
Weight loss injections such as semaglutide (Wegovy) and liraglutide (Saxenda) have transformed obesity management in the UK, yet some patients experience disappointing results. Understanding why weight loss injections may not be working requires examining multiple factors—from medication dosing and administration technique to lifestyle habits and underlying medical conditions. This article explores the common reasons for suboptimal response to GLP-1 receptor agonists, realistic expectations based on clinical evidence, and when to seek medical review. Whether you're experiencing a weight loss plateau or minimal initial response, identifying the underlying cause is essential for optimising treatment outcomes and exploring alternative strategies.
Quick Answer: Weight loss injections may not work due to insufficient treatment duration, inadequate dosing, poor injection technique, compensatory eating behaviours, medication interactions, or underlying metabolic conditions affecting individual response.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly prescribed for weight management in the UK. These prescription-only medications work by mimicking natural hormones that regulate appetite and glucose metabolism, leading to reduced hunger, increased satiety, and slower gastric emptying. The MHRA has licensed these treatments for adults with a body mass index (BMI) of 30 kg/m² or above, or 27 kg/m² with weight-related comorbidities, though NHS access may be more restricted.
Realistic expectations are crucial when starting weight loss injections. Clinical trials demonstrate varying outcomes by product: semaglutide typically achieves 12-15% weight loss, while liraglutide shows approximately 8-10% weight reduction over 12-18 months when combined with lifestyle modifications. Individual responses vary considerably, with some patients experiencing more modest results. Weight loss is rarely linear; plateaus are common and do not necessarily indicate treatment failure.
It is important to understand that these medications are not 'quick fixes' but rather tools to support comprehensive weight management programmes. NICE guidance emphasises that pharmacological interventions should be integrated with dietary changes, increased physical activity, and behavioural support. For example, semaglutide (Wegovy) under NICE TA875 is recommended within specialist weight management services with specific eligibility criteria. The timeframe for noticeable results also varies—whilst some patients report reduced appetite within days, measurable weight loss typically becomes apparent after 4-8 weeks of treatment. Patients should maintain realistic expectations and understand that slower, sustained weight loss is generally more maintainable than rapid reduction.
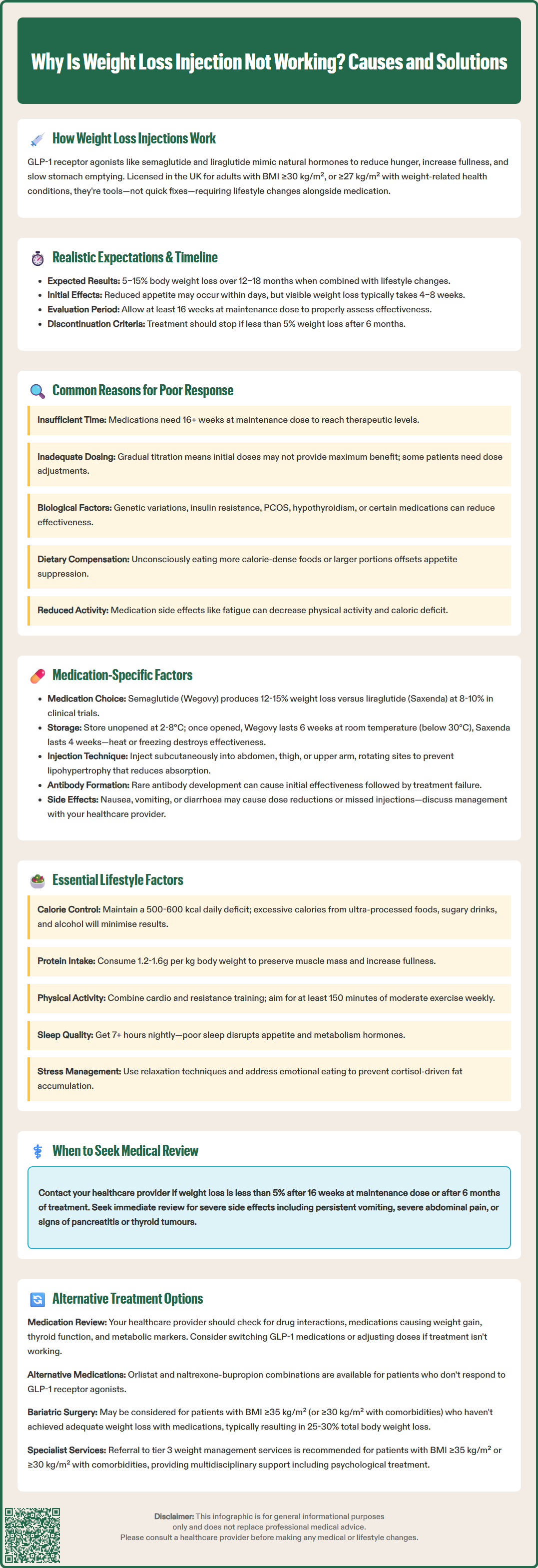
Several factors can contribute to suboptimal response to weight loss injections, and understanding these can help identify potential solutions. Insufficient treatment duration is amongst the most common reasons for perceived treatment failure. Many patients expect immediate results, but these medications require time to reach therapeutic levels and exert their full metabolic effects. Assessment timeframes vary by product—liraglutide (Saxenda) requires evaluation after 12 weeks at the full 3mg dose, while semaglutide (Wegovy) has a longer evaluation period as specified in the SmPC and NICE guidance.
Inadequate dosing represents another significant factor. Weight loss injections follow specific titration schedules, gradually increasing from starter doses to maintenance levels. This stepwise approach minimises gastrointestinal side effects but means that patients may not experience maximum therapeutic benefit during the initial weeks. Some individuals may require dose adjustments or longer titration periods, particularly if they experience tolerability issues that prevent reaching target doses.
Biological factors also play a crucial role in treatment response. Individual metabolic differences may influence how effectively these medications work. Patients with certain conditions such as polycystic ovary syndrome (PCOS) or insulin resistance may experience different responses, while untreated hypothyroidism should be corrected before assessing medication efficacy. Additionally, certain medications—particularly some antipsychotics (e.g., olanzapine, clozapine), corticosteroids, and certain antidepressants (e.g., mirtazapine)—can promote weight gain and potentially counteract the effects of weight loss injections.
Compensatory eating behaviours may develop unconsciously. Some patients, feeling less hungry overall, may consume more calorie-dense foods during meals or increase portion sizes when they do eat, inadvertently offsetting the appetite-suppressing effects of the medication. Similarly, reduced physical activity due to fatigue or other side effects can diminish the overall caloric deficit necessary for weight loss.
The pharmacological properties of different weight loss injections can significantly influence treatment outcomes. Semaglutide (Wegovy) and liraglutide (Saxenda) have distinct pharmacokinetic profiles that affect their efficacy and tolerability. Semaglutide, administered once weekly, has a longer half-life and generally demonstrates superior weight loss outcomes in clinical trials, with patients losing an average of 12-15% of body weight. Liraglutide, requiring daily injections, typically results in 8-10% weight loss over similar timeframes, as shown in the STEP and SCALE trials respectively.
Injection technique and storage can impact medication effectiveness. These biologics are temperature-sensitive and must be stored according to product-specific instructions. Wegovy (semaglutide) pens can be kept at room temperature (below 30°C) for up to 6 weeks after first use, while Saxenda (liraglutide) pens can be stored for up to 1 month. Exposure to excessive heat or freezing can denature the active ingredient, rendering it less effective. Patients should also ensure proper injection technique—administering subcutaneously into the abdomen, thigh, or upper arm, rotating injection sites to prevent lipohypertrophy, which can affect absorption.
Antibody formation is uncommon with GLP-1 receptor agonists and rarely affects clinical efficacy. According to the SmPCs, while some patients may develop antibodies, this seldom results in reduced effectiveness. More commonly, gastrointestinal side effects—including nausea, vomiting, and diarrhoea—may lead some patients to reduce their dose prematurely or take the medication inconsistently, compromising efficacy.
Patients should be aware of potential safety concerns, including gallbladder disease (presenting as right upper abdominal pain, fever, or jaundice) and, rarely, pancreatitis. People with diabetes should be monitored for diabetic retinopathy when glycaemic control improves rapidly. Patients should report suspected side effects to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
Weight loss injections are most effective when integrated into comprehensive lifestyle modification programmes. Dietary patterns remain fundamental to successful weight management, regardless of pharmacological support. Patients who continue consuming excessive calories—particularly from ultra-processed foods, sugary beverages, and alcohol—may experience minimal weight loss despite medication. NICE recommends a balanced, calorie-controlled diet with a deficit of approximately 500-600 kcal per day for sustainable weight loss.
The composition of one's diet also matters. Protein intake is particularly important, as adequate protein helps preserve lean muscle mass during weight loss and enhances satiety. Patients should aim to include protein sources at each meal and may benefit from personalised dietary advice from a registered dietitian. Focus should be on whole foods, including vegetables, fruits, whole grains, lean proteins, and healthy fats, whilst limiting refined carbohydrates and saturated fats. Some individuals may benefit from structured programmes such as the NHS Digital Weight Management Programme, which provides evidence-based dietary guidance.
Physical activity levels significantly influence treatment outcomes. Whilst weight loss injections reduce appetite, they do not directly increase energy expenditure. Regular exercise—combining both cardiovascular activity and resistance training—enhances fat loss, preserves muscle mass, and improves metabolic health. UK Chief Medical Officers' guidelines recommend at least 150 minutes of moderate-intensity activity weekly plus muscle-strengthening activities on at least two days per week, though higher levels may be necessary for significant weight loss.
Sleep quality and stress management are often overlooked factors. Poor sleep (fewer than 7 hours nightly) disrupts hormones regulating appetite and metabolism, potentially undermining medication effects. Chronic stress elevates cortisol levels, which can promote abdominal fat accumulation and emotional eating. Patients should be encouraged to address these factors through sleep hygiene practices, stress-reduction techniques, and, where appropriate, psychological support for emotional eating patterns or binge eating disorder.
Patients should seek medical review if they do not achieve adequate weight loss according to product-specific criteria. For liraglutide (Saxenda), the SmPC advises discontinuation if less than 5% weight loss is achieved after 12 weeks at the full 3mg daily dose. For semaglutide (Wegovy), assessment timeframes follow NICE TA875 guidance and the SmPC. Additionally, patients should contact their GP or prescribing clinician if they experience severe or persistent side effects, including severe abdominal pain, persistent vomiting, signs of pancreatitis, gallbladder problems (right upper abdominal pain, fever, jaundice), or symptoms of thyroid concerns (neck lump, difficulty swallowing, persistent hoarseness).
Medication review is essential when weight loss injections prove ineffective. Healthcare professionals should assess for potential drug interactions, review concurrent medications that may promote weight gain, and evaluate underlying medical conditions that might impair treatment response. Thyroid function tests, HbA1c, and other metabolic markers may help identify contributing factors. Women of childbearing potential should use effective contraception during treatment, as these medications are not recommended during pregnancy.
Alternative pharmacological options exist for patients who do not respond to GLP-1 receptor agonists. These include orlistat (a lipase inhibitor) and naltrexone-bupropion (Mysimba), though NHS availability varies by local commissioning decisions. Tirzepatide (a dual GLP-1/GIP receptor agonist) has UK authorisation for weight management, but NHS access depends on NICE appraisal and local commissioning. For individuals with BMI ≥40 kg/m² or 35-39.9 kg/m² with significant comorbidities who have not achieved adequate weight loss with pharmacotherapy, bariatric surgery may be considered. In specific circumstances, those with BMI 30-34.9 kg/m² and recent-onset type 2 diabetes may also be eligible. Procedures such as gastric bypass or sleeve gastrectomy typically result in 25-30% total body weight loss and significant improvement in obesity-related conditions.
Patients should also be referred to specialist weight management services (Tier 3/4) if available locally. These multidisciplinary teams—including dietitians, psychologists, exercise specialists, and physicians—can provide comprehensive assessment and tailored interventions. Addressing psychological factors, such as binge eating disorder or depression, through cognitive behavioural therapy or other evidence-based approaches may significantly enhance treatment outcomes. Remember, weight management is a long-term journey, and lack of response to one intervention does not preclude success with alternative approaches.
Whilst some patients notice reduced appetite within days, measurable weight loss typically becomes apparent after 4–8 weeks of treatment. Full efficacy should be evaluated after at least 16 weeks at the maintenance dose, as these medications require time to reach therapeutic levels and exert their full metabolic effects.
Yes, certain medications—particularly some antipsychotics, corticosteroids, and antidepressants—can promote weight gain and potentially counteract the effects of GLP-1 receptor agonists. A comprehensive medication review with your healthcare provider is essential if weight loss injections are not producing expected results.
Contact your GP or prescribing clinician if you experience less than 5% weight loss after 16 weeks at maintenance dose, develop severe or persistent side effects, or notice symptoms such as severe abdominal pain, persistent vomiting, or signs of thyroid problems. Your healthcare provider can assess for underlying causes and discuss alternative treatment options.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.