
Experiencing a bad taste in your mouth whilst taking GLP-1 medications is an uncommon but recognised side effect that can affect some patients during treatment. GLP-1 receptor agonists—including semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda)—are widely prescribed in the UK for type 2 diabetes and weight management. Whilst these medicines offer significant therapeutic benefits, taste disturbances such as metallic, bitter, or unpleasant sensations may occur, often linked to delayed gastric emptying and gastrointestinal effects. Understanding why this happens, how long it typically lasts, and practical management strategies can help you navigate this side effect whilst maintaining effective treatment.
Quick Answer: A bad taste in the mouth with GLP-1 medications is an uncommon side effect, typically related to delayed gastric emptying and gastrointestinal effects, and often improves within 4 to 8 weeks.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists are increasingly prescribed medications for type 2 diabetes and weight management in the UK. Whilst these medicines offer significant therapeutic benefits, some patients report experiencing an unpleasant taste in their mouth during treatment—often described as metallic, bitter, or simply 'off'.
The exact mechanism behind taste disturbances with GLP-1 medications is not fully understood, though several factors may contribute. GLP-1 receptor agonists work by mimicking the natural incretin hormone GLP-1, which slows gastric emptying, reduces appetite, enhances insulin secretion and suppresses inappropriate glucagon secretion. The delayed gastric emptying may potentially lead to gastro-oesophageal reflux, which could contribute to an unpleasant taste sensation. Some clinicians hypothesise that these medications might also affect saliva composition or flow, though this remains speculative.
Another potential contributor is the medication's effect on the gastrointestinal system more broadly. Many patients experience nausea—one of the most common adverse effects of GLP-1 therapy—which can be accompanied by taste changes. It's worth noting that other common causes of taste changes should also be considered, including oral/dental disease, recent viral infections, smoking, dry mouth, and other medications.
It is important to note that taste disturbances are generally considered a minor adverse effect and do not typically indicate a serious medical problem. However, understanding why they occur can help patients manage expectations and implement practical strategies to minimise discomfort during treatment.
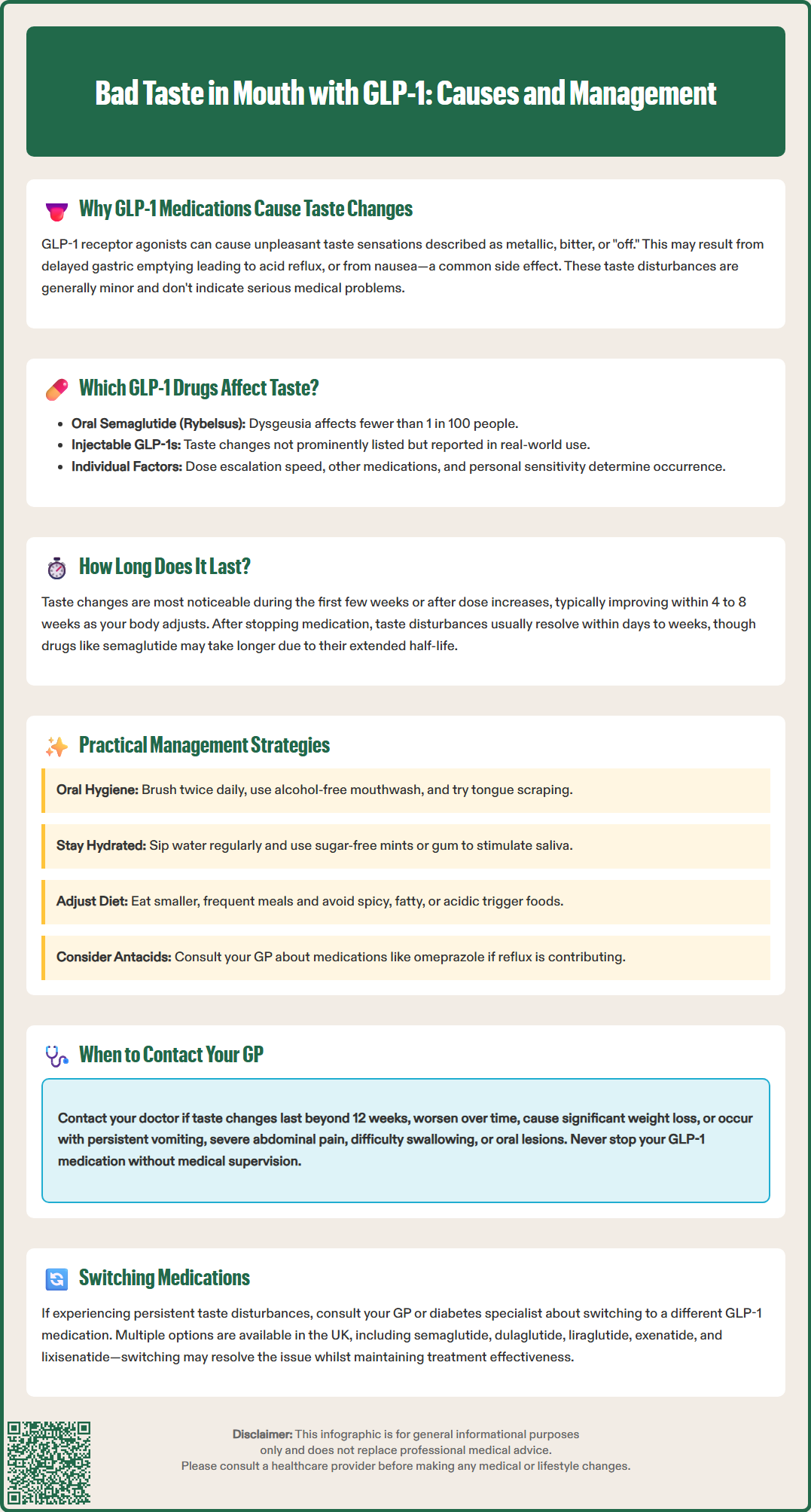
Several GLP-1 receptor agonists are currently licensed for use in the UK, including semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), exenatide (Bydureon BCise), and lixisenatide (Lyxumia). Taste disturbances have been reported with various GLP-1 medications, though the frequency varies between products.
According to the Summary of Product Characteristics (SmPCs), dysgeusia (altered taste) is listed as an uncommon side effect (affecting fewer than 1 in 100 but more than 1 in 1,000 people) for oral semaglutide (Rybelsus). For injectable semaglutide (Ozempic, Wegovy) and other GLP-1 receptor agonists, taste disturbances are not specifically highlighted among the most common adverse effects, though gastrointestinal symptoms that might indirectly affect taste perception are well-documented.
Patient experiences in clinical practice sometimes differ from clinical trial data, with some individuals reporting taste changes even when not prominently featured in product literature. The relationship between formulation type (oral versus injectable) and taste effects requires further research to establish definitive patterns.
Individual susceptibility varies considerably. Factors such as dose escalation speed, concurrent medications, underlying gastrointestinal conditions, and personal sensitivity all influence whether a patient experiences taste changes. If you are concerned about taste disturbances with your current GLP-1 medication, discuss alternative options with your GP or diabetes specialist, as switching to a different agent within the class may provide relief whilst maintaining therapeutic benefits.
The duration of taste disturbances associated with GLP-1 therapy varies considerably between individuals. For many patients, taste changes are most noticeable during the initial weeks of treatment or following dose increases, often coinciding with the period when gastrointestinal adverse effects such as nausea are most prominent.
In clinical practice, taste-related symptoms frequently improve or resolve within 4 to 8 weeks as the body adjusts to the medication, though this timeframe is based on clinical experience rather than specific studies. This adaptation period likely reflects physiological tolerance to the drug's effects on gastric emptying and gastrointestinal function. Some patients report that the unpleasant taste becomes less bothersome over time, even if it does not disappear entirely, as they become accustomed to the sensation.
However, a minority of patients experience persistent taste disturbances that continue throughout treatment. In such cases, the symptom may be related to ongoing gastro-oesophageal reflux or other gastrointestinal effects that do not fully resolve. If taste changes persist beyond 8 to 12 weeks or significantly affect your quality of life and nutritional intake, it is important to discuss this with your healthcare provider.
The relationship between dose and taste disturbance is not entirely clear, though higher doses of GLP-1 medications generally produce more pronounced gastrointestinal effects. Gradual dose titration, as recommended in product SmPCs, may help minimise taste-related adverse effects by allowing the body time to adapt. If you discontinue the medication, taste disturbances typically resolve within days to weeks, depending on the drug's half-life (for example, semaglutide has a half-life of approximately one week, so effects may persist for several weeks after stopping).
Whilst taste disturbances can be bothersome, several practical strategies may help reduce their impact and improve your comfort during GLP-1 treatment. These approaches focus on managing the underlying causes—particularly gastro-oesophageal reflux and altered oral environment—and minimising the perception of unpleasant tastes.
Dietary and lifestyle modifications can be particularly effective:
Maintain good oral hygiene: Brush your teeth at least twice daily and consider using an alcohol-free mouthwash. Some patients find that tongue scraping helps remove coating that may contribute to taste changes.
Stay well hydrated: Drinking plenty of water throughout the day helps maintain saliva flow and can dilute unpleasant tastes. Sipping water regularly may be more effective than consuming large amounts at once.
Try sugar-free mints or gum: These can stimulate saliva production and mask unpleasant tastes. Mint, citrus, or cinnamon flavours are often helpful.
Eat smaller, more frequent meals: This approach aligns with the medication's mechanism and may reduce reflux that contributes to bad taste.
Avoid trigger foods: Spicy, fatty, or acidic foods may worsen reflux and taste disturbances. Keep a food diary to identify personal triggers.
Medical interventions may also be appropriate:
Discuss antacid therapy with your GP: If reflux appears to be contributing, medications such as proton pump inhibitors (e.g., omeprazole) or H2-receptor antagonists (e.g., famotidine) may help, though these should only be used under medical supervision.
Review timing of medication: For oral semaglutide (Rybelsus), ensuring proper administration (on an empty stomach with up to 120 mL of water, then waiting at least 30 minutes before any food, drink, or other oral medicines) may reduce gastrointestinal effects.
Consider dose adjustment: If taste changes are severe, your prescriber may recommend temporarily reducing the dose before re-escalating more gradually.
Nutritional considerations are important, particularly if taste changes affect your appetite or food choices. Ensure you maintain adequate nutrition and do not avoid entire food groups due to taste disturbances. If dietary intake becomes significantly compromised, request a referral to a dietitian for personalised advice.
A dental review may also be helpful if oral lesions or poor dentition might be contributing to taste changes.
Whilst taste changes associated with GLP-1 medications are generally benign and self-limiting, certain circumstances warrant medical review. Understanding when to seek advice ensures that more serious underlying conditions are not overlooked and that your treatment remains safe and effective.
Contact your GP or diabetes specialist if:
Taste disturbances persist beyond 12 weeks or worsen over time rather than improving, as this may indicate an alternative cause requiring investigation.
You experience significant weight loss or nutritional compromise due to reduced appetite or food aversion related to taste changes.
Taste disturbances are accompanied by other concerning symptoms such as persistent vomiting, severe abdominal pain, difficulty swallowing, or signs of dehydration.
You develop complete loss of taste (ageusia) rather than altered taste, as this may suggest a different underlying condition.
You notice oral lesions, persistent dry mouth, or signs of oral infection alongside taste changes, which may require specific treatment.
The taste disturbance significantly affects your quality of life or adherence to treatment, as alternative therapeutic options may be available.
Seek urgent medical attention if you experience:
Severe, persistent abdominal pain (especially if radiating to the back) with or without vomiting, which could indicate pancreatitis
Right upper quadrant pain, fever, or yellowing of the skin/eyes, which might suggest gallbladder disease
Severe chest pain, difficulty breathing, facial swelling, or signs of an allergic reaction
For urgent advice, call NHS 111. For life-threatening symptoms or suspected anaphylaxis, call 999.
Your healthcare provider can assess whether the taste disturbance is likely related to your GLP-1 medication or whether further investigation is needed. Blood tests, oral examination, or referral to an ear, nose, and throat (ENT) specialist may be appropriate in cases where the cause is unclear or symptoms are atypical. Remember that medication adjustments should only be made under medical supervision—do not stop or alter your GLP-1 therapy without consulting your prescriber, as this may affect your diabetes control or weight management goals.
If you suspect your taste disturbance is a side effect of your medication, you can report it through the MHRA Yellow Card scheme, which helps monitor the safety of medicines in the UK.
GLP-1 medications slow gastric emptying, which may lead to gastro-oesophageal reflux and altered taste perception. The exact mechanism is not fully understood, but gastrointestinal effects and possible changes to saliva composition may contribute to metallic, bitter, or unpleasant taste sensations.
Taste disturbances are usually most noticeable during the first few weeks of treatment or after dose increases and often improve within 4 to 8 weeks as the body adjusts. If symptoms persist beyond 12 weeks or significantly affect quality of life, consult your GP.
Practical strategies include maintaining good oral hygiene, staying well hydrated, using sugar-free mints or gum, eating smaller frequent meals, and avoiding spicy or fatty foods that may worsen reflux. If symptoms are severe, discuss antacid therapy or dose adjustment with your GP.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.