
Wegovy (semaglutide 2.4 mg) and gastric sleeve surgery represent two distinct approaches to managing obesity, each with proven efficacy in achieving substantial weight loss. Whilst gastric sleeve surgery is a well-established bariatric procedure that reduces stomach capacity and alters gut hormones, Wegovy is a GLP-1 receptor agonist licensed for chronic weight management. Some patients who experience inadequate weight loss or weight regain after gastric sleeve may wonder whether Wegovy could provide additional benefit. However, combining these interventions is not routinely recommended in UK clinical practice, and evidence remains limited. This article examines the rationale, potential benefits, risks, and clinical considerations surrounding the use of Wegovy after gastric sleeve surgery.
Quick Answer: Wegovy is not routinely recommended after gastric sleeve surgery in the UK, though it may be considered by specialist teams for patients with inadequate weight loss or significant weight regain.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA for chronic weight management in adults with obesity or overweight with weight-related comorbidities. It works by mimicking the naturally occurring hormone GLP-1, which regulates appetite and food intake. Semaglutide slows gastric emptying, enhances satiety signals to the brain, and reduces hunger, leading to decreased caloric intake and subsequent weight loss. Administered as a once-weekly subcutaneous injection, Wegovy follows a dose-escalation schedule (starting at 0.25 mg and increasing gradually to 2.4 mg) and is intended as an adjunct to a reduced-calorie diet and increased physical activity within specialist weight management services, as per NICE TA875.
Gastric sleeve surgery (sleeve gastrectomy) is a bariatric surgical procedure that involves removing approximately 75–80% of the stomach, leaving a narrow, tube-shaped 'sleeve'. This restrictive procedure significantly reduces stomach capacity, limiting food intake and promoting early satiety. Additionally, the surgery alters gut hormone production—particularly reducing ghrelin (the 'hunger hormone')—which contributes to appetite suppression and metabolic improvements. Gastric sleeve is one of the most commonly performed bariatric operations in the UK and is typically reserved for individuals with a body mass index (BMI) of 40 kg/m² or above, or 35 kg/m² with significant obesity-related comorbidities. NICE guidance (CG189) also recognises lower BMI thresholds (typically 30-35 kg/m²) for certain groups, including those with recent-onset type 2 diabetes and people of certain ethnic backgrounds.
Both interventions aim to achieve substantial, sustained weight loss and improve obesity-related conditions such as type 2 diabetes, hypertension, and obstructive sleep apnoea. However, they operate through different mechanisms—one pharmacological, the other surgical—and are generally considered distinct treatment pathways rather than complementary therapies in standard clinical practice.
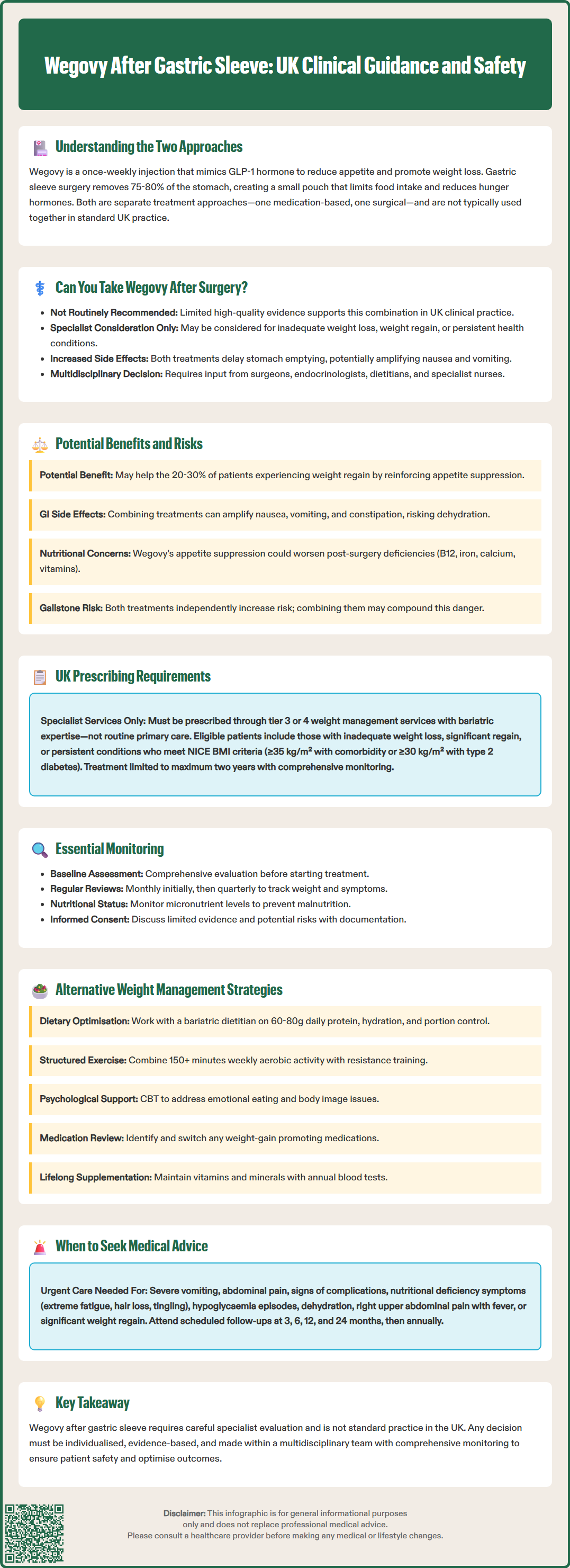
The use of Wegovy following gastric sleeve surgery is not routinely recommended in standard UK clinical practice, and there is currently limited high-quality evidence to support this combination. While the Wegovy SmPC does not specifically exclude patients with prior bariatric surgery, NICE guidance does not advocate for GLP-1 receptor agonists as a standard adjunct following successful bariatric procedures.
That said, there is no contraindication to prescribing semaglutide after gastric sleeve surgery if patients meet the standard criteria for Wegovy treatment. In clinical scenarios where patients experience inadequate weight loss (failure to achieve expected outcomes), weight regain after initial success, or persistent obesity-related comorbidities despite surgery, some specialists may consider pharmacotherapy as part of a comprehensive management plan. This decision would typically be made within a multidisciplinary bariatric team, including bariatric surgeons, endocrinologists, dietitians, and specialist nurses.
It is important to recognise that gastric sleeve surgery already produces significant changes in gut hormone profiles and gastric physiology that overlap with semaglutide's mechanisms of action. Both interventions delay gastric emptying and enhance satiety signalling, raising theoretical concerns about additive gastrointestinal side effects such as nausea, vomiting, and potential nutritional deficiencies. Furthermore, post-operative patients may already be managing complex dietary regimens and supplement schedules, which could complicate medication adherence and monitoring.
Any decision to initiate Wegovy after bariatric surgery must be individualised, evidence-informed, and made collaboratively between the patient and their specialist healthcare team, with careful consideration of potential benefits, risks, and alternative strategies. In accordance with NICE TA875, treatment would need to be provided within a specialist weight management service (Tier 3 or 4) and is typically limited to a maximum of two years.
Potential benefits of using Wegovy after gastric sleeve surgery may include enhanced weight loss in patients who have not achieved their target weight or who experience weight regain—a phenomenon affecting approximately 20–30% of bariatric surgery patients over time according to systematic reviews. Emerging evidence from small observational studies suggests that GLP-1 receptor agonists may help address this 'weight recidivism' by reinforcing appetite suppression and metabolic improvements. Additionally, semaglutide has shown cardiovascular benefits in clinical trials (such as the SELECT trial), though it's important to note that cardiovascular risk reduction is not currently part of the UK licensed indication for Wegovy.
However, significant risks and considerations must be weighed carefully:
Gastrointestinal adverse effects: Both gastric sleeve and semaglutide delay gastric emptying and can cause nausea, vomiting, abdominal discomfort, and constipation. The combination may amplify these effects, potentially leading to dehydration, electrolyte imbalances, or reduced quality of life.
Nutritional deficiencies: Post-bariatric patients are already at increased risk of deficiencies in vitamin B12, iron, calcium, and fat-soluble vitamins due to reduced food intake and altered absorption. Semaglutide-induced appetite suppression and nausea could further compromise nutritional intake, necessitating vigilant monitoring and supplementation.
Gallbladder disease: Both rapid weight loss after bariatric surgery and GLP-1 receptor agonists are associated with increased risk of gallstones and cholecystitis. The Wegovy SmPC highlights this risk, which could potentially be compounded in post-sleeve patients.
Hypoglycaemia risk: While uncommon with semaglutide monotherapy in non-diabetic patients, those taking concurrent diabetes medications (particularly insulin or sulfonylureas) or experiencing post-bariatric reactive hypoglycaemia may face increased risk and require careful monitoring.
Cost and access: Wegovy is prescribed according to NICE TA875 criteria within specialist services, typically for a maximum of two years. Patients must meet specific BMI and comorbidity thresholds for NHS funding.
There is currently no official recommendation established by UK regulatory bodies or clinical guidelines supporting routine combination therapy, and long-term safety data in this population remain limited.
NICE guidance (CG189) on obesity management recommends bariatric surgery for appropriate candidates but does not routinely advocate for pharmacological weight management agents post-operatively. GLP-1 receptor agonists like Wegovy (NICE TA875) are generally positioned as alternatives to surgery or for patients who are not surgical candidates, rather than as adjuncts following bariatric procedures.
If Wegovy is being considered after gastric sleeve surgery, prescribing should occur within a specialist multidisciplinary setting—specifically a tier 3 or tier 4 weight management service with bariatric surgery expertise, as required by NICE TA875. Key considerations include:
Patient selection: Candidates might include those with documented inadequate weight loss, significant weight regain, or persistent obesity-related comorbidities despite surgical intervention. They should meet the standard NICE criteria for Wegovy treatment (BMI ≥35 kg/m² with weight-related comorbidity or ≥30 kg/m² with type 2 diabetes).
Baseline assessment: Comprehensive evaluation should include current BMI, nutritional status (including micronutrient levels), glycaemic control, renal and hepatic function, gastrointestinal symptoms, and psychological wellbeing.
Monitoring protocol: Regular follow-up (initially monthly, then quarterly) to assess weight trajectory, tolerability, nutritional markers, and adherence to dietary and supplement regimens is essential. Particular attention should be paid to signs of malnutrition, dehydration, or worsening gastrointestinal symptoms.
Treatment duration: As per NICE TA875, Wegovy treatment is typically limited to a maximum of two years on the NHS.
Shared decision-making: Patients must be fully informed about the limited evidence base, potential risks, and alternative strategies. Written consent and documentation of discussions are advisable.
Funding and access: NHS funding follows NICE TA875 criteria within specialist services. Patients must meet the specified BMI thresholds and have weight-related comorbidities to qualify for treatment.
Before considering pharmacotherapy like Wegovy, optimising non-pharmacological strategies should be the priority for managing inadequate weight loss or weight regain after gastric sleeve surgery. Evidence-based alternatives include:
Dietary optimisation: Referral to a specialist bariatric dietitian for comprehensive nutritional assessment and tailored meal planning. Focus on high-protein intake (60–80 g daily per British Obesity & Metabolic Surgery Society guidance), adequate hydration, portion control, and avoidance of high-calorie liquids and grazing behaviours. Addressing emotional eating patterns and food choices is crucial.
Physical activity programmes: Structured exercise interventions combining aerobic activity (150+ minutes weekly) and resistance training can enhance weight loss maintenance, preserve lean muscle mass, and improve metabolic health, as recommended by UK Chief Medical Officers' guidelines. Referral to exercise specialists or tier 3 services may be beneficial.
Psychological support: Cognitive behavioural therapy (CBT) or other evidence-based psychological interventions can address underlying eating behaviours, body image concerns, depression, or anxiety that may contribute to weight regain. Many bariatric centres offer integrated psychological services.
Medication review: Certain medications (e.g., antipsychotics, antidepressants, corticosteroids) promote weight gain. Where clinically appropriate, switching to weight-neutral alternatives should be explored with the prescribing clinician.
Revisional surgery: In selected cases of significant weight regain or technical surgical issues (e.g., sleeve dilation), revisional bariatric procedures may be considered, though these carry higher complication risks.
Other pharmacotherapy: Alternative anti-obesity medications such as orlistat may be considered, though evidence post-bariatric surgery is limited and NHS availability varies.
Lifelong supplementation: All post-bariatric patients require lifelong vitamin and mineral supplementation according to BOMSS guidelines, with annual blood tests to monitor nutritional status. This becomes even more critical if additional weight loss interventions are introduced.
A multidisciplinary approach remains the gold standard, with regular engagement with the bariatric team ensuring comprehensive, individualised care.
Patients who have undergone gastric sleeve surgery should maintain regular follow-up with their bariatric team, typically at 3, 6, 12, and 24 months post-operatively, then annually thereafter as recommended by BOMSS. However, urgent medical advice should be sought if any of the following occur:
Severe or persistent gastrointestinal symptoms: Intractable nausea, vomiting (especially if unable to tolerate fluids), severe abdominal pain, or signs of bowel obstruction require immediate assessment to exclude surgical complications such as stricture or gastric leak (sleeve-specific complications).
Signs of nutritional deficiency: Symptoms such as extreme fatigue, hair loss, neurological changes (tingling, numbness, confusion), visual disturbances, or recurrent infections may indicate vitamin or mineral deficiencies requiring urgent investigation and supplementation.
Hypoglycaemia: Episodes of shakiness, sweating, confusion, or loss of consciousness, particularly in patients taking diabetes medications, warrant immediate medical review and potential medication adjustment.
Dehydration: Reduced urine output, dizziness, dry mouth, or concentrated urine may indicate inadequate fluid intake, especially if experiencing nausea or vomiting.
Gallbladder symptoms: Right upper quadrant pain, especially after eating fatty foods, fever, or yellowing of the skin/eyes could indicate gallstones or cholecystitis—risks increased by both rapid weight loss and GLP-1 receptor agonists.
Inadequate weight loss or significant regain: If weight loss plateaus early (within 6–12 months) or substantial weight regain occurs, patients should contact their bariatric team for assessment rather than self-managing.
For patients considering or currently taking Wegovy after gastric sleeve surgery, any new or worsening side effects—particularly severe gastrointestinal symptoms, signs of pancreatitis (severe upper abdominal pain radiating to the back), or allergic reactions—require prompt medical evaluation. Your GP or bariatric specialist can provide guidance, adjust treatment plans, or arrange appropriate investigations to ensure safe, effective ongoing care.
Wegovy is not contraindicated after gastric sleeve surgery, but it is not routinely recommended in UK practice. Specialist bariatric teams may consider it for patients with inadequate weight loss or weight regain, with careful monitoring for additive gastrointestinal side effects and nutritional deficiencies.
Approximately 20–30% of bariatric surgery patients experience weight regain over time. Wegovy may be considered in specialist settings to address inadequate weight loss, significant weight regain, or persistent obesity-related comorbidities despite surgical intervention.
Key risks include amplified gastrointestinal symptoms (nausea, vomiting), worsening nutritional deficiencies, increased gallbladder disease risk, and potential hypoglycaemia in patients taking diabetes medications. Close monitoring within a specialist multidisciplinary team is essential.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.