Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for treating type 2 diabetes mellitus. Whilst clinical trials demonstrate significant efficacy in glycaemic control for many patients, individual responses vary considerably. Understanding why Ozempic may not work for you requires consideration of multiple factors, including dosage adequacy, injection technique, medication adherence, concurrent medical conditions, and lifestyle behaviours. This article explores common reasons for reduced effectiveness and provides guidance on optimising treatment outcomes in line with UK clinical practice and NICE recommendations.
Quick Answer: Ozempic may not work due to inadequate dosing, poor injection technique, insufficient treatment duration, dietary factors, medication interactions, advanced pancreatic dysfunction, or non-adherence to the once-weekly regimen.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Whilst clinical trials demonstrate significant efficacy in glycaemic control and weight reduction for many patients, individual responses vary considerably. Understanding why Ozempic may not produce expected results requires consideration of multiple physiological, pharmacological, and behavioural factors.
The medication works by mimicking the action of endogenous GLP-1, enhancing glucose-dependent insulin secretion, suppressing inappropriate glucagon release, slowing gastric emptying, and promoting satiety through central nervous system pathways. However, the degree to which these mechanisms translate into clinical benefit depends on numerous variables, including baseline pancreatic beta-cell function, concurrent medications, adherence patterns, and individual metabolic characteristics.
It is important to recognise that 'not working' can mean different things to different patients. Some may expect rapid weight loss when Ozempic is primarily prescribed for glycaemic control, whilst others may not achieve target HbA1c reductions despite appropriate dosing. The MHRA-approved indication focuses on diabetes management, and whilst weight loss often occurs as a secondary benefit, this is not guaranteed for all patients. Realistic expectations, informed by discussion with healthcare professionals, are essential for evaluating treatment success.
Individual variation in drug metabolism, receptor sensitivity, and disease progression all contribute to heterogeneous treatment outcomes. The effectiveness of Ozempic should generally be assessed after approximately 3 months on a stable maintenance dose, as this provides sufficient time to evaluate changes in HbA1c levels. NICE guidance (NG28) provides recommendations for GLP-1 receptor agonist use within the type 2 diabetes treatment pathway, typically as part of combination therapy when other treatments have not achieved glycaemic targets.
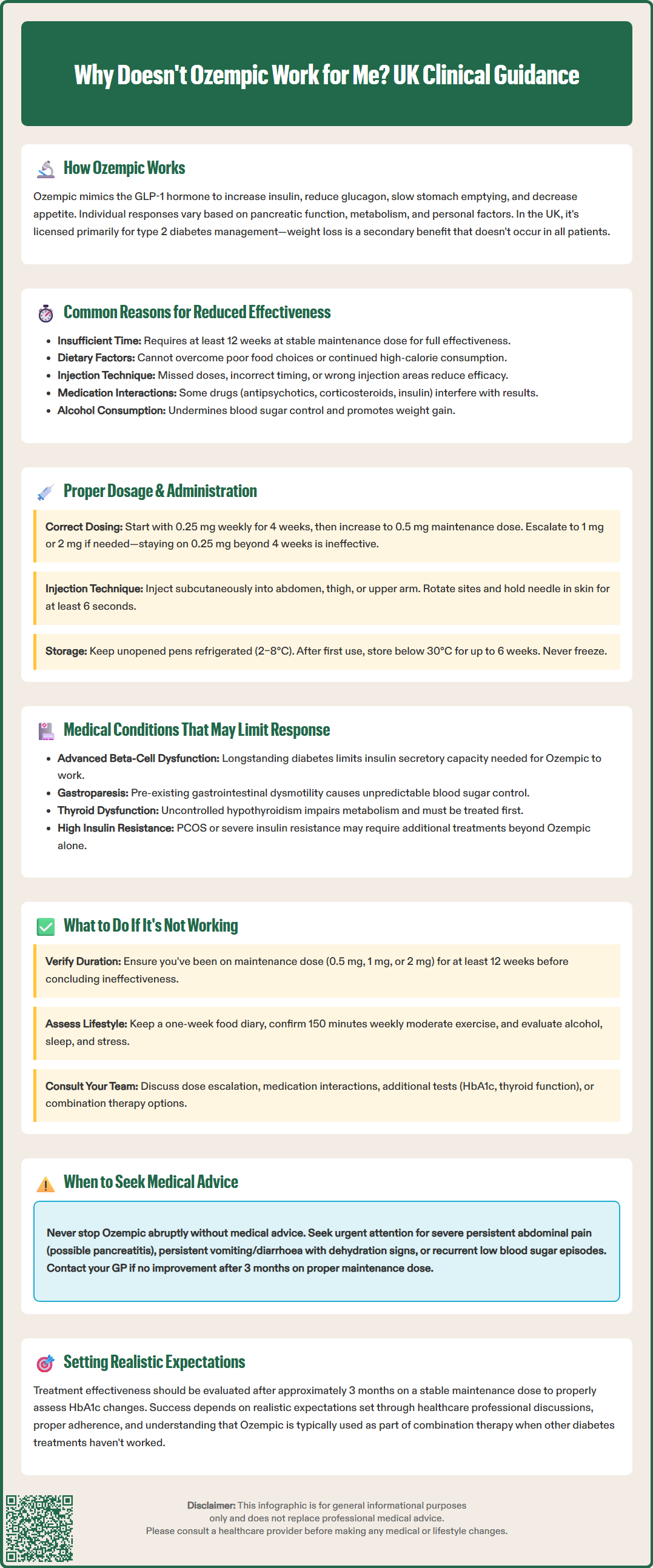
Several factors commonly contribute to diminished Ozempic effectiveness. Inadequate duration of treatment represents a frequent issue, as the full therapeutic effect typically requires assessment after about 12 weeks on a stable maintenance dose. Patients may prematurely conclude the medication is ineffective before reaching steady-state plasma concentrations or achieving maximal pharmacodynamic effects.
Dietary and lifestyle factors significantly influence outcomes. Ozempic enhances satiety and reduces appetite, but these effects can be overridden by continued consumption of calorie-dense foods or large portion sizes. The medication facilitates behavioural change but does not eliminate the need for dietary modification. Patients who do not engage with structured dietary advice or physical activity recommendations may experience limited benefits, particularly regarding weight management.
Medication adherence poses another critical challenge. Ozempic requires once-weekly subcutaneous injection, and missed doses or irregular administration patterns compromise therapeutic efficacy. If a dose is missed, it should be administered within 5 days of the scheduled date; otherwise, skip that dose and take the next one on the usual day. Some patients may also inject incorrectly—for instance, into areas with reduced subcutaneous tissue or lipohypertrophy—leading to erratic absorption. Proper injection technique, including site rotation and appropriate needle depth, is essential for consistent drug delivery.
Concurrent medications may interfere with Ozempic's action. Semaglutide delays gastric emptying, which may impact the absorption of oral medications. Particular caution is needed with medicines that have a narrow therapeutic index, such as warfarin, where additional monitoring may be required. Medications that promote weight gain—including some antipsychotics, corticosteroids, or insulin regimens—may counteract the weight-reducing effects of semaglutide. Additionally, alcohol consumption can impair glycaemic control and contribute to weight gain, potentially masking Ozempic's benefits.
Ozempic dosing follows a structured titration schedule designed to minimise gastrointestinal adverse effects whilst achieving therapeutic plasma concentrations. The standard regimen begins with 0.25 mg once weekly for four weeks, serving as an initiation dose rather than a therapeutic dose. This is increased to 0.5 mg weekly, which represents the first maintenance dose for many patients. If additional glycaemic control is required after at least four weeks, the dose may be increased to 1 mg weekly, with a maximum licensed dose of 2 mg weekly available for those needing further intensification.
Patients who remain on the 0.25 mg initiation dose beyond the recommended four-week period are unlikely to achieve optimal results, as this dose is insufficient for therapeutic effect. Similarly, some individuals may require the higher 1 mg or 2 mg doses to achieve target HbA1c reductions, particularly those with higher baseline values or longer diabetes duration. Underdosing represents a common, correctable cause of apparent treatment failure.
Injection technique critically influences drug absorption and efficacy. Ozempic should be administered subcutaneously into the abdomen, thigh, or upper arm, with site rotation to prevent lipohypertrophy. Injecting into areas of lipohypertrophy, scar tissue, or muscle can result in unpredictable absorption. The pen device should have the flow checked before first use of a new pen only (not before each injection), and the needle should remain in the skin for at least six seconds after depression of the dose button to ensure complete delivery. Injections should be given on the same day each week, though the day may be changed if the time since the last dose is at least 2 days.
Storage conditions also matter: Ozempic pens must be stored in a refrigerator (2–8°C) before first use, then may be kept at room temperature (below 30°C) for up to six weeks. Exposure to excessive heat or freezing temperatures can denature the protein, rendering it ineffective. Patients should inspect the solution before each injection, discarding any pen that appears cloudy, discoloured, or contains particles.
Certain underlying medical conditions can significantly impair Ozempic's effectiveness. Advanced pancreatic beta-cell dysfunction represents a primary limitation, as semaglutide's glucose-lowering effect depends substantially on residual insulin secretory capacity. Patients with longstanding type 2 diabetes or those with very elevated HbA1c levels may have insufficient beta-cell reserve to respond adequately to GLP-1 receptor stimulation. In such cases, combination therapy with basal insulin or other agents may be necessary.
Gastroparesis or severe gastrointestinal dysmotility may paradoxically reduce Ozempic's efficacy. Whilst the medication intentionally slows gastric emptying, pre-existing severe dysmotility can lead to unpredictable nutrient absorption, erratic postprandial glucose excursions, and intolerable gastrointestinal symptoms that limit dose escalation. Patients with documented gastroparesis require careful assessment before initiating GLP-1 receptor agonists.
Thyroid dysfunction, particularly hypothyroidism, can impair metabolic rate and weight loss efforts. Uncontrolled hypothyroidism should be optimised before attributing lack of response solely to Ozempic. Similarly, polycystic ovary syndrome (PCOS) and other conditions associated with insulin resistance may require additional interventions beyond GLP-1 receptor agonist therapy alone. It is important to note that Ozempic is not indicated for PCOS or weight management alone in the UK.
Patients with a history of pancreatitis or gallbladder disease require careful monitoring, as these conditions are noted cautions in the SmPC. Severe gastrointestinal adverse effects may lead to dehydration, which can worsen renal function. While dose adjustment is not typically required for renal impairment, monitoring for dehydration is important.
The role of genetic factors influencing drug metabolism or receptor function remains investigational. Specific pharmacogenomic markers for semaglutide response are not established in routine clinical practice. Renal impairment does not typically require dose adjustment for Ozempic, as it is eliminated primarily through protein catabolism rather than renal excretion, though severe renal disease may alter overall metabolic responses to therapy.
If Ozempic appears ineffective after an adequate trial period, a systematic approach is warranted. First, verify that you have been on the appropriate maintenance dose (0.5 mg, 1 mg, or 2 mg weekly) for at least 12 weeks, as this timeframe is necessary to assess true therapeutic response through HbA1c measurement. Review your injection technique with your practice nurse or diabetes specialist nurse, ensuring proper subcutaneous administration, site rotation, and complete dose delivery.
Assess adherence and lifestyle factors honestly. Keep a food diary for one week to identify potential dietary patterns that may counteract the medication's effects. Consider whether you are engaging in regular physical activity as recommended by NICE guidance (typically 150 minutes of moderate-intensity activity weekly). Evaluate alcohol intake, sleep quality, and stress levels, all of which influence metabolic health and treatment outcomes.
Contact your GP or diabetes care team to discuss your concerns. They may recommend:
Dose escalation if you are not yet on the maximum dose
Review of concurrent medications that may interfere with efficacy
Additional investigations, including HbA1c measurement, thyroid function tests, or assessment for complications
Combination therapy with other glucose-lowering agents (such as metformin, SGLT2 inhibitors, or basal insulin)
Referral to specialist diabetes services for complex cases or consideration of alternative GLP-1 receptor agonists
Do not discontinue Ozempic abruptly without medical advice, as this may lead to deterioration in glycaemic control. If you miss a dose, administer it within 5 days of the scheduled date; otherwise, skip that dose and take the next one on your usual day.
Seek urgent medical attention or contact NHS 111 if you experience severe, persistent abdominal pain (which could indicate pancreatitis), persistent vomiting or diarrhoea with signs of dehydration, or recurrent hypoglycaemia (particularly if you also take insulin or sulfonylureas).
Some patients may benefit from switching to alternative GLP-1 receptor agonists (such as dulaglutide or liraglutide), as individual responses can vary between agents within the same class. Your healthcare team can guide appropriate next steps based on your specific clinical circumstances, treatment goals, and any adverse effects experienced. Remember that diabetes management often requires a personalised, multifaceted approach, and apparent treatment failure with one agent does not preclude success with alternative strategies.
If you experience any suspected side effects, you or your healthcare professional can report these via the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk.
Ozempic typically requires at least 12 weeks on a stable maintenance dose (0.5 mg, 1 mg, or 2 mg weekly) to assess therapeutic response through HbA1c measurement. The initial 0.25 mg dose is for tolerability only and is not therapeutically effective.
Yes, injecting into areas of lipohypertrophy, scar tissue, or muscle can result in unpredictable absorption. Proper subcutaneous administration into the abdomen, thigh, or upper arm with site rotation and keeping the needle in skin for at least 6 seconds ensures consistent drug delivery.
Contact your GP or diabetes care team to review your dose, injection technique, and adherence. They may recommend dose escalation, combination therapy with other glucose-lowering agents, additional investigations, or referral to specialist diabetes services for complex cases.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.