When you take a medicine, your body doesn't simply absorb it and then eliminate it unchanged. Instead, it undergoes metabolism—a complex chemical transformation that breaks down the drug into different compounds. Understanding what 'metabolised' means is essential for grasping how medicines work, why doses vary between individuals, and how drug interactions occur. Metabolism primarily happens in the liver through specialised enzymes, affecting how long a medicine stays active in your system and how effectively it works. This natural process explains why the same medication can affect different people differently, and why healthcare professionals carefully consider individual factors when prescribing treatment.
Quick Answer: Metabolism is the chemical process by which your body breaks down and transforms medicines into different compounds that can be used or eliminated.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMetabolism is the process by which your body chemically transforms substances—including foods, drinks, and medicines—into forms that can be used for energy or eliminated from the body. When we say a drug is "metabolised," we mean your body is breaking it down and changing its chemical structure.
Think of metabolism as your body's internal recycling and waste management system. When you take a tablet or receive an injection, the active ingredient enters your bloodstream and travels to where it's needed. Your body begins processing the medicine, often while it's still having its therapeutic effect. This processing—metabolism—converts the drug into different chemical compounds called metabolites.
Some metabolites are inactive, meaning they no longer have a therapeutic effect and are simply waste products ready for elimination. However, other metabolites can be active and may contribute to the drug's overall effect, or occasionally cause side effects. In certain cases, a medicine you take is actually an inactive "prodrug" (such as enalapril or codeine) that only becomes effective after your body metabolises it into its active form.
Understanding metabolism is important because it affects how long a medicine stays in your system, how strong its effects are, and how often you need to take it. The speed and efficiency of metabolism vary from person to person, which is why the same dose of a medicine can affect different people in different ways. This natural variation is one reason why healthcare professionals carefully consider individual factors when prescribing medications.
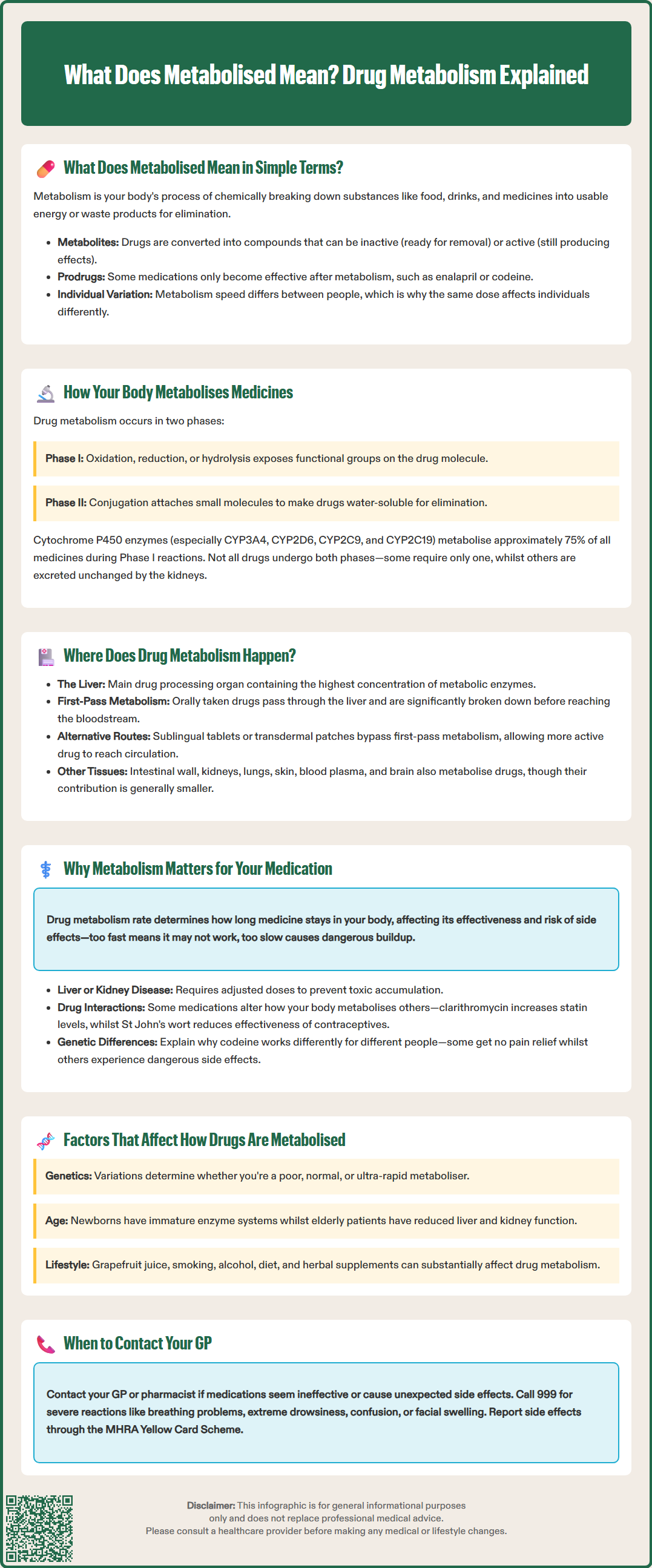
Drug metabolism occurs through two main types of chemical reactions, known as Phase I and Phase II metabolism. These processes work together to make medicines more water-soluble, which allows them to be excreted through urine or bile.
Phase I reactions typically involve oxidation, reduction, or hydrolysis—chemical processes that add or expose functional groups on the drug molecule. The most important enzymes involved in Phase I metabolism belong to the cytochrome P450 (CYP450) family. These enzymes, particularly CYP3A4, CYP2D6, CYP2C9, and CYP2C19, are responsible for metabolising approximately 75% of all medicines. During Phase I, drugs may become more active, less active, or remain similarly active, but they're generally prepared for the next stage of processing.
Phase II reactions involve conjugation, where the body attaches small molecules (such as glucuronic acid, sulphate, or glutathione) to the drug or its Phase I metabolite. This process typically produces inactive, highly water-soluble compounds that are easily eliminated. Common Phase II enzymes include UDP-glucuronosyltransferases (UGTs) and sulphotransferases.
Not all drugs undergo both phases—some may only require Phase I or Phase II metabolism, whilst others bypass liver metabolism entirely and are excreted unchanged by the kidneys. The specific metabolic pathway depends on the drug's chemical structure and properties. Some medicines are designed to be "modified-release" or "extended-release" formulations, which alter the rate of drug release and absorption rather than the metabolic process itself. This creates a more stable concentration in the bloodstream, often allowing for once-daily dosing rather than multiple doses throughout the day.
The liver is the primary site of drug metabolism, functioning as the body's main chemical processing plant. This large organ contains the highest concentrations of metabolic enzymes, particularly the CYP450 system, making it responsible for metabolising the majority of medicines. Blood from the digestive system passes through the liver via the hepatic portal vein, meaning that drugs taken orally encounter liver enzymes before reaching the general circulation—a phenomenon called first-pass metabolism.
First-pass metabolism can significantly reduce the amount of active drug that reaches your bloodstream. For some medicines, such as glyceryl trinitrate (used for angina), first-pass metabolism is so extensive that oral administration would be ineffective, which is why these drugs are given via alternative routes like sublingual tablets or transdermal patches that bypass the liver initially.
Whilst the liver is the primary metabolic organ, drug metabolism also occurs in other tissues throughout the body, though generally to a lesser extent. The intestinal wall contains CYP450 enzymes, particularly CYP3A4, which begin metabolising some drugs even before they're absorbed, contributing to first-pass effects. The kidneys metabolise certain drugs and are crucial for eliminating water-soluble metabolites through urine. Other sites include the lungs (important for inhaled medications), skin, blood plasma, and even the brain, though their contribution is typically minor compared to the liver.
The gut microbiome—the trillions of bacteria living in your intestines—also plays a role in drug metabolism. These microorganisms can chemically modify certain medicines before or after absorption, potentially affecting their efficacy and side effects. For example, some gut bacteria can inactivate digoxin, a heart medication. This is an emerging area of research that may explain some individual variations in drug response.
Understanding drug metabolism is crucial for safe and effective treatment. The rate at which your body metabolises a medicine directly affects its duration of action, therapeutic effect, and potential for side effects.
If a drug is metabolised too quickly, it may not remain in your system long enough to be effective, potentially requiring higher doses or more frequent administration. Conversely, if metabolism is too slow, the drug can accumulate in your body, increasing the risk of adverse effects or toxicity. This is why people with liver disease often require adjusted doses—their reduced metabolic capacity means standard doses could build up to dangerous levels. Similarly, in kidney impairment, reduced elimination of drugs and metabolites can lead to accumulation, even when metabolism itself is normal.
Drug interactions frequently occur at the metabolic level. Some medicines can inhibit (slow down) or induce (speed up) the enzymes that metabolise other drugs. For example, the antibiotic clarithromycin inhibits CYP3A4, which can increase blood levels of statins like simvastatin, raising the risk of muscle damage. The BNF advises avoiding simvastatin during clarithromycin treatment and using reduced doses of atorvastatin. Conversely, the herbal remedy St John's wort induces several CYP450 enzymes, potentially reducing the effectiveness of hormonal contraceptives, anticoagulants like warfarin, and other critical medications.
Metabolism also explains why some people experience prodrug activation differently. Codeine, for instance, must be metabolised by CYP2D6 to morphine to provide pain relief. People who are "poor metabolisers" due to genetic variations in CYP2D6 may get little benefit from codeine, whilst "ultra-rapid metabolisers" may experience excessive effects and side effects from standard doses. The MHRA has issued specific guidance restricting codeine use in children due to these metabolic variations, and NICE guidance suggests considering alternative analgesics in certain populations.
If you experience unexpected side effects or reduced medication effectiveness, contact your GP or pharmacist. For severe reactions such as breathing difficulties, severe drowsiness, confusion, or facial swelling, call 999 or go to A&E immediately. For urgent advice, contact NHS 111.
Multiple factors influence how efficiently your body metabolises medicines, contributing to the significant variation in drug response between individuals.
Genetic factors play a substantial role through pharmacogenomics—the study of how genes affect drug response. Variations in genes encoding metabolic enzymes can make someone a poor, intermediate, normal, or ultra-rapid metaboliser. For example, approximately 5-10% of people of European ancestry are poor CYP2D6 metabolisers, whilst certain populations have higher rates of ultra-rapid metabolism. In the UK, genetic testing is used for specific drugs where metabolism significantly affects safety or efficacy, such as testing for DPD deficiency before fluoropyrimidine chemotherapy (fluorouracil, capecitabine) and HLA-B*57:01 screening before abacavir treatment.
Age significantly impacts metabolism. Newborns and infants have immature enzyme systems, requiring careful dose adjustments. Elderly patients often experience reduced liver blood flow and enzyme activity, alongside decreased kidney function, meaning they typically require lower doses and are more susceptible to drug accumulation and interactions.
Liver and kidney function are critical. Conditions such as cirrhosis, hepatitis, or fatty liver disease impair metabolic capacity, whilst chronic kidney disease affects drug elimination. Healthcare professionals routinely assess liver and kidney function through blood tests before prescribing certain medications and may adjust doses accordingly.
Other factors include:
Sex: Hormonal differences can affect enzyme activity, and differences in body composition (including water content) can affect drug distribution and concentration
Diet and nutrition: Grapefruit juice famously inhibits CYP3A4; some vegetables may modestly affect certain enzymes; malnutrition impairs metabolic capacity
Smoking: Induces CYP1A2, affecting drugs like theophylline and clozapine, requiring dose adjustments when smoking status changes
Alcohol consumption: Chronic use induces some enzymes but acute intoxication inhibits metabolism
Concurrent medications and herbal supplements: As discussed, these can significantly inhibit or induce metabolic enzymes
Disease states: Infections, inflammation, and chronic conditions can alter enzyme expression
When to contact your GP: If you experience unexpected side effects, reduced medication effectiveness, or are starting new medicines (including over-the-counter products or herbal remedies), discuss potential metabolic interactions with your GP or pharmacist. If you have liver or kidney disease, ensure all healthcare providers are aware, as dose adjustments may be necessary. Never adjust your medication dose without professional guidance. Report suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Genetic variations in metabolic enzymes, age, liver and kidney function, concurrent medications, diet, smoking status, and underlying health conditions all influence how quickly and efficiently your body metabolises medicines. These factors explain why the same dose can affect different people differently.
First-pass metabolism occurs when orally administered drugs pass through the liver before reaching general circulation, where liver enzymes break down a portion of the drug. This can significantly reduce the amount of active medicine available, which is why some drugs are given via alternative routes like patches or sublingual tablets.
Yes, some medicines can inhibit or induce the enzymes responsible for drug metabolism, leading to potentially dangerous interactions. For example, clarithromycin can increase statin levels, whilst St John's wort can reduce the effectiveness of contraceptives and anticoagulants. Always inform your GP or pharmacist about all medications and supplements you're taking.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.