
Wegovy (semaglutide 2.4 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA for weight management in adults with obesity or overweight with weight-related comorbidities. Whilst clinical trials demonstrate significant efficacy, headaches are reported by approximately 14.8% of patients during treatment. Understanding why Wegovy causes headaches involves examining its effects on GLP-1 receptors in the central nervous system, metabolic changes associated with weight loss, and gastrointestinal effects that may influence hydration and nutrition. Most headaches are mild to moderate, occurring predominantly during dose escalation, and typically resolve as the body adapts to treatment.
Quick Answer: Wegovy causes headaches through GLP-1 receptor activation in the central nervous system, metabolic changes from weight loss, and gastrointestinal effects affecting hydration and nutrition.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWegovy (semaglutide 2.4 mg) is a prescription medicine licensed by the Medicines and Healthcare products Regulatory Agency (MHRA) for weight management in adults with obesity (BMI ≥30 kg/m²) or those who are overweight (BMI ≥27 kg/m²) with at least one weight-related health condition. It must be used as an adjunct to a reduced-calorie diet and increased physical activity. Wegovy belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which were originally developed for type 2 diabetes management but have demonstrated significant efficacy in promoting weight loss.
The medication works by mimicking the action of GLP-1, a naturally occurring hormone produced in the intestines after eating. Semaglutide binds to GLP-1 receptors throughout the body, including those in the brain, pancreas, and gastrointestinal tract. This binding triggers several physiological responses: it slows gastric emptying (the rate at which food leaves the stomach), reduces appetite by acting on brain regions that control hunger and satiety, and enhances insulin secretion whilst suppressing glucagon release when blood glucose levels are elevated.
Wegovy is administered as a once-weekly subcutaneous injection, typically starting at a low dose (0.25 mg) and gradually increasing over 16–20 weeks to the maintenance dose of 2.4 mg. This dose escalation schedule is designed to improve tolerability and reduce the likelihood of gastrointestinal side effects, which are among the most commonly reported adverse reactions.
Important contraindications include personal or family history of medullary thyroid carcinoma, Multiple Endocrine Neoplasia syndrome type 2, and previous serious hypersensitivity to semaglutide. It should also not be used in pregnancy or by patients with a history of pancreatitis.
The medication's effects on multiple body systems—including the central nervous system, digestive tract, and metabolic pathways—mean that patients may experience various side effects as their bodies adjust to treatment. Understanding how Wegovy works provides important context for why certain adverse effects, including headaches, may occur during therapy.
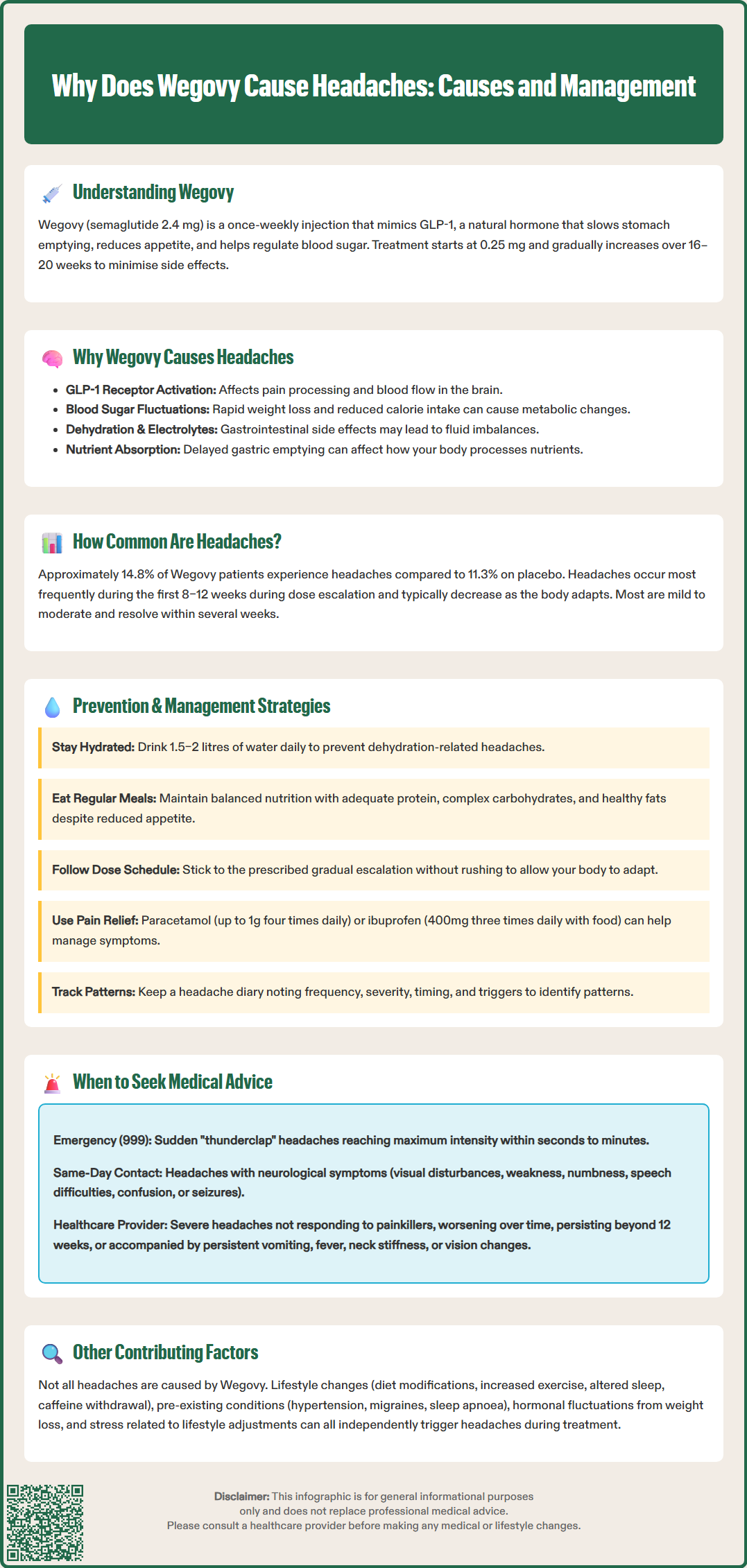
Headaches are a recognised adverse effect of Wegovy treatment, though the precise mechanisms underlying this side effect are not fully elucidated. Several hypothetical physiological pathways may contribute to headache development in patients taking semaglutide, though direct causal evidence in humans remains limited.
GLP-1 receptors are present in the central nervous system, including areas involved in pain processing and vascular regulation. When semaglutide activates these receptors, it may influence neurotransmitter release, cerebral blood flow, or neuronal excitability in ways that could potentially trigger headache symptoms in susceptible individuals. Some preclinical research suggests that GLP-1 receptor activation might affect the trigeminovascular system, which plays a central role in migraine pathophysiology, though there is no established causal link between Wegovy and migraines.
Metabolic changes associated with rapid weight loss and altered eating patterns may also contribute. As patients consume fewer calories and lose weight, fluctuations in blood glucose levels—even within the normal range—can precipitate headaches in some individuals. Additionally, changes in hydration status, electrolyte balance, and nutritional intake during the early phases of treatment may play a role.
Gastrointestinal effects of Wegovy, particularly nausea and reduced food intake, may indirectly contribute to headaches through dehydration or inadequate nutrition. The medication's effect on gastric emptying can also influence the absorption of other medications or nutrients that might affect headache susceptibility.
It is worth noting that headaches reported during Wegovy treatment are typically mild to moderate in intensity and often improve as the body adjusts to the medication. The dose escalation protocol is partly designed to minimise such adverse effects by allowing gradual physiological adaptation to the drug's effects.
According to the MHRA-approved Summary of Product Characteristics (SmPC), headaches are reported by approximately 14.8% of patients taking Wegovy, compared to around 11.3% in placebo groups. This indicates that whilst headaches do occur more frequently with semaglutide treatment, they are also relatively common in the general population and among individuals undergoing lifestyle modifications for weight loss.
Data from the pivotal STEP (Semaglutide Treatment Effect in People with obesity) clinical trials, which involved over 4,500 participants, showed that headache was among the ten most frequently reported adverse events. The incidence was highest during the dose escalation phase, particularly in the first 8–12 weeks of treatment, and tended to decrease over time as patients reached their maintenance dose and their bodies adapted to the medication.
Most headaches associated with Wegovy are classified as mild to moderate in severity. Severe headaches leading to treatment discontinuation are uncommon, occurring in fewer than 1% of trial participants. The majority of patients who experience headaches find that symptoms are manageable with standard over-the-counter analgesics and resolve spontaneously within several weeks.
Individual susceptibility varies considerably. Patients with a pre-existing history of headaches or migraines may be more likely to experience this side effect, though Wegovy does not appear to significantly worsen pre-existing headache disorders in most cases. Factors such as age, sex, baseline body mass index, and concurrent medications do not appear to substantially modify headache risk, though comprehensive data on all potential risk factors remain limited.
The clinical benefits of Wegovy for weight management—with average weight loss of 12–15% of body weight in clinical trials—should be weighed against potential adverse effects on an individual basis. Persistent or severe headaches warrant medical review to exclude other causes and optimise management.
Several practical strategies can help patients manage and potentially prevent headaches whilst taking Wegovy. These approaches focus on addressing the likely contributing factors and supporting the body's adjustment to treatment.
Hydration is paramount. Patients should aim to drink adequate fluids throughout the day—typically 1.5–2 litres of water daily, though individual needs vary based on activity levels, climate, and personal factors. Dehydration can both trigger headaches and exacerbate those caused by other factors. Keeping a water bottle accessible and setting regular reminders can help maintain consistent hydration.
Nutritional considerations are equally important. Despite reduced appetite, patients should ensure they consume:
Regular, balanced meals containing adequate protein, complex carbohydrates, and healthy fats
Sufficient calories to meet basic metabolic needs (consult with a healthcare professional or dietitian for personalised advice)
Electrolytes, particularly sodium and potassium, which can be depleted with reduced food intake
Avoiding prolonged fasting periods and maintaining relatively stable blood glucose levels may help reduce headache frequency.
Gradual dose escalation, as prescribed, allows the body to adapt progressively to Wegovy's effects. Patients should never skip dose levels or increase doses more rapidly than recommended, as this may increase the likelihood and severity of adverse effects, including headaches.
Standard headache management approaches remain effective:
Over-the-counter analgesics such as paracetamol (up to 1g four times daily) or ibuprofen (400mg three times daily with food) can provide relief. Patients should seek advice from their pharmacist or GP before using these medications if they have kidney disease, stomach ulcers, or other relevant medical conditions
Rest in a quiet, darkened room
Cold or warm compresses applied to the forehead or neck
Stress management techniques, including relaxation exercises or meditation
Patients should maintain a headache diary noting frequency, severity, timing, and potential triggers. This information can help identify patterns and guide discussions with healthcare providers about optimal management strategies.
Patients are encouraged to report suspected side effects to the MHRA through the Yellow Card Scheme (yellowcard.mhra.gov.uk).
Whilst most headaches associated with Wegovy are benign and self-limiting, certain warning signs warrant prompt medical evaluation. Patients should contact their GP or prescribing clinician if they experience:
Severe or worsening headaches that do not respond to standard analgesics or that progressively intensify despite continued treatment. Headaches that are significantly more severe than any previously experienced require medical assessment to exclude serious underlying causes.
Sudden-onset severe headache (often described as "thunderclap" headache) reaching maximum intensity within seconds to minutes requires immediate medical attention via emergency services (999), as this may indicate serious conditions such as subarachnoid haemorrhage, though such events are not specifically linked to Wegovy.
Headaches accompanied by neurological symptoms including:
Visual disturbances (blurred vision, double vision, visual field defects)
Weakness or numbness in the face, arms, or legs
Difficulty speaking or understanding speech
Balance problems or coordination difficulties
Confusion or altered consciousness
Seizures
These features may indicate conditions requiring urgent investigation, such as stroke or increased intracranial pressure, and necessitate same-day medical assessment.
Persistent headaches lasting beyond the first 12 weeks of treatment or those that significantly impact daily functioning should be discussed with a healthcare provider. The prescriber may consider:
Temporarily pausing dose escalation
Reducing to a previously tolerated dose
Investigating alternative causes
Referring to a specialist if headaches have features suggesting a primary headache disorder
Headaches with other concerning symptoms such as persistent vomiting, fever, neck stiffness, or changes in vision should prompt medical review to exclude conditions such as meningitis or other serious pathology.
Patients should also inform their healthcare provider if headaches necessitate frequent use of analgesics (more than 10–15 days per month), as medication-overuse headache can develop and complicate the clinical picture. Regular follow-up appointments provide opportunities to discuss any concerns and ensure treatment remains appropriate and well-tolerated.
When evaluating headaches in patients taking Wegovy, it is essential to consider alternative or contributing causes beyond the medication itself. A comprehensive assessment helps ensure appropriate management and avoids incorrectly attributing symptoms solely to semaglutide.
Lifestyle and dietary changes accompanying weight loss efforts may independently trigger headaches. Patients often simultaneously modify their diet, increase physical activity, and alter sleep patterns—all of which can influence headache susceptibility. Caffeine withdrawal is particularly relevant; individuals who reduce coffee, tea, or cola consumption as part of dietary changes may experience withdrawal headaches, typically occurring 12–24 hours after the last caffeine intake and lasting several days.
Concurrent medical conditions should be considered. Conditions such as:
Hypertension or blood pressure fluctuations
Sleep apnoea, which is common in individuals with obesity
Temporomandibular joint disorders
Cervical spine problems
Primary headache disorders (tension-type headache, migraine)
Sinusitis or other infections
These conditions may coincidentally present or worsen during Wegovy treatment without being causally related to the medication.
Medication interactions warrant consideration. Patients taking multiple medications should review their complete medication list with their pharmacist or GP, as some drugs can contribute to headaches or interact with metabolic changes induced by weight loss.
Hormonal factors may be relevant, particularly in women. Weight loss can potentially influence reproductive hormone levels, which might affect headache patterns in those with menstrual-related headaches, though evidence for this specific to Wegovy is limited. Additionally, some women may experience changes in the effectiveness or side effect profile of hormonal contraceptives during significant weight loss.
Psychological factors, including stress, anxiety, or depression—which may themselves be related to weight concerns or lifestyle changes—can manifest as tension-type headaches. The psychological adjustment to new eating patterns and body image changes during weight loss may contribute to stress-related headaches.
There is no official link between Wegovy and serious neurological conditions, but any persistent or concerning headache pattern should be properly investigated to exclude unrelated pathology. A thorough clinical assessment, including detailed history and appropriate examination, helps distinguish between medication-related headaches and those requiring alternative management approaches.
Most Wegovy-related headaches are mild to moderate and occur during the dose escalation phase, typically improving within 8–12 weeks as the body adapts to treatment. Persistent headaches beyond 12 weeks warrant medical review.
Yes, over-the-counter analgesics such as paracetamol (up to 1g four times daily) or ibuprofen (400mg three times daily with food) are generally safe and effective for managing Wegovy-related headaches. Consult your pharmacist or GP if you have kidney disease, stomach ulcers, or other relevant conditions.
Most headaches do not require stopping Wegovy and can be managed with hydration, regular meals, and standard analgesics. However, contact your GP if headaches are severe, worsening, persistent beyond 12 weeks, or accompanied by neurological symptoms such as visual disturbances or weakness.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.