
Non-alcoholic fatty liver disease, now termed metabolic dysfunction-associated steatotic liver disease (MASLD), affects approximately one in three UK adults. Whilst no medications are currently licensed specifically for fatty liver disease in the UK, GLP-1 receptor agonists—originally developed for type 2 diabetes—show promising benefits for liver health. These medications can reduce hepatic fat content, improve liver enzymes, and potentially slow fibrosis progression. This article examines which GLP-1 treatments may benefit fatty liver disease, the clinical evidence supporting their use, and how patients might access these therapies through the NHS.
Quick Answer: No GLP-1 receptor agonist is currently licensed specifically for fatty liver disease in the UK, but semaglutide and liraglutide show the most promising evidence for reducing hepatic steatosis and inflammation in patients with MASLD/NASH.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereNon-alcoholic fatty liver disease (NAFLD), now increasingly referred to as metabolic dysfunction-associated steatotic liver disease (MASLD), affects approximately one in three adults in the UK. This condition occurs when excess fat accumulates in the liver in people who drink little or no alcohol. The spectrum ranges from simple steatosis (fat accumulation) to non-alcoholic steatohepatitis (NASH, now termed MASH or metabolic dysfunction-associated steatohepatitis), which involves inflammation and can progress to cirrhosis and liver failure.
The condition is strongly associated with obesity, type 2 diabetes, and metabolic syndrome. Traditional management has focused on lifestyle modification—weight loss, dietary changes, and increased physical activity—as currently no medications are licensed in the UK specifically for MASLD/MASH. However, the emergence of GLP-1 receptor agonists (glucagon-like peptide-1 analogues) has opened new therapeutic possibilities.
GLP-1 receptor agonists were originally developed for type 2 diabetes management but have demonstrated significant benefits beyond glucose control. These medications mimic the action of naturally occurring GLP-1, a hormone that regulates appetite, insulin secretion, and various metabolic processes. Clinical trials have shown that GLP-1 receptor agonists can reduce liver fat content, improve liver enzyme levels, and potentially slow the progression of liver fibrosis.
Whilst these medications are not yet routinely prescribed specifically for fatty liver disease in the UK, their use is expanding as evidence accumulates. In UK primary care, risk assessment typically begins with calculating the FIB-4 score; those at intermediate or high risk may proceed to Enhanced Liver Fibrosis (ELF) testing or FibroScan, with referral to hepatology for those with suspected advanced fibrosis, in line with NICE guidance (NG49).
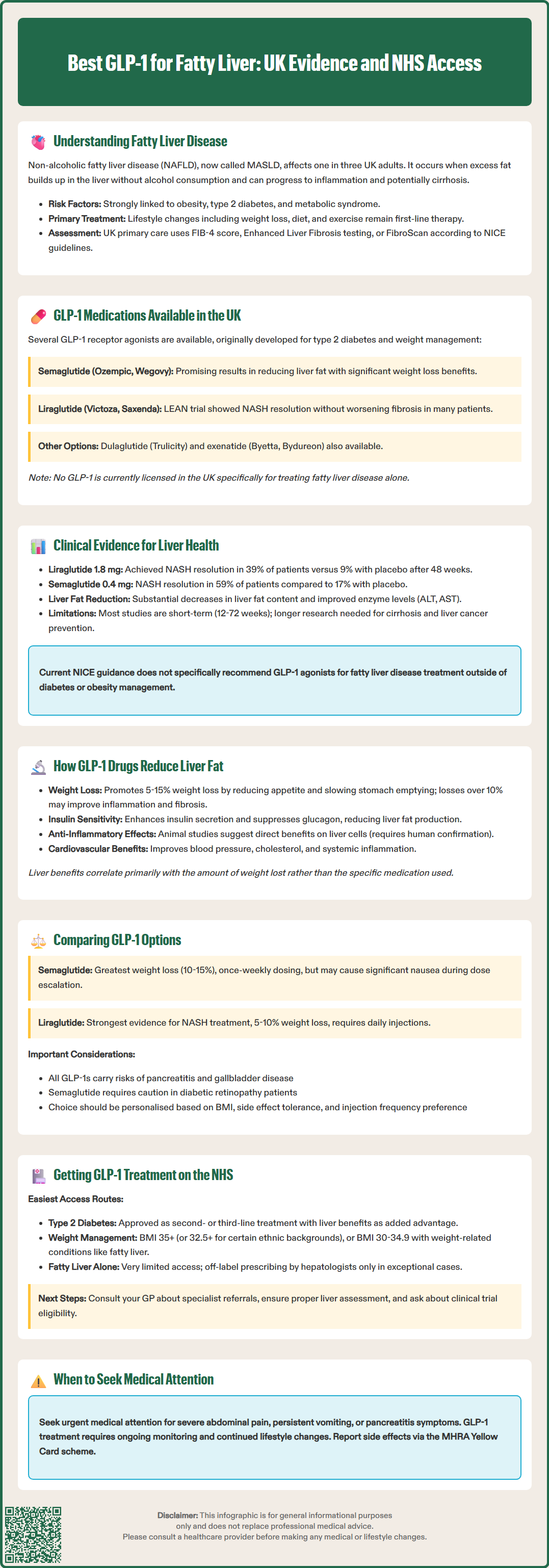
Several GLP-1 receptor agonists are currently available in the UK, though their primary licensed indications are for type 2 diabetes and, in some cases, weight management. The main agents include semaglutide (Ozempic for diabetes, Wegovy for weight management), liraglutide (Victoza for diabetes, Saxenda for weight management), dulaglutide (Trulicity for diabetes only), and exenatide (Byetta, Bydureon for diabetes only).
Semaglutide has garnered particular attention for its potential liver benefits. Available as a weekly subcutaneous injection for diabetes (Ozempic) or weight management (Wegovy), and as a daily oral tablet (Rybelsus) for diabetes only, semaglutide has demonstrated substantial weight loss and metabolic improvements in clinical trials. Studies specifically examining its effects on liver fat have shown promising results, with significant reductions in hepatic steatosis.
Liraglutide, a daily injection, was one of the first GLP-1 agonists to be studied extensively in NASH patients. The LEAN trial demonstrated that liraglutide could resolve NASH without worsening fibrosis in a significant proportion of patients. However, it is not currently licensed specifically for this indication in the UK.
It is important to note that no GLP-1 receptor agonist is currently licensed by the MHRA specifically for the treatment of fatty liver disease alone. These medications may be prescribed for patients with fatty liver who also have type 2 diabetes or meet criteria for weight management treatment. Off-label use for fatty liver disease specifically would be at the discretion of specialist hepatologists or endocrinologists, typically in research settings or exceptional clinical circumstances.
Patients interested in GLP-1 therapy for fatty liver should discuss their individual circumstances with their GP or specialist, as eligibility depends on multiple factors including BMI, diabetes status, and cardiovascular risk profile. Local formulary policies may also restrict access despite national guidance.
The evidence base for GLP-1 receptor agonists in fatty liver disease has expanded considerably in recent years. Multiple randomised controlled trials and observational studies have examined their hepatic effects, with generally encouraging results.
The LEAN trial (Liraglutide Efficacy and Action in NASH) was a landmark study published in The Lancet (2016) demonstrating that liraglutide 1.8 mg daily led to NASH resolution in 39% of patients compared to 9% in the placebo group after 48 weeks. Importantly, this occurred without worsening of fibrosis. Patients also experienced significant weight loss and improvements in metabolic parameters.
For semaglutide, a phase 2 trial published in the New England Journal of Medicine (2021) examined daily semaglutide 0.4 mg in NASH patients and found that 59% achieved NASH resolution compared to 17% with placebo. However, the trial did not demonstrate significant improvement in fibrosis. Studies using MRI-based measurements (MRI-PDFF) have shown that semaglutide can substantially reduce hepatic fat content, with reductions correlating with the degree of weight loss achieved.
Real-world evidence from UK and European databases suggests that patients with type 2 diabetes and fatty liver who receive GLP-1 therapy experience improvements in liver enzyme levels (ALT, AST) and non-invasive markers of fibrosis. However, long-term data on hard outcomes such as cirrhosis prevention or liver-related mortality are still accumulating.
It is worth noting that whilst these results are promising, most studies have been relatively short-term (12-72 weeks). The natural history of NAFLD spans decades, so longer-term studies are needed to confirm whether GLP-1 agonists can prevent progression to advanced fibrosis, cirrhosis, or hepatocellular carcinoma. Current NICE guidance (NG49) does not yet include specific recommendations for GLP-1 use in fatty liver disease outside the context of diabetes or obesity management.
GLP-1 receptor agonists exert their beneficial effects on the liver through multiple interconnected mechanisms, both direct and indirect. Understanding these pathways helps explain why these medications show promise beyond their original indication for diabetes.
Weight loss and caloric restriction represent the most significant mechanism. GLP-1 agonists act on appetite centres in the hypothalamus, promoting satiety and reducing food intake. They also slow gastric emptying, prolonging the feeling of fullness after meals. The resulting weight loss—typically 5-15% of body weight depending on the agent and dose—directly reduces hepatic fat accumulation. Even modest weight loss of 5-7% can significantly improve liver steatosis, whilst losses exceeding 10% may lead to improvements in inflammation and fibrosis.
Improved insulin sensitivity is another crucial factor. GLP-1 receptor agonists enhance glucose-dependent insulin secretion from pancreatic beta cells and suppress inappropriate glucagon release. This improved glycaemic control reduces hepatic glucose production and lipogenesis (fat synthesis in the liver). Better insulin sensitivity also reduces the flux of free fatty acids from adipose tissue to the liver, a key driver of hepatic steatosis.
Potential direct hepatic effects have also been identified in preclinical studies, though GLP-1 receptors are expressed at relatively low levels in the liver itself. Animal and laboratory studies suggest GLP-1 agonists may have anti-inflammatory and anti-fibrotic properties, potentially mediated through effects on hepatic stellate cells and Kupffer cells. They may also influence hepatic lipid metabolism by modulating enzymes involved in fatty acid oxidation and synthesis. However, these direct mechanisms require further confirmation in human studies.
Additionally, these medications improve cardiovascular risk factors—reducing blood pressure, improving lipid profiles, and decreasing systemic inflammation—all of which contribute to the metabolic milieu that drives fatty liver disease. Clinical evidence suggests that the magnitude of liver benefits largely tracks with the degree of weight loss achieved, regardless of which specific GLP-1 agent is used.
When considering GLP-1 receptor agonists for patients with fatty liver disease, several factors influence the choice of agent, though direct head-to-head comparisons specifically in NAFLD populations are limited.
Semaglutide appears to offer the greatest weight loss potential, with trials showing average reductions of 10-15% of body weight at the 2.4 mg weekly dose (Wegovy). For liver fat reduction, this translates to substantial improvements in hepatic steatosis. The convenience of once-weekly dosing may improve adherence. However, gastrointestinal side effects—particularly nausea—can be pronounced, especially during dose escalation. The oral formulation (Rybelsus) offers an alternative for patients who prefer not to inject, though it requires specific administration instructions (taken on an empty stomach with minimal water) and is licensed for diabetes only, not weight management.
Liraglutide has the most robust evidence base specifically in NASH, given the LEAN trial results. The daily injection allows for more gradual dose adjustment, which some patients find easier to tolerate. Weight loss is typically somewhat less than with semaglutide (5-10% on average), but still clinically meaningful. The daily dosing requirement may be less convenient for some patients.
Dulaglutide offers once-weekly convenience with a generally favourable tolerability profile. Whilst specific data in NAFLD are more limited, studies in diabetes populations show improvements in liver enzymes and metabolic parameters. It may be particularly suitable for patients who prioritise convenience and have concurrent diabetes. Dulaglutide is licensed for type 2 diabetes only, not for weight management.
Important safety considerations include the risk of pancreatitis (all GLP-1 agonists carry warnings about this), gallbladder disease (more common with greater weight loss), and a caution with semaglutide in patients with pre-existing diabetic retinopathy, where rapid improvement in glucose control may temporarily worsen retinopathy.
Patient-specific factors that influence choice include:
Concurrent diabetes: Patients with type 2 diabetes may have broader access through NHS prescribing pathways
BMI and weight loss goals: Higher BMI patients may benefit from agents with greater weight loss efficacy
Tolerability: Previous experience with gastrointestinal side effects may guide selection
Injection preference: Some patients strongly prefer weekly over daily injections, or oral over injectable formulations
Cardiovascular disease: Certain GLP-1 agonists have proven cardiovascular benefits, which may be relevant for high-risk patients
Ultimately, the choice should be individualised through shared decision-making between patient and clinician, considering the available evidence, licensed indications, local prescribing policies, and patient preferences.
Accessing GLP-1 receptor agonists specifically for fatty liver disease on the NHS can be challenging, as current prescribing pathways are primarily designed for diabetes and weight management rather than liver disease alone.
For patients with type 2 diabetes and fatty liver, access is more straightforward. NICE guidelines (NG28) recommend GLP-1 agonists as second- or third-line therapy for type 2 diabetes when metformin and other agents are insufficient or unsuitable. If you have both conditions, your GP or diabetes specialist can prescribe a GLP-1 agonist for diabetes management, with the liver benefits being an additional advantage.
For weight management, NICE Technology Appraisals (TA875 for semaglutide 2.4 mg; TA664 for liraglutide 3.0 mg) recommend considering GLP-1 agonists for adults with a BMI of 35 kg/m² or more (or 32.5 kg/m² or more for people from South Asian, Chinese, other Asian, Middle Eastern, Black African or African-Caribbean family backgrounds), or a BMI of 30-34.9 kg/m² with at least one weight-related comorbidity. Fatty liver disease may be considered such a comorbidity, though local implementation varies. Treatment is typically provided through specialist weight management services with defined monitoring and review periods.
For fatty liver disease without diabetes or obesity meeting treatment thresholds, NHS access to GLP-1 agonists is currently very limited. Specialist hepatologists may occasionally prescribe off-label in exceptional circumstances, particularly for patients with biopsy-proven NASH and significant fibrosis, but this is not routine practice.
Steps to explore GLP-1 treatment:
Consult your GP: Discuss your liver condition, weight, and metabolic health. Request referral to appropriate specialists if needed
Liver assessment: Ensure proper diagnosis through blood tests, FIB-4 calculation, and if indicated, imaging (ultrasound or FibroScan) or ELF testing
Specialist review: Hepatology or endocrinology input may be needed to assess suitability
Clinical trials: Some patients may be eligible for research studies examining GLP-1 agonists in NAFLD/NASH
Patients should be aware that even when prescribed, GLP-1 agonists require ongoing monitoring, lifestyle modification remains essential, and treatment should be reviewed regularly to assess response and tolerability. If you experience severe abdominal pain, persistent nausea or vomiting, or signs of pancreatitis whilst taking these medications, contact your GP or seek urgent medical attention. Report any suspected side effects via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
GLP-1 receptor agonists are not licensed specifically for fatty liver disease in the UK. NHS access is available if you have concurrent type 2 diabetes or meet BMI criteria for weight management services (typically BMI ≥35 kg/m² or ≥30 kg/m² with weight-related comorbidities). Specialist hepatology referral may be considered in exceptional circumstances for patients with biopsy-proven NASH and significant fibrosis.
Liraglutide has the most robust evidence specifically in NASH, with the LEAN trial showing 39% NASH resolution compared to 9% with placebo. Semaglutide has also demonstrated impressive results, with 59% NASH resolution in a phase 2 trial and substantial reductions in hepatic fat content measured by MRI.
Weight loss of 5-7% can significantly improve liver steatosis, whilst losses exceeding 10% may lead to improvements in inflammation and fibrosis. GLP-1 receptor agonists typically achieve 5-15% body weight reduction depending on the specific agent and dose, with semaglutide generally producing the greatest weight loss.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.