Many people wonder what to expect when starting Ozempic (semaglutide), a once-weekly injectable medication prescribed for type 2 diabetes in the UK. Most patients report feeling relatively normal initially, though noticeable changes typically emerge within hours to days. The most common early sensation is reduced hunger and feeling full more quickly during meals. Some experience mild nausea, particularly after eating, whilst the injection itself causes minimal discomfort. Physical effects vary considerably between individuals, with the gradual dose escalation protocol designed to minimise side effects and allow your body to adjust over time.
Quick Answer: Ozempic typically causes reduced hunger, earlier fullness when eating, and sometimes mild nausea, with effects varying between individuals.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
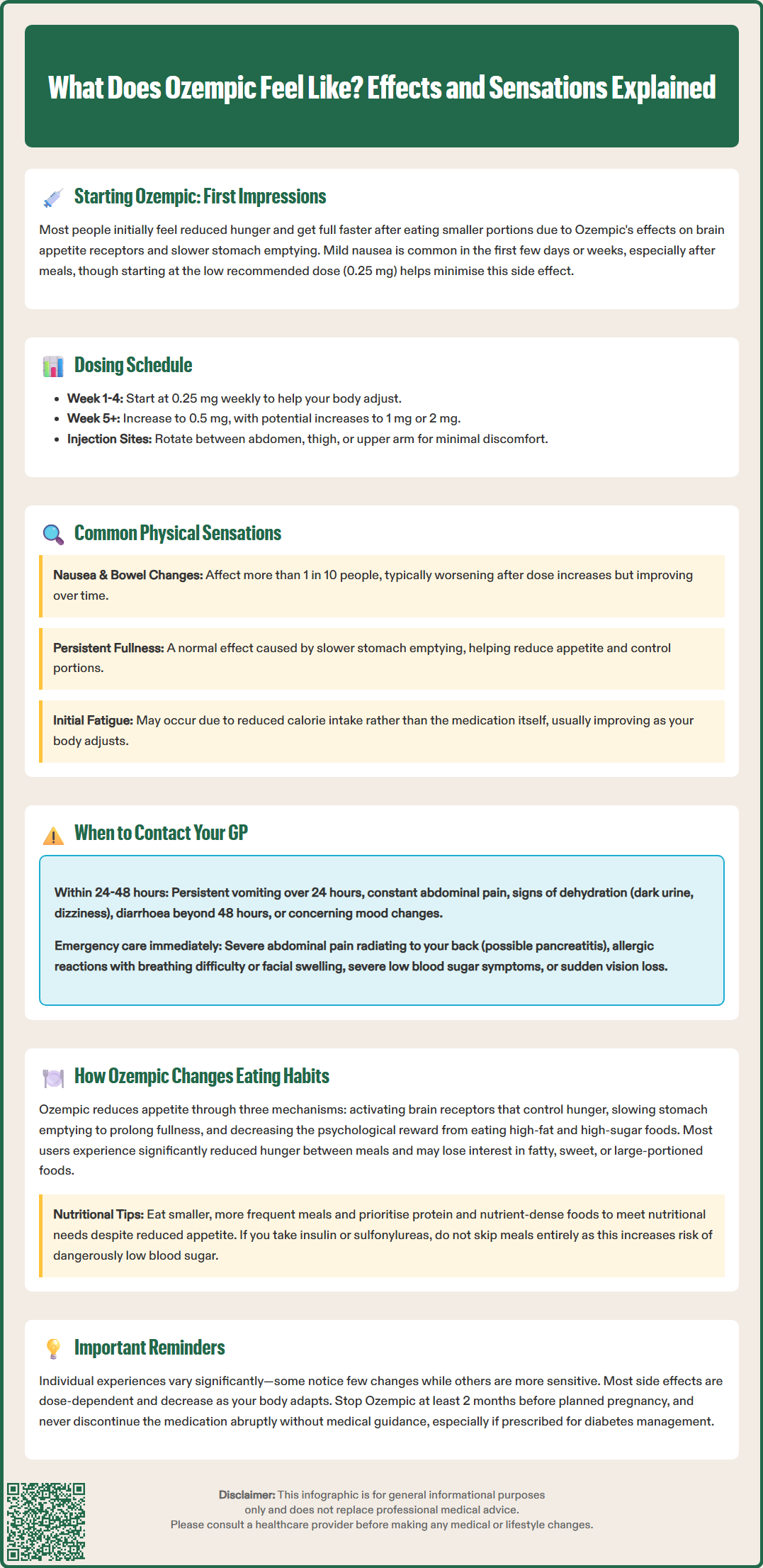
Start HereWhen you first begin taking Ozempic (semaglutide), many people report feeling relatively normal initially, though some physical sensations may emerge within hours to days of your first injection. Ozempic is a glucagon-like peptide-1 (GLP-1) receptor agonist administered once weekly via subcutaneous injection, prescribed for type 2 diabetes management in the UK.
The most commonly reported early sensation is a feeling of reduced hunger or earlier satiety when eating. This occurs because semaglutide acts on receptors in the brain that regulate appetite, whilst also slowing gastric emptying—the rate at which food leaves your stomach. Many patients describe feeling "comfortably full" after smaller portions than usual, which can feel unusual if you're accustomed to larger meals.
Some individuals experience mild nausea during the first few days or weeks, particularly after eating. This sensation typically ranges from slight queasiness to more noticeable discomfort, though severe nausea is less common when starting at the recommended low dose. As per the Ozempic SmPC, treatment begins with 0.25 mg once weekly for four weeks, then increases to 0.5 mg weekly, with further increases to 1 mg and potentially 2 mg at minimum 4-week intervals based on glycaemic response and tolerability.
The injection itself is generally well-tolerated, with most people reporting minimal discomfort at the injection site—similar to other subcutaneous injections. Injections should be administered in the abdomen, thigh, or upper arm, with rotation of injection sites recommended to reduce local reactions.
It's important to note that experiences vary considerably between individuals. Some people notice very few changes initially, whilst others may be more sensitive to the medication's effects. The gradual dose escalation protocol is specifically designed to minimise side effects and allow your body to adjust to the medication over time.
Beyond the initial adjustment period, several physical sensations and side effects are commonly associated with Ozempic treatment. Understanding these can help you distinguish between expected effects and symptoms requiring medical attention.
Gastrointestinal effects are the most frequently reported:
Nausea: Very common (affecting more than 1 in 10 people), usually most pronounced after dose increases and often improving over time
Altered bowel habits: Diarrhoea is very common, whilst constipation is common (affecting up to 1 in 10 people)
Bloating and abdominal discomfort: A sensation of fullness or mild cramping, particularly after meals
Indigestion or reflux: Slower gastric emptying can occasionally trigger acid reflux symptoms
Many patients describe a persistent feeling of fullness that extends well beyond mealtimes. This is a direct pharmacological effect of semaglutide's action on gastric motility and is often the mechanism through which appetite regulation occurs. Some people find this sensation helpful for portion control, whilst others may need time to adjust their eating patterns.
Fatigue or low energy is occasionally reported, particularly during the first few weeks or after dose escalations. This may relate to reduced caloric intake rather than a direct drug effect, though the distinction isn't always clear.
Less common but notable sensations include:
Mild headaches, typically transient
Dizziness, especially if blood glucose levels drop (hypoglycaemia risk is low with Ozempic alone but increases when used with insulin or sulfonylureas)
Changes in taste perception (uncommon)
Injection site reactions (redness, itching, or small lumps)
Important safety considerations include:
Gallbladder problems: Semaglutide has been associated with gallstones and inflammation of the gallbladder
Diabetic retinopathy complications: Particularly in those with pre-existing retinopathy, rapid improvement in glucose control may temporarily worsen eye problems
Dehydration risk: Prolonged vomiting or diarrhoea can lead to dehydration and potentially acute kidney injury
Most side effects are dose-dependent and tend to diminish as your body adapts to the medication. The gradual dose titration schedule exists specifically to improve tolerability whilst achieving therapeutic benefit.
Whilst many Ozempic-related sensations are expected and manageable, certain symptoms warrant prompt medical attention. Understanding when to contact your GP or seek urgent care is essential for safe medication use.
Contact your GP within 24–48 hours if you experience:
Persistent or severe nausea and vomiting that prevents you from keeping down fluids or food for more than 24 hours, as this increases dehydration risk
Abdominal pain, particularly if constant or uncomfortable—this requires assessment to exclude gallbladder problems or other causes
Signs of dehydration: dark urine, dizziness on standing, reduced urination, or extreme thirst
Persistent diarrhoea lasting more than 48 hours
Palpitations accompanied by chest pain, fainting, or sustained rapid heartbeat
Mood changes including persistent low mood, anxiety, or thoughts of self-harm (contact NHS 111 or your local mental health crisis team if urgent support is needed)
Seek immediate medical attention (A&E or call 999) if you develop:
Severe, unrelenting abdominal pain, especially if radiating to your back and accompanied by vomiting (possible pancreatitis)
Signs of an allergic reaction: difficulty breathing, facial swelling, or widespread rash
Symptoms of hypoglycaemia (if taking insulin or sulfonylureas): severe shakiness, confusion, loss of consciousness
Sudden vision loss, severe eye pain, or flashing lights/floaters
The Ozempic SmPC notes that acute pancreatitis has been reported as an uncommon side effect (affecting fewer than 1 in 100 people). Severe upper abdominal pain that doesn't resolve should always be evaluated urgently.
For thyroid-related symptoms such as a lump in your neck, persistent hoarseness, or difficulty swallowing, book a routine GP appointment unless you experience breathing difficulties, which would require emergency care.
If you have diabetes and pre-existing retinopathy, contact your GP or diabetes team promptly about any vision changes, as rapid improvement in blood glucose can sometimes temporarily worsen retinopathy.
For routine concerns about tolerability or questions about whether your symptoms are normal, schedule a non-urgent appointment with your GP or practice nurse. They can assess whether dose adjustment, symptomatic management, or medication review is appropriate.
If you're planning pregnancy, Ozempic should be discontinued at least 2 months before a planned conception as per the SmPC.
You can report any suspected side effects to the MHRA Yellow Card Scheme at yellowcard.mhra.gov.uk or via the Yellow Card app. Never stop Ozempic abruptly without medical guidance, particularly if prescribed for diabetes management.
One of the most profound and consistent effects people report with Ozempic is a fundamental change in appetite and relationship with food. Understanding the mechanism behind these changes can help you adapt your eating habits appropriately.
Semaglutide works through multiple pathways to influence appetite:
Central appetite regulation: It activates GLP-1 receptors in the hypothalamus and other brain regions that control hunger and satiety signals
Delayed gastric emptying: Food remains in your stomach longer, prolonging the feeling of fullness
Reduced food reward signalling: Research suggests GLP-1 agonists may diminish the psychological reward associated with eating, particularly high-fat or high-sugar foods
Most people describe a marked reduction in hunger between meals. The constant thoughts about food or frequent snacking urges that many experience—particularly those with obesity or insulin resistance—often diminish significantly. Many patients report that they simply "forget to eat" or need reminders for regular meals, which can feel quite unusual initially.
Changes in food preferences are anecdotally reported by some patients, though this effect has not been thoroughly studied in controlled trials. Some people find they lose interest in previously enjoyed foods, particularly:
Rich, fatty, or fried foods
Very sweet items
Large portion sizes
Alcohol (some report increased nausea with alcohol consumption)
Practical implications for eating habits:
To optimise nutrition whilst on Ozempic, consider:
Eating smaller, more frequent meals rather than forcing large portions
Prioritising protein and nutrient-dense foods to meet nutritional needs despite reduced intake
Eating slowly and stopping when comfortably satisfied, not full
Staying well-hydrated, as reduced food intake can decrease fluid consumption
Avoiding lying down immediately after eating to minimise reflux risk
If you have diabetes and take insulin or sulfonylureas, it's important not to skip meals entirely, as this could increase hypoglycaemia risk. Discuss with your diabetes team whether medication adjustments are needed if your eating patterns change significantly.
Some people find the appetite suppression helpful and liberating, whilst others may need time to adjust to eating primarily for nutrition rather than hunger cues. If you're struggling to maintain adequate nutrition or experiencing unintended excessive weight loss, discuss this with your GP or request referral to a dietitian. NICE guidance emphasises that GLP-1 receptor agonists should be part of a comprehensive approach including dietary advice and lifestyle modification, not a standalone intervention.
Most people notice reduced hunger and earlier fullness within hours to days of their first injection, though experiences vary. Mild nausea, if it occurs, typically emerges during the first few days or weeks of treatment.
The injection is generally well-tolerated, with most people reporting minimal discomfort similar to other subcutaneous injections. Rotating injection sites between the abdomen, thigh, or upper arm helps reduce local reactions.
Contact your GP within 24–48 hours for persistent vomiting, severe nausea preventing fluid intake, constant abdominal pain, or signs of dehydration. Seek immediate medical attention for severe unrelenting abdominal pain, difficulty breathing, facial swelling, or sudden vision loss.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.