
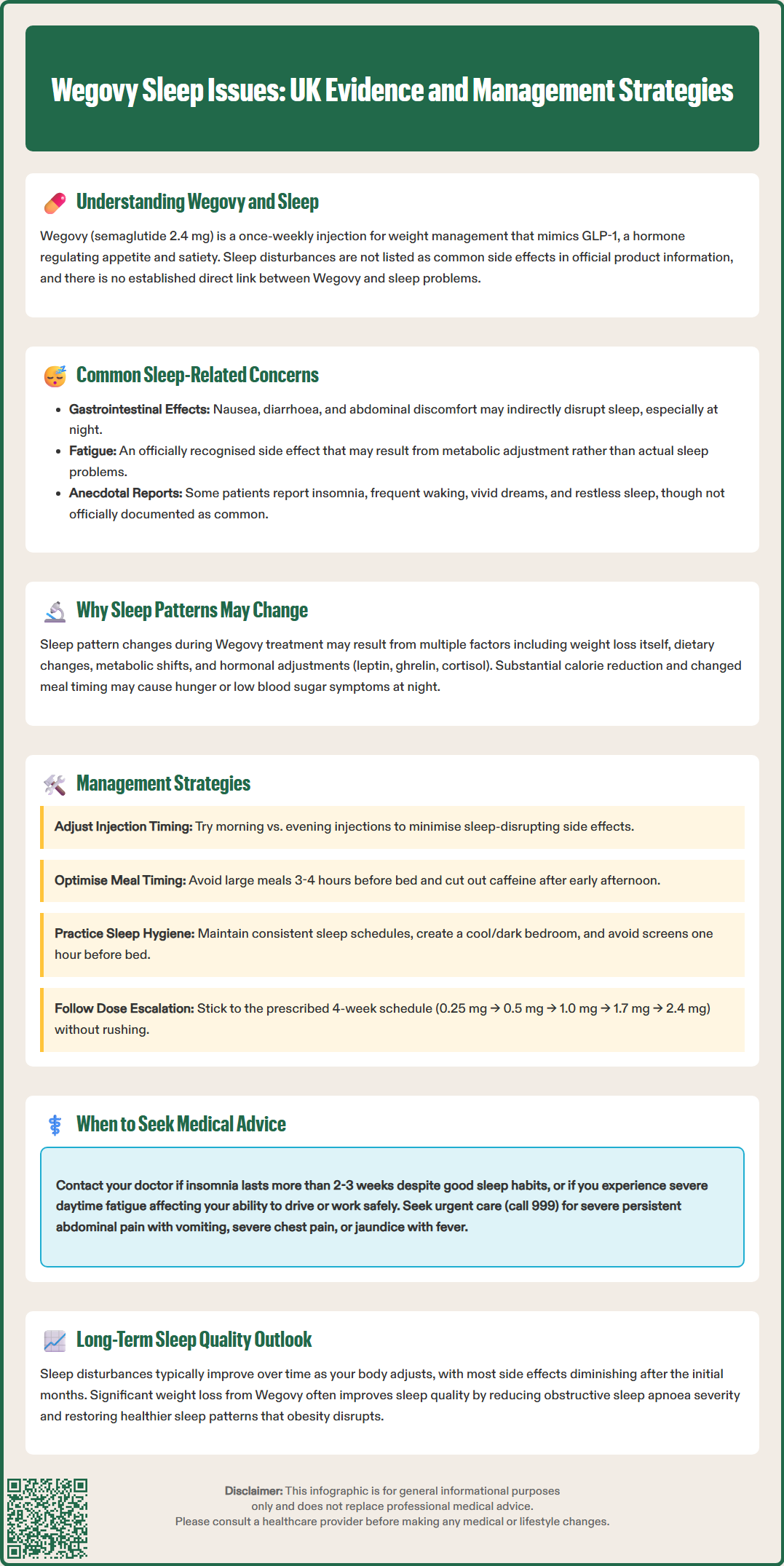
Wegovy sleep issues have been reported anecdotally by some patients, though sleep disturbances are not listed amongst the common side effects in the official UK product information. Wegovy (semaglutide 2.4 mg) is a GLP-1 receptor agonist licensed by the MHRA for weight management in adults with obesity or overweight with weight-related comorbidities. Whilst gastrointestinal effects such as nausea and fatigue are well-documented, the relationship between Wegovy and sleep quality remains an area requiring further research. This article examines current evidence, explores potential mechanisms, and provides practical guidance for managing sleep-related concerns during treatment.
Quick Answer: Sleep disturbances are not listed as common side effects of Wegovy in UK product information, though some patients report sleep-related concerns that may relate to gastrointestinal effects, metabolic changes, or dietary adjustments rather than direct drug effects.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA for weight management in adults with obesity or overweight with weight-related comorbidities. It is indicated as an adjunct to a reduced-calorie diet and increased physical activity. Administered as a once-weekly subcutaneous injection, Wegovy works by mimicking the natural hormone GLP-1, which regulates appetite and food intake through actions on the brain's satiety centres.
Whilst Wegovy has demonstrated significant efficacy in clinical trials for weight reduction, patients and healthcare professionals have reported various side effects during treatment. Sleep disturbances are not listed amongst the common or very common side effects in the Summary of Product Characteristics (SmPC), though some patients have reported sleep-related concerns anecdotally. It is important to understand that there is no officially established direct link between Wegovy and sleep problems in the licensed product information.
The relationship between GLP-1 receptor agonists and sleep quality remains an area requiring further research. Sleep patterns can be influenced by numerous factors, including weight loss itself, dietary changes, metabolic shifts, and the adjustment period when starting new medications. Understanding the potential mechanisms and distinguishing between direct drug effects and indirect consequences of treatment is essential for both patients and clinicians.
This article examines the current evidence regarding sleep issues in patients taking Wegovy, explores possible mechanisms, and provides practical guidance for managing any sleep-related concerns during treatment. Patients experiencing persistent or concerning sleep disturbances should always consult their prescribing healthcare professional for individualised advice. In the UK, Wegovy is typically prescribed within specialist weight management services, as recommended by NICE Technology Appraisal 875.
According to the official MHRA/EMC Summary of Product Characteristics, the most frequently reported adverse effects of Wegovy are gastrointestinal in nature, including:
Nausea (very common, affecting more than 1 in 10 people)
Diarrhoea (very common)
Vomiting (common, affecting up to 1 in 10 people)
Constipation (common)
Abdominal pain (common)
Fatigue is also listed as a common side effect in the SmPC. Sleep disturbances such as insomnia are not listed amongst the common or very common side effects. However, post-marketing surveillance and patient reports have identified sleep-related concerns in some individuals, including:
Difficulty falling asleep (insomnia)
Frequent night-time waking
Vivid dreams or nightmares
Daytime fatigue despite adequate sleep duration
Restless sleep patterns
It is crucial to note that these reports do not establish causation. The gastrointestinal side effects of Wegovy, particularly nausea and abdominal discomfort, may themselves disrupt sleep quality, especially if symptoms worsen during the night. Additionally, the significant dietary changes and caloric restriction that often accompany Wegovy treatment can independently affect sleep architecture.
Fatigue, as noted in the SmPC, may be misinterpreted as a sleep problem when it actually reflects the body's metabolic adjustment to treatment and weight loss. Patients should maintain a symptom diary to help distinguish between true sleep disturbances and other treatment-related effects that might impact perceived sleep quality. This information proves valuable when discussing concerns with healthcare professionals.
If you experience any suspected adverse reactions to Wegovy, you can report them via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Several potential mechanisms might explain why some patients experience sleep changes whilst taking Wegovy, though robust clinical evidence remains limited:
Metabolic and hormonal changes: GLP-1 receptor agonists influence multiple metabolic pathways beyond appetite regulation. Weight loss itself triggers hormonal adaptations, including changes in leptin, ghrelin, and cortisol levels, all of which play roles in sleep-wake regulation. The body's adjustment to a new metabolic state during significant weight reduction may temporarily disrupt established sleep patterns.
Gastrointestinal effects: The pronounced gastrointestinal side effects of Wegovy, particularly nausea and reflux symptoms, can directly interfere with sleep quality. Delayed gastric emptying—a therapeutic mechanism of semaglutide documented in the SmPC—may cause nocturnal discomfort if meals are consumed too close to bedtime.
Dietary changes and timing: Patients taking Wegovy typically reduce their caloric intake substantially. Going to bed hungry or making significant changes to meal timing can affect sleep quality. Some individuals may experience symptoms that feel like low blood sugar at night, particularly if they have reduced food intake dramatically. True hypoglycaemia is uncommon with semaglutide alone but is a risk when combined with insulin or sulfonylureas in patients with diabetes.
Central nervous system effects: Whilst GLP-1 receptors are found throughout the brain, including areas involved in sleep regulation, the clinical significance of this distribution for sleep quality remains unclear. There is no official evidence that Wegovy directly alters sleep architecture through central mechanisms, and human data on this topic are limited.
Understanding these potential mechanisms helps patients and clinicians develop targeted strategies to minimise sleep disruption during treatment. If you have diabetes and take insulin or sulfonylureas alongside Wegovy, discuss with your prescriber whether dose adjustments are needed to prevent nocturnal hypoglycaemia.
If you experience sleep difficulties whilst taking Wegovy, several evidence-based strategies may help improve sleep quality:
Optimise injection timing: Although Wegovy can be administered at any time of day, some patients find that adjusting injection timing helps minimise side effects that might disrupt sleep. Experiment with morning versus evening administration to identify what works best for your individual response. According to the SmPC, Wegovy should be administered on the same day each week; if changing the day, ensure at least 72 hours have passed since the last dose.
Dietary modifications:
Avoid large meals within 3–4 hours of bedtime to reduce nocturnal gastrointestinal discomfort
Ensure adequate hydration throughout the day, but limit fluids close to bedtime
Consider small, protein-rich snacks if hunger disrupts sleep, whilst staying within your caloric goals
Avoid caffeine after early afternoon and limit alcohol consumption
Sleep hygiene practices:
Maintain consistent sleep and wake times, even on weekends
Create a cool, dark, quiet sleeping environment
Establish a relaxing pre-sleep routine (reading, gentle stretching, meditation)
Limit screen exposure for at least one hour before bed
Engage in regular physical activity, but not within 3 hours of bedtime
Manage gastrointestinal symptoms: Work with your healthcare provider to optimise management of nausea and other GI effects. If anti-emetic medications are considered, discuss options with your prescriber or pharmacist rather than self-medicating, as some medications may have interactions. Elevating the head of your bed may help if reflux symptoms worsen at night.
Gradual dose escalation: Wegovy treatment follows a specific dose-escalation schedule designed to improve tolerability: 0.25 mg → 0.5 mg → 1.0 mg → 1.7 mg → 2.4 mg, with each dose maintained for 4 weeks. Do not rush this process; allow your body adequate time to adjust at each dose level before progressing. If sleep disturbances are severe, discuss with your prescriber whether temporarily remaining at a lower dose (such as 1.7 mg) might be appropriate.
Whilst mild, temporary sleep changes may occur as your body adjusts to Wegovy, certain situations warrant prompt medical consultation:
Contact your GP or prescribing clinician if you experience:
Persistent insomnia lasting more than 2–3 weeks despite implementing sleep hygiene measures
Severe daytime fatigue that impairs your ability to function safely (particularly if driving or operating machinery)
Sleep disturbances accompanied by mood changes, including low mood, anxiety, or irritability
Symptoms suggesting sleep apnoea (loud snoring, witnessed breathing pauses, morning headaches, excessive daytime sleepiness)
Neck swelling, difficulty swallowing, or persistent hoarseness (thyroid symptoms requiring assessment)
Right upper abdominal pain, especially after eating (possible gallbladder issues, which are associated with GLP-1 receptor agonists)
Seek urgent medical attention (call 999 or go to A&E) if:
You experience severe, persistent abdominal pain, especially if radiating to the back and accompanied by vomiting (possible pancreatitis)
You develop severe chest pain
You have signs of jaundice (yellowing of the skin/eyes) with fever and abdominal pain (possible acute gallbladder disease)
Your healthcare provider can assess whether sleep disturbances are related to Wegovy, another underlying condition, or the weight loss process itself. They may recommend:
Temporary dose adjustment or treatment pause
Additional investigations to rule out other causes (thyroid function tests, sleep studies if sleep apnoea suspected)
Referral to a sleep specialist for persistent, unexplained sleep disorders
Alternative weight management strategies if side effects prove intolerable
Do not stop Wegovy without discussing with your prescriber. Your healthcare professional can help you make informed decisions about continuing, adjusting, or stopping treatment based on a comprehensive assessment of benefits versus side effects.
For most patients, any sleep disturbances experienced when starting Wegovy tend to improve over time as the body adjusts to treatment. Clinical trial data from the STEP programme (particularly STEP 1 and STEP 4) extending beyond one year show that tolerability generally improves after the initial months, with many side effects diminishing in frequency and severity.
Weight loss and sleep benefits: Importantly, the substantial weight reduction achieved with Wegovy may ultimately improve sleep quality for many patients. Obesity is strongly associated with obstructive sleep apnoea (OSA), and weight loss represents a cornerstone of OSA management according to NICE guidance. Studies have demonstrated that significant weight reduction can reduce OSA severity, decrease the need for continuous positive airway pressure (CPAP) therapy, and improve overall sleep architecture.
Patients with obesity often experience:
Reduced sleep efficiency
Increased sleep fragmentation
Lower proportions of restorative deep sleep
Greater daytime sleepiness
As weight decreases during Wegovy treatment, these parameters frequently improve, potentially offsetting any initial medication-related sleep disruption. The metabolic improvements accompanying weight loss—including better glycaemic control, reduced inflammation, and improved cardiovascular function—may also contribute to enhanced sleep quality over time.
Monitoring and adjustment: Long-term success with Wegovy requires ongoing communication with your healthcare team. Regular follow-up appointments provide opportunities to discuss sleep quality alongside other treatment outcomes. According to NICE TA875, Wegovy is typically prescribed for up to 2 years within specialist weight management services in the UK. If sleep problems persist beyond the initial adjustment period (typically 3–6 months), your clinician may recommend:
Comprehensive sleep assessment
Review of concomitant medications that might affect sleep
Evaluation for mood disorders, which can both cause and result from poor sleep
Consideration of whether treatment benefits outweigh persistent side effects
Maintaining realistic expectations about the treatment journey, including the possibility of temporary side effects, helps patients persist with therapy long enough to achieve meaningful health benefits.
Sleep disturbances are not listed as common side effects in the UK Summary of Product Characteristics for Wegovy. Some patients report sleep-related concerns anecdotally, but these may relate to gastrointestinal effects, dietary changes, or metabolic adjustments during weight loss rather than direct drug effects on sleep.
Optimise injection timing, avoid large meals within 3–4 hours of bedtime, maintain consistent sleep hygiene practices, manage gastrointestinal symptoms with your healthcare provider, and follow the gradual dose-escalation schedule. If sleep disturbances persist beyond 2–3 weeks, consult your prescribing clinician.
Contact your GP or prescribing clinician if you experience persistent insomnia lasting more than 2–3 weeks, severe daytime fatigue impairing function, sleep disturbances with mood changes, or symptoms suggesting sleep apnoea. Do not stop Wegovy without discussing with your prescriber.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.