHRA Yellow Card Scheme. Self-directed use of Wegovy without medical supervision, particularly in the post-bariatric population, is strongly discouraged due to the complex physiological interactions and monitoring requirements involved.
Wegovy can potentially be used after gastric bypass to manage weight regain, though this is currently off-label use in the UK. It requires specialist supervision within a multidisciplinary bariatric service due to increased risks of nutritional deficiencies and gastrointestinal side effects.
Yes, Wegovy should be discontinued at least one week before gastric bypass surgery due to its effects on gastric emptying, which increases aspiration risk during anaesthesia. Your surgical team will provide specific guidance on timing.
The main risks include worsened gastrointestinal symptoms (nausea, vomiting), increased nutritional deficiencies (vitamins, minerals, protein), gallbladder disease, and potential hypoglycaemia in diabetic patients. Regular monitoring of nutritional status and weight is essential.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.