
What are Ozempic eyes? This term describes cosmetic changes around the orbital area—such as hollowing, increased eyelid creases, and a sunken appearance—that some people notice during semaglutide (Ozempic) treatment. 'Ozempic eyes' is not a recognised medical condition or official adverse effect listed by the MHRA or EMA. These aesthetic changes typically result from significant weight loss rather than direct drug effects on ocular tissues. Semaglutide is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes mellitus, and its appetite-suppressing properties can lead to facial fat reduction, creating a hollowed periorbital appearance.
Quick Answer: 'Ozempic eyes' refers to cosmetic periorbital changes—such as hollowing and increased eyelid creases—resulting from weight loss during semaglutide treatment, not a direct drug effect on eye tissues.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereThe term 'Ozempic eyes' has emerged in popular discourse to describe perceived changes in facial appearance—particularly around the eyes—that some individuals attribute to treatment with semaglutide (Ozempic). This phenomenon is not a recognised medical condition or an official adverse effect listed in the Summary of Product Characteristics (SmPC) from the MHRA or EMA. Rather, it refers to cosmetic changes including hollowing around the orbital area, increased visibility of eyelid creases, and a sunken or aged appearance of the periorbital region.
These changes are generally understood to result from significant weight loss rather than a direct pharmacological effect of semaglutide on ocular tissues. Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus, while Wegovy (also semaglutide, at higher doses) is licensed for weight management. Semaglutide works by enhancing insulin secretion, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways. Consequently, many patients experience weight reduction during treatment.
When rapid or significant fat loss occurs, subcutaneous facial fat—including the delicate fat pads around the eyes—may diminish. This loss of volume can create a hollowed, tired, or prematurely aged appearance. It is important to distinguish these cosmetic concerns from genuine ophthalmic complications. Whilst 'Ozempic eyes' reflects aesthetic changes likely secondary to weight loss, there are separate, clinically significant eye-related adverse effects associated with semaglutide that require medical attention, particularly in individuals with pre-existing diabetic retinopathy, as noted in the Ozempic SmPC.
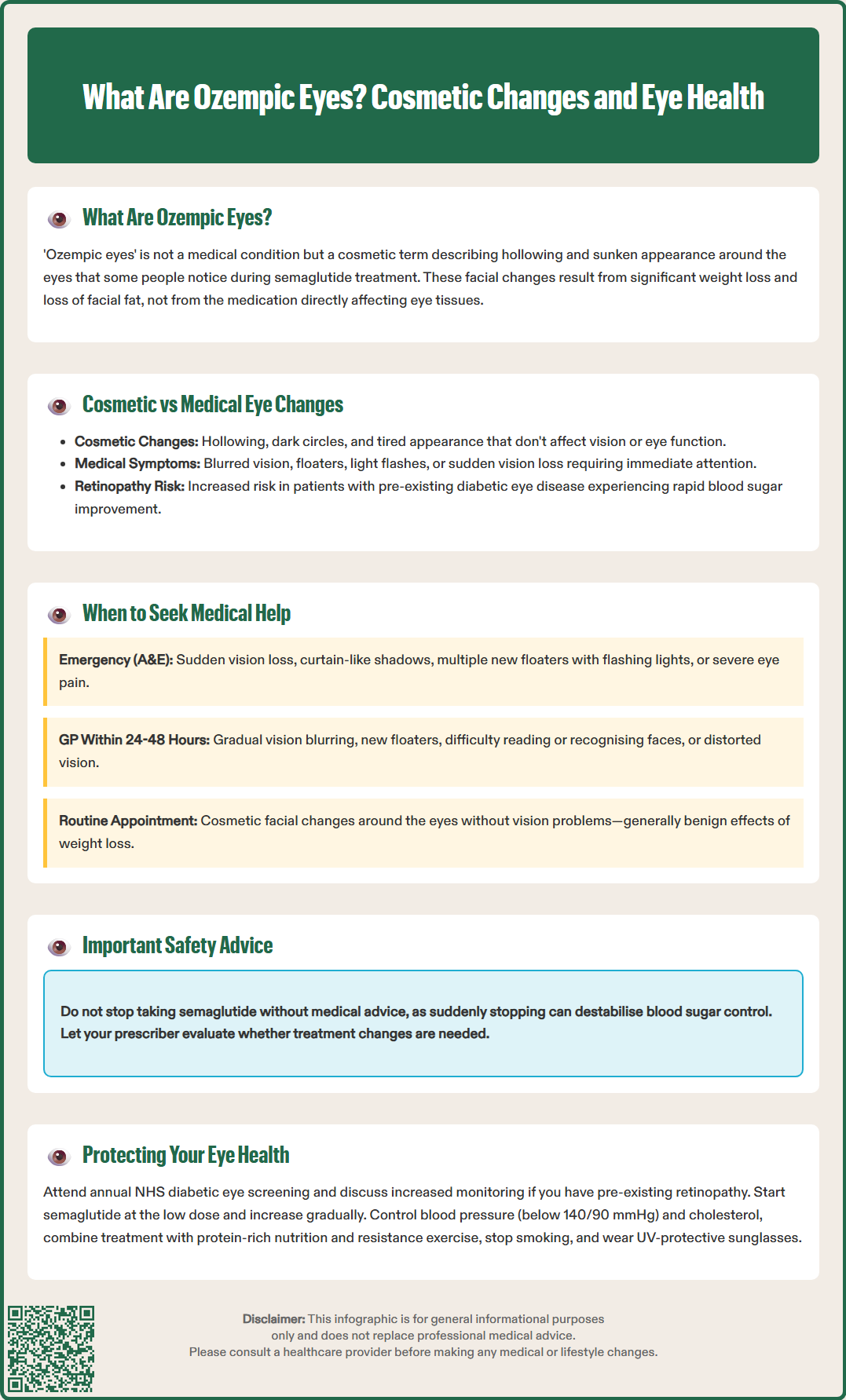
Understanding the distinction between cosmetic changes and medically significant ocular symptoms is essential for patient safety. Cosmetic periorbital changes attributed to weight loss may include:
Hollowing or sunken appearance around the eyes
Increased prominence of eyelid folds and fine lines
Dark circles or shadowing beneath the eyes
A generally tired or aged facial appearance
These aesthetic alterations do not typically affect vision or eye function and are not listed as adverse drug reactions in the SmPC. They reflect volume loss in facial fat compartments and are comparable to changes seen with weight loss from any cause. If you suspect these or any other side effects, you can report them via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
In contrast, clinically significant eye symptoms that warrant medical evaluation include:
Blurred vision or difficulty focusing
Floaters (spots or cobwebs drifting across the visual field)
Flashes of light in peripheral vision
Sudden vision loss or dark areas in the visual field
Eye pain or persistent discomfort
Distorted vision (straight lines appearing wavy)
These symptoms may indicate diabetic retinopathy progression, retinal detachment, or other serious ophthalmic conditions. Clinical trial data (SUSTAIN-6) and post-marketing surveillance have identified an increased risk of diabetic retinopathy complications in patients with pre-existing retinopathy who experience rapid glycaemic improvement on semaglutide. The MHRA's SmPC for Ozempic specifically notes this association, particularly in patients with a history of diabetic eye disease.
Patients should be aware that whilst facial volume changes are generally benign, any alteration in vision quality, visual field, or eye comfort requires prompt professional assessment. Early detection of retinopathy progression significantly improves treatment outcomes and helps preserve vision.
If you develop any visual symptoms whilst taking semaglutide, prompt action is essential to protect your eyesight. The following steps provide guidance on appropriate responses:
Immediate medical attention (same day via A&E, eye casualty, or urgent optometry service) is required for:
Sudden vision loss or significant deterioration
Curtain-like shadow across the visual field
Sudden onset of multiple floaters or flashing lights
Severe eye pain
These symptoms may indicate retinal detachment or other sight-threatening emergencies requiring urgent ophthalmological intervention. Do not drive if you experience these symptoms until you have been assessed.
Contact your GP or diabetes specialist within 24–48 hours for:
Gradual blurring of vision
New or increasing floaters (without sudden onset or visual field changes)
Difficulty reading or recognising faces
Distorted or wavy vision
Any persistent visual disturbance
Your healthcare provider will assess whether urgent ophthalmology referral is needed. You can also contact NHS 111 for advice. Do not discontinue Ozempic without medical advice, as abrupt cessation may destabilise glycaemic control. Your prescriber can evaluate the risk-benefit balance and determine whether treatment modification is appropriate.
For cosmetic periorbital changes without visual symptoms, discuss concerns at your next routine appointment. Whilst these changes do not require emergency intervention, your healthcare team can:
Assess your overall diabetes management and glycaemic control
Provide reassurance about the benign nature of facial volume changes
Discuss strategies to support gradual, sustainable weight reduction
Cosmetic treatments for facial volume loss are not routinely provided on the NHS. If considering private options, ensure you consult a suitably qualified, regulated healthcare professional.
Maintain your scheduled diabetic eye screening appointments (annual retinal photography for people with diabetes in the UK). If you have known diabetic retinopathy, more frequent monitoring may be recommended when initiating or intensifying semaglutide therapy, particularly during the first year of treatment when glycaemic changes are most pronounced.
Proactive eye health management is crucial for patients receiving semaglutide, particularly those with diabetes. The following evidence-based strategies help minimise risks and maintain ocular wellbeing:
Optimise diabetic eye screening compliance. The NHS Diabetic Eye Screening Programme offers annual retinal photography to all people with diabetes aged 12 and over. This screening detects diabetic retinopathy before symptoms develop. Patients with pre-existing retinopathy should discuss monitoring schedules with their healthcare team when starting semaglutide, as NICE guidance (NG28) notes that rapid improvements in glycaemic control can temporarily worsen retinopathy.
Gradual glycaemic optimisation may reduce retinopathy progression risk. Whilst semaglutide's glucose-lowering effects are therapeutically beneficial, very rapid HbA1c reduction has been associated with temporary worsening of diabetic retinopathy. Treatment is typically initiated at 0.25 mg weekly (a starting dose not intended for glycaemic control), with gradual escalation according to the SmPC, allowing physiological adaptation. This approach balances glycaemic control with ocular safety.
Maintain optimal blood pressure and lipid control. Hypertension and dyslipidaemia independently contribute to diabetic retinopathy progression. Comprehensive cardiovascular risk management—including individualised blood pressure targets (generally <140/90 mmHg in adults under 80 per NICE NG136, with lower targets considered for those with kidney disease, albuminuria or eye/cerebrovascular disease) and statin therapy where indicated—supports both macrovascular and microvascular health.
Support gradual, sustainable weight loss. Whilst semaglutide effectively promotes weight reduction, extremely rapid loss may exacerbate facial volume depletion. Combining pharmacotherapy with:
Balanced nutrition emphasising protein intake to preserve lean mass
Regular resistance exercise to maintain muscle tone
Adequate hydration
Gradual dose escalation as per SmPC
...can help achieve therapeutic weight loss whilst minimising cosmetic concerns.
Address modifiable risk factors for eye disease, including smoking cessation (smoking significantly accelerates diabetic retinopathy) and UV protection through quality sunglasses.
Finally, maintain open communication with your healthcare team. Report any visual changes promptly, attend all screening appointments, and discuss concerns about treatment effects. With appropriate monitoring, most patients can use semaglutide safely whilst preserving their vision and overall eye health.
No, 'Ozempic eyes' is not listed as an adverse drug reaction in the MHRA or EMA Summary of Product Characteristics. The term describes cosmetic periorbital changes resulting from weight loss rather than a direct pharmacological effect of semaglutide on eye tissues.
Seek immediate medical attention for sudden vision loss, curtain-like shadows, multiple floaters with flashing lights, or severe eye pain. Contact your GP within 24–48 hours for gradual blurring, new floaters, or persistent visual disturbances, as these may indicate diabetic retinopathy progression.
Attend annual NHS Diabetic Eye Screening appointments, maintain optimal blood pressure and lipid control, support gradual weight loss through balanced nutrition and exercise, and report any visual changes promptly to your healthcare team. Patients with pre-existing retinopathy may require more frequent monitoring.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.