Microdosing GLP-1 for rheumatoid arthritis has emerged as a topic of interest, yet remains unsupported by clinical evidence or UK regulatory approval. Glucagon-like peptide-1 (GLP-1) receptor agonists are licensed for type 2 diabetes and weight management, not inflammatory conditions. Microdosing involves using substantially lower doses than standard therapeutic regimens, falling outside approved prescribing guidance. Whilst preclinical research suggests potential anti-inflammatory properties, no randomised controlled trials demonstrate efficacy in rheumatoid arthritis. NICE guidance (NG100) recommends disease-modifying antirheumatic drugs (DMARDs) as standard care. This article examines the current evidence, potential risks, and the importance of evidence-based treatment decisions in rheumatoid arthritis management.
Quick Answer: GLP-1 receptor agonists are not licensed or supported by clinical evidence for rheumatoid arthritis treatment in the UK, and microdosing remains experimental without established safety or efficacy data.
Glucagon-like peptide-1 (GLP-1) is a naturally occurring hormone produced in the intestines that plays a crucial role in regulating blood glucose levels and appetite. GLP-1 receptor agonists are a class of medications originally developed and licensed for the treatment of type 2 diabetes mellitus, with some formulations also approved by the MHRA for weight management in adults with obesity or overweight with weight-related comorbidities, under specialist services as per NICE guidance (TA875).
These medications work by mimicking the action of natural GLP-1, binding to GLP-1 receptors throughout the body. Their primary mechanisms include:
Enhancing insulin secretion from pancreatic beta cells in a glucose-dependent manner
Suppressing glucagon release, which reduces hepatic glucose production
Slowing gastric emptying, promoting satiety and reducing food intake
Acting on appetite centres in the brain to decrease hunger signals
Microdosing refers to the practice of using substantially lower doses of a medication than those typically prescribed for its licensed indications. In the context of GLP-1 receptor agonists, microdosing involves using doses below the standard therapeutic range for diabetes or weight management. This approach falls outside the Summary of Product Characteristics (SmPC) dosing regimens and is not supported by UK guidance. Proponents suggest that lower doses may confer benefits whilst minimising adverse effects, though this approach remains experimental and is not supported by current regulatory approvals.
It is important to note that GLP-1 receptor agonists are not currently licensed for the treatment of rheumatoid arthritis or other inflammatory conditions in the UK. Any use outside approved indications would be considered off-label prescribing, which requires careful clinical justification and informed patient consent. These are prescription-only medicines that should only be obtained through legitimate healthcare channels.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereEmerging preclinical research has identified GLP-1 receptors in various immune cells and tissues, leading to scientific interest in potential anti-inflammatory properties. Laboratory studies have suggested that GLP-1 receptor activation may modulate inflammatory pathways, though the clinical relevance of these findings remains uncertain.
Preclinical observations include:
Reduction in pro-inflammatory cytokines such as interleukin-6 (IL-6) and tumour necrosis factor-alpha (TNF-α) in animal models
Potential effects on immune cell function and inflammatory signalling cascades
Possible protective effects in models of inflammatory disease
However, there is currently no robust clinical evidence supporting the use of GLP-1 receptor agonists for rheumatoid arthritis specifically. No randomised controlled trials have been published demonstrating efficacy in reducing disease activity, joint inflammation, or radiographic progression in patients with rheumatoid arthritis. The existing evidence base consists primarily of:
Small observational studies in patients with diabetes who also have inflammatory conditions
Mechanistic studies exploring theoretical anti-inflammatory pathways
Indirect evidence from cardiovascular outcome trials showing reduced inflammatory markers in people with type 2 diabetes (which cannot be extrapolated to rheumatoid arthritis or to microdosing)
NICE guidance for rheumatoid arthritis management (NG100) does not include GLP-1 receptor agonists among recommended treatment options. The standard of care remains disease-modifying antirheumatic drugs (DMARDs), including conventional synthetic DMARDs like methotrexate as first-line therapy, with escalation to biological DMARDs or targeted synthetic DMARDs if disease activity remains inadequately controlled, following a treat-to-target approach.
Patients should be aware that there is no official link established between GLP-1 therapy and improvement in rheumatoid arthritis symptoms or disease progression. Any purported benefits remain speculative and require rigorous clinical investigation before recommendations can be made.
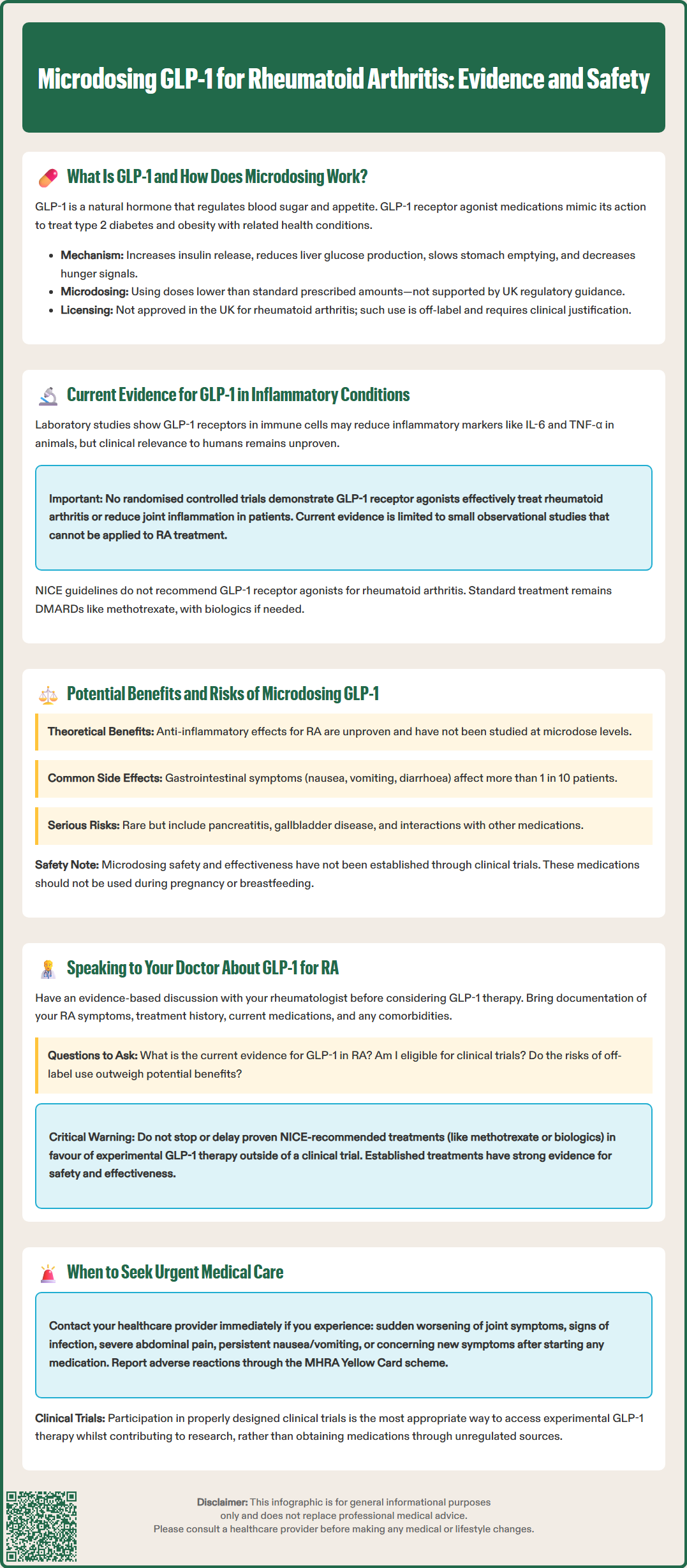
Whilst the theoretical benefits of GLP-1 receptor agonists in inflammatory conditions are being explored in research settings, patients considering this approach must understand both the potential advantages and significant risks associated with off-label use.
Theoretical potential benefits (currently unproven for rheumatoid arthritis and not studied at microdose levels):
Possible anti-inflammatory effects through modulation of immune pathways
Weight reduction, which may indirectly benefit joint symptoms in overweight patients
Cardiovascular risk reduction, relevant given increased cardiovascular disease risk in rheumatoid arthritis (established in type 2 diabetes populations at therapeutic doses only)
Improved metabolic parameters in patients with concurrent metabolic syndrome
Known adverse effects of GLP-1 receptor agonists at standard doses include:
Gastrointestinal symptoms: nausea, vomiting, diarrhoea, constipation, and abdominal discomfort (very common, affecting more than 1 in 10 patients)
Hypoglycaemia: particularly when used with other glucose-lowering medications
Injection site reactions: erythema, pruritus, or nodules
Pancreatitis: rare but serious, requiring immediate medical attention if severe abdominal pain develops
Gallbladder disease: increased risk of cholelithiasis and cholecystitis
Thyroid effects: thyroid C-cell tumours observed in rodents; human relevance unknown; patients should be monitored for thyroid symptoms as per SmPC guidance
Diabetic retinopathy complications: potential worsening in patients with pre-existing retinopathy, particularly with rapid HbA1c reductions (observed with semaglutide)
The safety profile of microdosing specifically has not been established through clinical trials. Lower doses may reduce gastrointestinal side effects, but this remains speculative. Furthermore, microdosing provides no guarantee of efficacy for any indication, including rheumatoid arthritis.
Important safety considerations:
GLP-1 receptor agonists may interact with other medications through delayed gastric emptying, potentially affecting absorption of oral medicines, particularly those with a narrow therapeutic index
Renal impairment: exenatide should be avoided if eGFR <30 mL/min/1.73m²; for semaglutide, liraglutide and dulaglutide, no dose adjustment is generally required, but monitor in severe renal impairment, especially with gastrointestinal losses
Pregnancy and breastfeeding: GLP-1 therapies are not recommended during pregnancy; discontinue if pregnancy occurs; avoid during breastfeeding
Long-term safety data for off-label use in inflammatory conditions is absent
Suspected adverse reactions should be reported via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
If you are interested in exploring GLP-1 therapy for rheumatoid arthritis, it is essential to have an open, evidence-based conversation with your rheumatologist or GP. Self-medication or obtaining these prescription-only medicines through unregulated sources poses serious health risks and is not advisable.
Prepare for your consultation by:
Documenting your current rheumatoid arthritis symptoms, disease activity, and treatment history
Listing all current medications, including DMARDs, biologics, corticosteroids, and analgesics
Noting any comorbidities, particularly diabetes, obesity, cardiovascular disease, or gastrointestinal conditions
Being honest about your treatment goals and what has prompted interest in GLP-1 therapy
Questions to discuss with your doctor:
What is the current evidence for GLP-1 use in rheumatoid arthritis?
Are there any ongoing clinical trials I might be eligible for? (You can search the NIHR 'Be Part of Research' website, but always discuss eligibility with your clinician)
What are the established treatment options that might better address my symptoms?
Could weight management through other means benefit my joint symptoms?
What are the risks of off-label GLP-1 use given my medical history?
Your doctor will likely emphasise that NICE-recommended treatments for rheumatoid arthritis (NG100) have substantial evidence supporting their efficacy and safety. These include methotrexate as first-line therapy, with escalation to combination conventional synthetic DMARDs or biological agents if disease activity remains inadequately controlled. These treatments have been rigorously studied in rheumatoid arthritis populations and have established benefit-risk profiles. It is important not to stop or delay evidence-based DMARD or biologic therapy in favour of experimental GLP-1 therapy outside a clinical trial.
When to seek urgent medical advice:
Sudden worsening of joint pain, swelling, or stiffness
Signs of infection (fever, malaise, localised warmth)
Severe abdominal pain (potential pancreatitis if on GLP-1 therapy)
Unexplained persistent nausea or vomiting
Any concerning new symptoms after starting any new medication
According to NICE Quality Standard 33, if you have suspected persistent synovitis, you should be referred to rheumatology within 3 working days and assessed within 3 weeks.
Ultimately, treatment decisions should be made collaboratively, based on current evidence, regulatory approvals, and individualised assessment of benefits and risks. Participation in properly designed clinical trials, if available, represents the most appropriate way to access experimental therapies whilst contributing to the evidence base for future patients.
No, GLP-1 receptor agonists are not licensed for rheumatoid arthritis in the UK. They are approved only for type 2 diabetes and weight management under specific NICE guidance, and any use for inflammatory conditions would be considered off-label prescribing.
There is currently no robust clinical evidence supporting GLP-1 use in rheumatoid arthritis. No randomised controlled trials have demonstrated efficacy in reducing disease activity or joint inflammation, and existing evidence consists only of preclinical studies and theoretical mechanisms.
NICE guidance (NG100) recommends disease-modifying antirheumatic drugs (DMARDs) as standard care, with methotrexate as first-line therapy. If disease activity remains inadequately controlled, treatment should escalate to combination conventional synthetic DMARDs or biological agents following a treat-to-target approach.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.