Insulin resistance is a metabolic condition where the body's cells become less responsive to insulin, a hormone that regulates blood glucose levels. This reduced sensitivity forces the pancreas to produce more insulin to maintain normal blood sugar, potentially leading to prediabetes or type 2 diabetes. Often developing silently over many years, insulin resistance increases the risk of cardiovascular disease, non-alcoholic fatty liver disease, and metabolic syndrome. Understanding the symptoms and risk factors is crucial, as early lifestyle modifications can significantly reduce progression to serious complications. Many people in the UK remain unaware of their condition until routine screening or investigation of related health concerns.
Quick Answer: Insulin resistance is often asymptomatic, but key symptoms include acanthosis nigricans (dark, velvety skin patches), increased waist circumference, skin tags, fatigue, and difficulty losing weight.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereInsulin resistance is a metabolic condition in which the body's cells become less responsive to the hormone insulin, which is produced by the pancreas. Insulin plays a crucial role in regulating blood glucose (sugar) levels by facilitating the uptake of glucose from the bloodstream into cells, where it can be used for energy or stored for later use. When cells become resistant to insulin's effects, the pancreas compensates by producing more insulin to maintain normal blood glucose levels.
Over time, this compensatory mechanism can become insufficient, leading to elevated blood glucose levels and potentially progressing to prediabetes or type 2 diabetes mellitus. Insulin resistance is not a disease in itself but rather a physiological state that increases the risk of several serious health conditions, including cardiovascular disease, non-alcoholic fatty liver disease (NAFLD, also now known as metabolic dysfunction-associated steatotic liver disease or MASLD), polycystic ovary syndrome (PCOS), and metabolic syndrome.
The condition develops gradually, often over many years, and may be present long before any noticeable symptoms appear or blood glucose levels become abnormal. According to Diabetes UK, many people in the UK are at risk of insulin resistance and may be unaware of their condition. Understanding insulin resistance is important because early identification and lifestyle modifications can significantly reduce the risk of progression to type 2 diabetes and associated complications.
Insulin resistance affects multiple organ systems and is closely linked to obesity, particularly excess visceral (abdominal) fat, which releases inflammatory substances that interfere with insulin signalling pathways at the cellular level. However, it's important to note that insulin resistance can also occur in people with a healthy weight, particularly in certain ethnic groups.
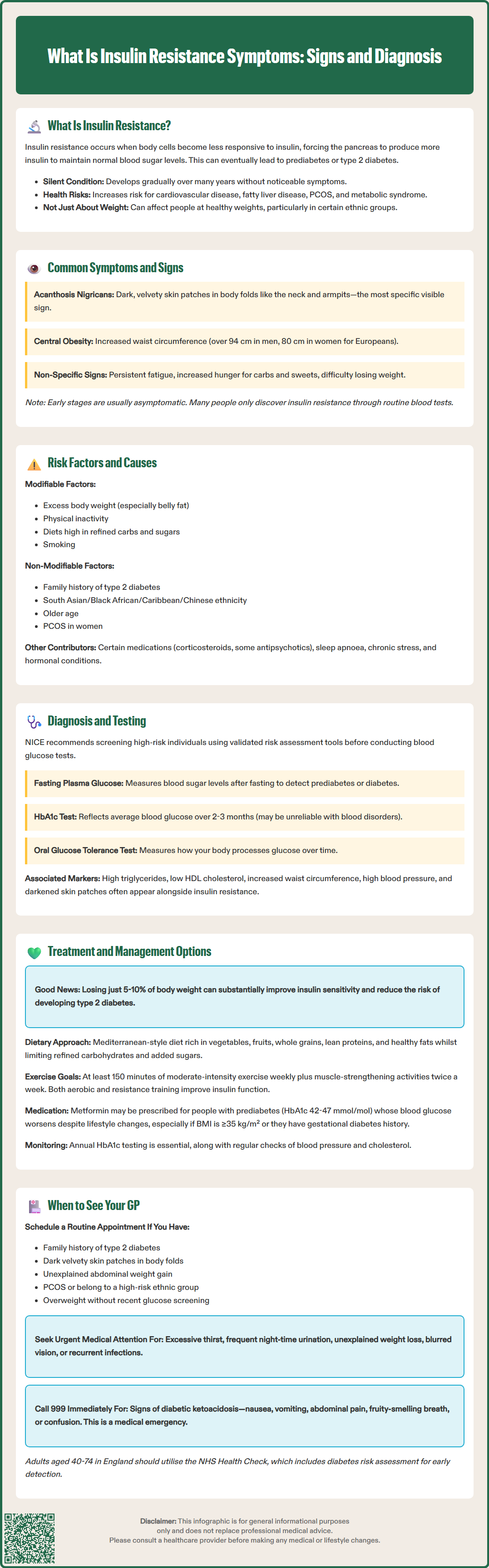
Insulin resistance is usually asymptomatic, with many individuals experiencing no obvious symptoms in the early stages. However, as the condition progresses, several signs may become apparent, though these can be subtle and easily overlooked.
Physical signs that may indicate insulin resistance include:
Acanthosis nigricans – dark, velvety patches of skin, typically appearing in body folds such as the neck, armpits, groin, or under the breasts. This is one of the most specific visible signs of insulin resistance and is recognised by Diabetes UK as a clinical marker.
Skin tags – small, soft growths of skin that commonly develop in areas where skin rubs together. While associated with insulin resistance, they are not specific to this condition.
Increased waist circumference – particularly central (abdominal) obesity, with fat accumulating around the midsection. For European populations, this is defined as >94 cm in men and >80 cm in women, with lower thresholds for South Asian populations (>90 cm for men, >80 cm for women).
Associations that may occur with insulin resistance include:
Fatigue – though this is non-specific and has many possible causes.
Increased hunger – especially for carbohydrates and sugary foods.
Difficulty losing weight – despite following a calorie-controlled diet and exercise programme.
It is important to note that these associations are non-specific and can occur in many other conditions. Additionally, insulin resistance itself does not cause the classic symptoms of diabetes (excessive thirst, frequent urination, unexplained weight loss) until blood glucose levels become significantly elevated. Many people only discover they have insulin resistance through routine blood tests or when investigating other health concerns.
Insulin resistance develops through a complex interplay of genetic, lifestyle, and environmental factors. Understanding these risk factors is essential for identifying individuals who may benefit from screening and preventive interventions.
Modifiable risk factors include:
Excess body weight and obesity – particularly visceral adiposity (fat stored around internal organs). Adipose tissue, especially when excessive, releases inflammatory cytokines and free fatty acids that interfere with insulin signalling.
Physical inactivity – sedentary behaviour reduces the muscles' glucose uptake capacity and contributes to weight gain.
Poor dietary habits – diets high in refined carbohydrates, added sugars, and saturated fats can promote insulin resistance.
Smoking – tobacco use is associated with increased insulin resistance and abdominal fat accumulation, as noted in NICE guidance on diabetes prevention.
Non-modifiable risk factors include:
Family history – having a first-degree relative with type 2 diabetes significantly increases risk.
Ethnicity – people of South Asian, Black African or Caribbean, and Chinese descent have higher susceptibility to insulin resistance at lower body weights, as reflected in UK risk assessment tools such as QDiabetes and the Leicester Practice Risk Score.
Age – risk increases with age; the NHS Health Check programme (offered to adults aged 40–74 in England) includes diabetes risk assessment.
Polycystic ovary syndrome (PCOS) – this hormonal condition is strongly associated with insulin resistance in women.
Other contributing factors include certain medications (such as corticosteroids, some antipsychotics, and protease inhibitors), sleep disorders (particularly obstructive sleep apnoea), chronic stress, and hormonal conditions such as Cushing's syndrome or hypothyroidism. Gestational diabetes during pregnancy also indicates increased risk of developing insulin resistance later in life. The NHS Diabetes Prevention Programme specifically targets individuals with multiple risk factors to prevent progression to type 2 diabetes.
Diagnosing insulin resistance can be challenging because there is no single, universally accepted diagnostic test used in routine clinical practice. However, several investigations can provide evidence of insulin resistance and assess associated metabolic abnormalities.
Blood tests commonly used include:
Fasting plasma glucose – measures blood sugar levels after an overnight fast. Normal is below 6.1 mmol/L; impaired fasting glucose (prediabetes) is 6.1–6.9 mmol/L; diabetes is ≥7.0 mmol/L, as defined by WHO and NICE guidance.
HbA1c (glycated haemoglobin) – reflects average blood glucose levels over the previous 2–3 months. Normal is below 42 mmol/mol; non-diabetic hyperglycaemia (NDH, also called prediabetes) is 42–47 mmol/mol; diabetes is ≥48 mmol/mol. HbA1c may be unreliable in certain conditions affecting red blood cells, such as haemoglobinopathies or anaemia.
Oral glucose tolerance test (OGTT) – measures glucose levels before and two hours after consuming a glucose drink. Normal is <7.8 mmol/L at 2 hours; impaired glucose tolerance is 7.8–11.0 mmol/L; diabetes is ≥11.1 mmol/L.
Fasting insulin levels – elevated fasting insulin suggests the pancreas is working harder to maintain normal glucose levels, though this test is not routinely performed in UK primary care.
Lipid profile – insulin resistance is often associated with elevated triglycerides and low HDL cholesterol.
NICE guidelines recommend screening for type 2 diabetes risk using validated tools such as the Leicester Practice Risk Score or Diabetes UK's 'Know Your Risk' tool. Individuals identified as high risk should undergo blood glucose testing.
Physical examination may reveal acanthosis nigricans, increased waist circumference (>94 cm in men, >80 cm in women of European descent; lower thresholds for South Asian populations), elevated blood pressure, or signs of PCOS.
More specialised tests, such as the hyperinsulinaemic-euglycaemic clamp (the gold standard for measuring insulin sensitivity) or HOMA-IR (Homeostatic Model Assessment of Insulin Resistance), are primarily used in research settings rather than routine clinical practice.
Managing insulin resistance focuses primarily on lifestyle modifications, which can significantly improve insulin sensitivity and reduce the risk of progression to type 2 diabetes. Pharmacological interventions may be considered in specific circumstances.
Lifestyle interventions form the cornerstone of treatment:
Weight loss – even modest weight reduction (5–10% of body weight) can substantially improve insulin sensitivity. The NHS Diabetes Prevention Programme offers structured support for individuals at high risk.
Dietary modifications – adopting a balanced diet rich in vegetables, fruits, whole grains, lean proteins, and healthy fats whilst limiting refined carbohydrates, added sugars, and saturated fats. The Mediterranean diet pattern has strong evidence for improving insulin sensitivity, as supported by the British Dietetic Association.
Regular physical activity – The UK Chief Medical Officers' Physical Activity Guidelines recommend at least 150 minutes of moderate-intensity aerobic activity per week, plus muscle-strengthening activities on two or more days. Both aerobic exercise and resistance training improve insulin sensitivity through different mechanisms.
Sleep optimisation – aiming for 7–9 hours of quality sleep per night, as sleep deprivation worsens insulin resistance.
Smoking cessation – NHS smoking cessation services can provide support for those looking to quit.
Pharmacological options may include:
Metformin – NICE guidance advises considering metformin for people with non-diabetic hyperglycaemia (HbA1c 42-47 mmol/mol) whose blood glucose is deteriorating despite lifestyle interventions. This is particularly relevant for those with a BMI ≥35 kg/m² (or ≥30 kg/m² in South Asian and other high-risk groups) or those with a history of gestational diabetes. It's important to note that metformin use for diabetes prevention is off-label in the UK and requires shared decision-making and monitoring of renal function.
Treatment of associated conditions – managing hypertension, dyslipidaemia, and PCOS can improve overall metabolic health.
Monitoring and follow-up are essential. Individuals with prediabetes should have annual HbA1c testing, and those with multiple risk factors may benefit from more frequent assessment. Regular review of cardiovascular risk factors, including blood pressure and lipid levels, is important as insulin resistance increases cardiovascular disease risk. Patient education about recognising symptoms of hyperglycaemia and the importance of adherence to lifestyle changes is crucial for long-term success.
Knowing when to seek medical advice is important for early detection and management of insulin resistance and prevention of complications.
You should arrange a routine GP appointment if you:
Have a family history of type 2 diabetes and are concerned about your own risk
Notice dark, velvety skin patches (acanthosis nigricans) developing in body folds
Are struggling with unexplained weight gain, particularly around your abdomen, despite efforts to maintain a healthy lifestyle
Have been diagnosed with PCOS, as insulin resistance is common in this condition
Belong to a high-risk ethnic group (South Asian, Black African or Caribbean, or Chinese descent) and have additional risk factors
Are overweight or obese and have not had recent blood glucose screening
Had gestational diabetes during pregnancy, as this increases future diabetes risk
Seek more urgent medical attention if you develop:
Symptoms of hyperglycaemia: excessive thirst, frequent urination (particularly at night), unexplained weight loss, blurred vision, or recurrent infections
Symptoms suggesting diabetic ketoacidosis (though rare with insulin resistance alone): nausea, vomiting, abdominal pain, fruity-smelling breath, or confusion. If you suspect DKA, call 999 or go to A&E immediately as this is a medical emergency.
Your GP can assess your diabetes risk using validated screening tools, arrange appropriate blood tests, and discuss personalised strategies for reducing your risk. They may refer you to specialist services such as the NHS Diabetes Prevention Programme if you have prediabetes, or to an endocrinologist if you have complex metabolic issues.
Regular health checks are advisable if you have multiple risk factors. The NHS Health Check, offered to adults aged 40–74 in England, includes diabetes risk assessment and is an excellent opportunity for early detection of insulin resistance and associated cardiovascular risk factors.
Yes, insulin resistance often develops years before blood glucose levels become elevated enough to diagnose prediabetes or type 2 diabetes. Many people have insulin resistance with completely normal blood glucose levels, though they remain at increased risk of progression to diabetes without lifestyle intervention.
Acanthosis nigricans appears as dark, velvety patches of thickened skin, typically in body folds such as the neck, armpits, groin, or under the breasts. It is one of the most specific visible clinical markers of insulin resistance and should prompt medical assessment.
Insulin sensitivity can begin to improve within weeks of starting regular physical activity and dietary modifications. Significant improvements are typically seen with 5–10% body weight reduction, which can substantially reduce the risk of progression to type 2 diabetes when sustained over time.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.