
Weight loss injections such as semaglutide (Wegovy) and liraglutide (Saxenda) are not necessarily lifelong treatments. The duration of therapy varies considerably between individuals and is guided by clinical response, tolerability, and UK regulatory approvals. NICE guidance limits NHS treatment with semaglutide to a maximum of 2 years within specialist weight management services, whilst liraglutide has specific continuation criteria outlined in its technology appraisal. These glucagon-like peptide-1 (GLP-1) receptor agonists are prescribed as part of a comprehensive weight management programme that includes dietary modification, increased physical activity, and behavioural support. Treatment duration depends on individual factors including response to medication, obesity-related comorbidities, and patient preference.
Quick Answer: Weight loss injections are not necessarily lifelong treatments; NHS guidance limits semaglutide (Wegovy) to a maximum of 2 years within specialist services, with duration determined by individual response and clinical need.
Weight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), are not necessarily lifelong treatments, though the duration varies considerably between individuals. The treatment duration is product-specific and guided by clinical evidence and UK regulatory approvals.
For semaglutide (Wegovy), NICE technology appraisal guidance limits NHS treatment to a maximum of 2 years within specialist weight management services. For liraglutide (Saxenda), continuation criteria are specified in its NICE technology appraisal and SmPC, with regular reviews to assess ongoing benefit.
The Medicines and Healthcare products Regulatory Agency (MHRA) has approved these medications for weight management as part of a comprehensive programme that includes dietary modification, increased physical activity, and behavioural support. Clinical trials have demonstrated that the most substantial weight loss occurs during the first year of treatment, with weight stabilisation or continued gradual loss in the second year.
Treatment duration depends on several factors:
Individual response to medication
Achievement of weight loss targets
Presence of obesity-related comorbidities (type 2 diabetes, hypertension, sleep apnoea)
Tolerability and side effects
Patient preference and lifestyle factors
Safety considerations (e.g., pregnancy planning, history of pancreatitis or gallbladder disease)
NICE guidance emphasises that weight loss injections should be considered as part of a long-term weight management strategy rather than a quick fix. The decision to continue or discontinue treatment should be made collaboratively between patient and clinician, with regular review appointments to assess efficacy, tolerability, and ongoing need. NHS treatment is provided within multidisciplinary specialist weight management services (tier 3/4) alongside diet, activity and behavioural support.
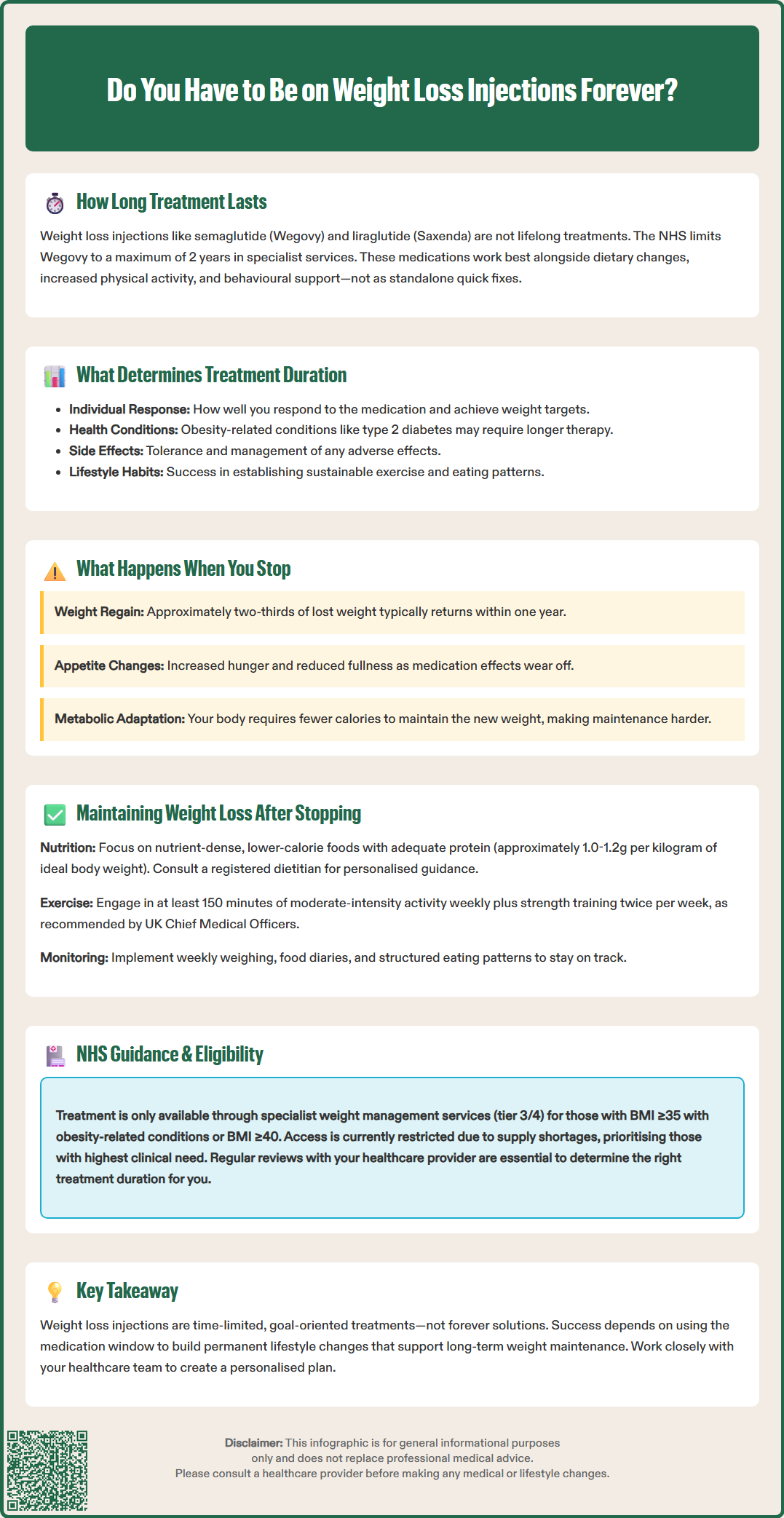
Discontinuation of weight loss injections frequently results in weight regain, though the extent varies considerably between individuals. The STEP 1 extension trial examining semaglutide demonstrated that participants regained approximately two-thirds of their lost weight within one year of stopping treatment. This phenomenon reflects the complex biological mechanisms underlying obesity, which is now recognised as a chronic relapsing disease rather than simply a lifestyle choice.
When GLP-1 receptor agonists are withdrawn, several physiological changes occur. The medication's effects on appetite suppression, gastric emptying, and satiety signalling diminish within days to weeks. Hunger and food cravings typically return to pre-treatment levels as the body's weight regulation mechanisms adapt. This is likely influenced by hormonal changes that collectively promote increased food intake, though the specific patterns vary between individuals.
Additionally, metabolic rate may decrease following significant weight loss, a phenomenon known as adaptive thermogenesis. This means the body requires fewer calories to maintain its new lower weight than would be predicted, making weight maintenance more challenging without pharmaceutical support.
Common experiences after stopping treatment include:
Increased appetite and reduced feelings of fullness
Gradual weight regain over 6-12 months
Return of food-related thoughts and cravings
Potential worsening of obesity-related conditions if significant weight is regained
It is important to note that there is no official link between stopping these medications and any dangerous withdrawal syndrome. GLP-1 receptor agonists do not require tapering when discontinuing. However, patients should discuss discontinuation plans with their healthcare provider rather than stopping abruptly, to ensure appropriate monitoring and support during the transition period.
Seek urgent medical attention if you experience:
Severe, persistent abdominal pain (with or without vomiting)
Signs of gallbladder disease (pain in upper right abdomen, especially after eating)
Persistent vomiting or signs of dehydration
Allergic reactions

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWhilst challenging, maintaining weight loss after discontinuing injections is possible with comprehensive lifestyle strategies and ongoing support. Research indicates that individuals who successfully maintain weight loss typically adopt permanent behavioural changes rather than viewing the medication period as a temporary intervention. The key lies in establishing sustainable habits during treatment that can continue independently afterwards.
Successful weight maintenance requires a multifaceted approach. Dietary modifications should focus on nutrient-dense, lower-calorie foods with adequate protein intake. A registered dietitian can provide personalised advice, but many adults may aim for approximately 1.0-1.2g of protein per kilogram of ideal body weight (higher amounts may be appropriate for some individuals but should be discussed with healthcare professionals, particularly for those with kidney disease). Regular physical activity is crucial, with the UK Chief Medical Officers recommending at least 150 minutes of moderate-intensity exercise weekly, supplemented by strength training on at least two days per week. Many individuals benefit from continued engagement with weight management programmes, whether through NHS services, commercial providers, or peer support groups.
Strategies that improve maintenance success include:
Self-monitoring: Regular weighing (weekly) and food diary keeping
Structured eating patterns: Consistent meal times and portion control
Environmental modifications: Reducing availability of high-calorie foods at home
Stress management: Addressing emotional eating triggers
Adequate sleep: 7-9 hours nightly, as sleep deprivation increases appetite hormones
Some clinicians may discuss the concept of intermittent or reduced-dose treatment rather than complete cessation. However, it's important to note that this approach is considered off-label with limited supporting evidence and is not current NHS practice. Any such strategy should only be considered under specialist supervision. Patients should contact their healthcare provider if they experience weight regain or worsening of obesity-related conditions after stopping treatment, as this may warrant reassessment of their weight management strategy.
The NHS follows NICE guidance on obesity (CG189) and specific technology appraisals for weight loss medications when determining the appropriate duration of therapy. These guidelines emphasise that pharmacological treatment should be time-limited and goal-oriented, with regular review to assess continued benefit and necessity. Access to these medications through the NHS is currently restricted due to supply constraints and cost considerations, with priority given to individuals with the highest clinical need.
For semaglutide (Wegovy), NICE technology appraisal guidance specifies a maximum treatment duration of 2 years within specialist weight management services. For liraglutide (Saxenda), continuation criteria are detailed in its specific NICE technology appraisal and SmPC, with regular reviews to assess ongoing benefit.
Product-specific continuation criteria apply, as outlined in the relevant NICE technology appraisals and SmPCs. These typically include achieving a minimum percentage weight loss within a specified timeframe. If these thresholds are not met, the medication should be discontinued, as the likelihood of achieving clinically meaningful benefit with continued use is low.
NHS prescribing criteria typically require:
BMI ≥35 kg/m² with obesity-related comorbidities, or BMI ≥40 kg/m² (with lower thresholds for people from certain ethnic groups)
Evidence of previous unsuccessful weight loss attempts through lifestyle modification
Commitment to a comprehensive weight management programme
Treatment within a specialist weight management service (tier 3/4)
Absence of contraindications (including pregnancy, breastfeeding, personal or family history of medullary thyroid carcinoma, multiple endocrine neoplasia syndrome type 2)
The decision to continue treatment is made on an individual basis, considering factors such as the presence of type 2 diabetes, cardiovascular risk, and the likelihood of significant health deterioration if weight is regained. Patients should discuss their individual treatment plan with their healthcare provider, as local NHS formularies and prescribing policies may vary across different integrated care boards (ICBs). Regular monitoring of weight, metabolic parameters, and treatment-related side effects is essential throughout the treatment duration.
The duration of weight loss injection therapy is highly individualised and depends on multiple clinical, psychological, and practical factors. Understanding these variables helps patients and clinicians make informed decisions about treatment continuation or cessation. There is no official link between any single factor and a predetermined treatment duration; rather, the decision emerges from a holistic assessment of the individual's circumstances.
Clinical factors play a primary role in determining treatment duration. Individuals with obesity-related comorbidities such as type 2 diabetes, obstructive sleep apnoea, or non-alcoholic fatty liver disease may require longer treatment periods, as weight regain could significantly worsen these conditions. The severity of obesity at baseline also influences duration—those with higher BMI values typically need extended treatment compared to individuals with lower BMI values. Secondary causes of obesity (such as thyroid dysfunction, certain medications, or Cushing's syndrome) should be evaluated and managed appropriately, as addressing these directly may impact weight management strategies.
Behavioural and psychological factors are equally important. Patients who successfully establish sustainable lifestyle changes during treatment—including regular physical activity, structured eating patterns, and effective stress management—are more likely to maintain weight loss after discontinuation. Conversely, those with significant psychological barriers such as binge eating disorder, emotional eating patterns, or inadequate social support may benefit from extended treatment whilst addressing these underlying issues through psychological intervention.
Practical considerations include:
Treatment response: Rapid, substantial weight loss may allow earlier cessation with appropriate maintenance strategies
Side effect profile: Persistent gastrointestinal symptoms, gallbladder issues, or other adverse effects may limit long-term tolerability
Accessibility: Availability through NHS specialist services varies by region; patients should check local policies and referral pathways
Patient preference: Some individuals prefer time-limited treatment, whilst others value ongoing pharmaceutical support
Regular review appointments are essential to reassess these factors and adjust the treatment plan accordingly. Patients should maintain open communication with their healthcare provider about their goals, challenges, and preferences regarding treatment duration. Any suspected side effects should be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
NICE guidance limits NHS treatment with semaglutide (Wegovy) to a maximum of 2 years within specialist weight management services. Liraglutide (Saxenda) has specific continuation criteria outlined in its technology appraisal, with regular reviews to assess ongoing benefit.
Weight regain is common after discontinuation, with clinical trials showing approximately two-thirds of lost weight regained within one year of stopping. However, maintaining weight loss is possible with comprehensive lifestyle strategies including dietary modification, regular physical activity, and ongoing behavioural support.
GLP-1 receptor agonists do not require tapering and there is no dangerous withdrawal syndrome associated with stopping. However, patients should discuss discontinuation plans with their healthcare provider to ensure appropriate monitoring and support during the transition period.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.