
Weight loss injections such as semaglutide (Wegovy) and liraglutide (Saxenda) are increasingly prescribed for weight management in the UK, but their use in people with Crohn's disease requires careful consideration. Crohn's disease is a chronic inflammatory bowel condition that affects the gastrointestinal tract, causing symptoms including abdominal pain, diarrhoea, and weight changes. Whilst some individuals with Crohn's disease may struggle with weight gain—particularly during remission or when taking corticosteroids—the gastrointestinal side effects of GLP-1 receptor agonists overlap significantly with IBD symptoms. UK product licences include specific cautions regarding use in severe gastrointestinal disease, making specialist assessment essential before considering these treatments.
Quick Answer: Weight loss injections are generally not recommended for people with Crohn's disease, with liraglutide (Saxenda) specifically contraindicated in inflammatory bowel disease and semaglutide requiring caution in severe gastrointestinal conditions.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereWeight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly prescribed for weight management in the UK. These medications work by mimicking the action of glucagon-like peptide-1, a naturally occurring hormone that regulates appetite and blood glucose levels. By slowing gastric emptying and promoting feelings of fullness, these injections help reduce caloric intake and facilitate weight loss.
Crohn's disease is a chronic inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal tract, from mouth to anus, though it most commonly involves the terminal ileum and colon. The condition causes inflammation, ulceration, and structural damage to the bowel wall, leading to symptoms including abdominal pain, diarrhoea, fatigue, and unintended weight loss. Crohn's disease follows a relapsing-remitting pattern, with periods of active inflammation (flares) alternating with remission.
Interestingly, weight management in Crohn's disease presents unique challenges. Whilst many patients experience weight loss during active disease due to malabsorption, reduced appetite, and increased metabolic demands, some individuals—particularly those in remission or taking corticosteroids—may struggle with weight gain. The intersection of obesity and IBD is increasingly recognised, with some evidence suggesting that excess weight may influence disease activity and treatment outcomes, though more research is needed in this area.
Understanding both the mechanism of weight loss injections and the complex nature of Crohn's disease is essential when considering whether these treatments are appropriate for individuals living with IBD. The gastrointestinal effects of GLP-1 agonists require careful consideration in the context of an already compromised digestive system, and UK product licences include specific cautions regarding use in severe gastrointestinal disease.
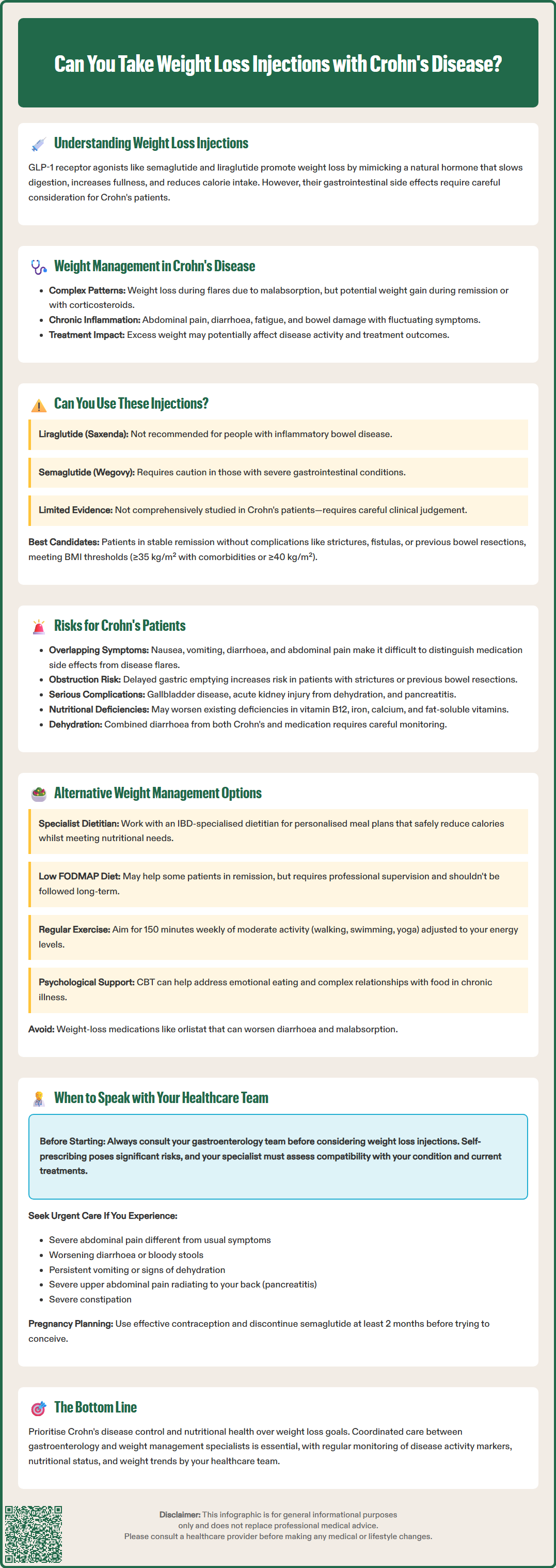
The suitability of weight loss injections for people with Crohn's disease varies depending on the specific medication and individual circumstances. According to the UK Summary of Product Characteristics (SmPC), liraglutide (Saxenda) is not recommended in patients with inflammatory bowel disease. For semaglutide (Wegovy), the SmPC advises caution in patients with severe gastrointestinal disease, including gastroparesis.
The MHRA-approved weight loss injections available in the UK have been primarily studied in populations without significant gastrointestinal disease. Consequently, their safety profile and efficacy in Crohn's patients, particularly those with active inflammation or stricturing disease, has not been comprehensively established. This evidence gap means prescribers must exercise clinical judgement when considering these treatments.
In the UK, NICE guidance specifies that these medications should only be prescribed within specialist weight management services and for people meeting specific BMI thresholds (typically BMI ≥35 kg/m² with weight-related comorbidities or ≥40 kg/m² without), alongside diet and physical activity interventions.
Key factors influencing whether weight loss injections may be appropriate include:
Disease activity: Patients in stable remission may be better candidates than those experiencing active flares
Location and extent of disease: Individuals with upper gastrointestinal or extensive small bowel involvement may face greater risks
Presence of complications: Strictures, fistulas, or previous bowel resections may increase the risk of adverse effects
Current medication regimen: While there are no known direct pharmacokinetic interactions with immunosuppressants or biologics, monitoring for overlapping gastrointestinal symptoms is important
Nutritional status: Patients already experiencing malnutrition or deficiencies may not be suitable candidates
NICE guidance on obesity management acknowledges that certain medical conditions require specialist input when considering pharmacological weight loss interventions. For Crohn's patients, this typically means coordinated care between gastroenterology and weight management services, ensuring that any treatment plan accounts for the complexities of inflammatory bowel disease whilst addressing legitimate weight concerns.
The primary concern with using GLP-1 receptor agonists in Crohn's disease relates to their gastrointestinal side effects, which overlap significantly with IBD symptoms. Common adverse effects include nausea, vomiting, diarrhoea, abdominal pain, and constipation, affecting a substantial proportion of users according to UK SmPCs. For someone with Crohn's disease, distinguishing between medication side effects and disease flare symptoms can prove challenging, potentially delaying appropriate treatment adjustments.
Delayed gastric emptying, the mechanism by which these injections promote satiety, poses particular risks for Crohn's patients. Individuals with stricturing disease or those who have undergone bowel resection may already experience altered gut motility. Further slowing of gastrointestinal transit could increase the risk of obstruction, particularly in areas of narrowing. The European Medicines Agency's Pharmacovigilance Risk Assessment Committee (PRAC) has identified ileus as an adverse reaction associated with GLP-1 receptor agonists, making this a recognised rather than merely theoretical risk.
Additional significant risks include:
Gallbladder disease: GLP-1 receptor agonists are associated with increased risk of gallstones and cholecystitis
Acute kidney injury: Particularly in the context of severe gastrointestinal side effects causing dehydration
Pancreatitis: A rare but serious adverse effect that requires immediate discontinuation of treatment if suspected
Nutritional considerations are paramount. Crohn's disease frequently causes malabsorption of essential nutrients, including vitamin B12, iron, calcium, and fat-soluble vitamins. Weight loss injections, by reducing food intake, may exacerbate existing deficiencies or create new ones. Patients with previous bowel resections face heightened risk, as they may already have compromised absorptive capacity.
Further considerations include:
Dehydration risk: Combined effects of diarrhoea (from both Crohn's and medication) may increase dehydration risk
Medication absorption: While generally minimal, delayed gastric emptying could affect absorption of oral medications with a narrow therapeutic index
Monitoring requirements: Regular assessment of disease activity markers, nutritional status, and weight trends is essential
Patients should be counselled about these risks and encouraged to report any worsening gastrointestinal symptoms promptly to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk), as distinguishing between expected side effects and disease progression requires clinical expertise.
For individuals with Crohn's disease seeking weight management, several alternatives to injectable medications may prove safer and more appropriate. Dietary modification represents the cornerstone of weight management in IBD, though it requires specialist input to ensure nutritional adequacy whilst creating a caloric deficit. A registered dietitian with IBD expertise can develop personalised meal plans that account for individual triggers, disease location, and nutritional requirements, as recommended by the British Dietetic Association.
The low FODMAP diet, whilst primarily used to manage IBS symptoms, has shown benefit for some Crohn's patients in remission experiencing functional gut symptoms (not for treating active inflammation). When carefully implemented under dietetic supervision, this approach may help identify problematic foods whilst supporting weight management goals. However, it should not be followed long-term without professional guidance due to potential nutritional inadequacies.
Physical activity offers multiple benefits for Crohn's patients, including weight management, improved bone health (important given increased osteoporosis risk), and enhanced mental wellbeing. NICE guidance recommends that adults aim for 150 minutes of moderate-intensity activity weekly. For those with active disease or fatigue, gentler options such as walking, swimming, or yoga may be more appropriate, with gradual progression as tolerated.
Psychological support through cognitive behavioural therapy (CBT) or other evidence-based approaches can address emotional eating, body image concerns, and the psychological impact of living with chronic illness. Many Crohn's patients develop complex relationships with food due to symptom triggers, making psychological input valuable for sustainable weight management.
Other pharmacological options, such as orlistat (which reduces fat absorption), are generally not recommended for Crohn's patients due to its contraindication in chronic malabsorption syndromes and the risk of exacerbating diarrhoea. Bariatric surgery, whilst effective for severe obesity, requires extremely careful consideration in IBD patients and should only be undertaken in specialist centres with expertise in both fields.
A multidisciplinary approach involving gastroenterologists, dietitians, specialist nurses, and potentially endocrinologists offers the best framework for safe, effective weight management in Crohn's disease, ensuring that interventions support rather than compromise overall health.
If you have Crohn's disease and are considering weight loss injections, it is essential to discuss this with your gastroenterology team before starting any new treatment. Self-prescribing or obtaining these medications through unregulated sources poses significant risks, particularly for individuals with complex medical conditions. Your specialist can assess whether weight loss injections are appropriate given your specific disease characteristics, current treatment regimen, and overall health status.
Contact your GP or IBD team promptly if you experience any of the following whilst taking weight loss injections:
Severe or persistent abdominal pain, particularly if different from your usual Crohn's symptoms
Significant worsening of diarrhoea or new-onset bloody stools
Persistent vomiting preventing adequate fluid or medication intake
Signs of dehydration (dark urine, dizziness, reduced urination)
Unexplained fever or signs of infection
Severe constipation or inability to pass wind (potential obstruction)
Symptoms suggesting pancreatitis (severe upper abdominal pain radiating to the back) – stop the medication immediately and seek urgent medical attention
For severe symptoms, contact NHS 111 for urgent advice or go to A&E/call 999 if you experience severe abdominal pain with vomiting, inability to pass stool or wind, or signs of severe dehydration.
Regular monitoring is crucial when combining weight loss treatments with Crohn's disease management. Your healthcare team should assess disease activity markers (such as faecal calprotectin or C-reactive protein), nutritional status (including vitamin and mineral levels), and weight trends at appropriate intervals.
Important considerations for women of childbearing age: GLP-1 receptor agonists are not recommended during pregnancy or breastfeeding. If you're planning pregnancy, discuss effective contraception with your healthcare provider and note that semaglutide typically should be discontinued at least 2 months before a planned pregnancy.
Before starting weight loss injections, ensure your healthcare team is aware of all medications you take. Report any suspected side effects to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
Remember that weight management in Crohn's disease should always prioritise disease control and nutritional health over cosmetic concerns. Achieving remission, preventing complications, and maintaining adequate nutrition form the foundation upon which any weight management strategy should be built. Your healthcare team can help you navigate these priorities whilst supporting your overall wellbeing and quality of life.
Weight loss injections are generally not recommended for people with Crohn's disease. Liraglutide (Saxenda) is specifically contraindicated in inflammatory bowel disease, whilst semaglutide (Wegovy) requires caution in severe gastrointestinal conditions due to overlapping side effects and potential complications.
The main risks include difficulty distinguishing medication side effects from disease flares, increased risk of bowel obstruction in patients with strictures, exacerbation of malnutrition, and gastrointestinal complications such as nausea, vomiting, and diarrhoea that overlap with Crohn's symptoms.
Safer alternatives include specialist dietetic support tailored to IBD, regular physical activity appropriate to disease activity, and psychological interventions such as cognitive behavioural therapy. A multidisciplinary approach involving gastroenterology and dietetic teams offers the safest framework for weight management in Crohn's disease.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.