GLP-1 receptor agonists—including semaglutide, dulaglutide, and liraglutide—are widely prescribed for type 2 diabetes and weight management. Whilst these medications offer substantial metabolic benefits, emerging evidence suggests a potential association between GLP-1 receptor agonist use and increased gallbladder disease risk. Clinical trials and post-marketing data indicate a modest elevation in cholelithiasis and cholecystitis rates, particularly with rapid weight loss and reduced gallbladder motility. Understanding this risk, recognising warning symptoms, and implementing preventive strategies are essential for patients and clinicians. This article examines the evidence, identifies at-risk groups, and provides practical guidance on minimising complications whilst maintaining therapeutic benefits.
Quick Answer: GLP-1 receptor agonists are associated with a modest but statistically significant increase in gallbladder disease risk, including gallstones and cholecystitis, affecting approximately 1–3% of users.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereGlucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications used to manage type 2 diabetes mellitus and, in specific formulations, obesity. These medicines work by mimicking the action of naturally occurring GLP-1, a hormone produced in the intestine that plays a crucial role in glucose regulation and appetite control.
The mechanism of action involves several physiological effects. GLP-1 receptor agonists stimulate insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning they only promote insulin release when blood glucose levels are elevated. Simultaneously, they suppress glucagon secretion, reducing hepatic glucose production. These medications also slow gastric emptying, which helps moderate post-meal blood glucose spikes and promotes satiety, leading to reduced calorie intake and weight loss.
Commonly prescribed GLP-1 receptor agonists available in the UK include:
Semaglutide (Ozempic, Rybelsus - licensed for type 2 diabetes; Wegovy - licensed for weight management)
Dulaglutide (Trulicity - for type 2 diabetes)
Liraglutide (Victoza - for type 2 diabetes; Saxenda - for weight management)
Exenatide (Byetta, Bydureon - for type 2 diabetes)
Lixisenatide (Lyxumia - for type 2 diabetes)
These medications are administered either as subcutaneous injections (weekly or daily, depending on the formulation) or as oral tablets (Rybelsus). NICE guideline NG28 recommends GLP-1 receptor agonists for adults with type 2 diabetes who have inadequate glycaemic control despite optimal management with other glucose-lowering therapies and have a BMI ≥30 kg/m². For weight management, NICE technology appraisals TA875 (semaglutide 2.4mg) and TA664 (liraglutide 3mg) provide specific eligibility criteria within NHS services.
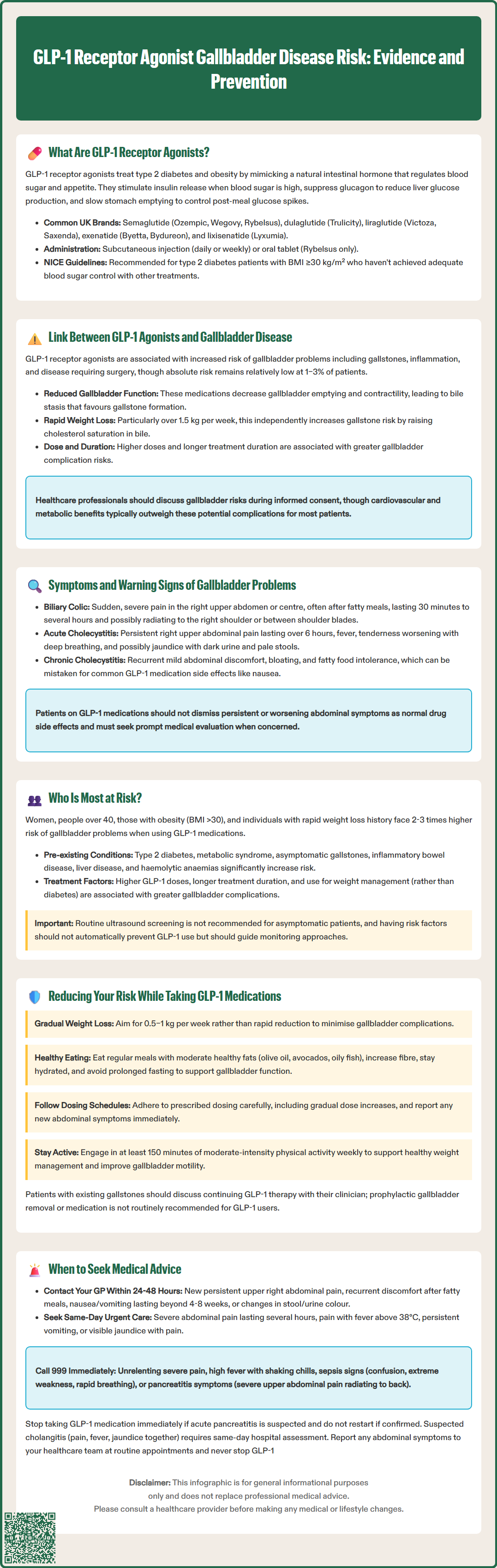
Emerging evidence from clinical trials and post-marketing surveillance has identified a potential association between GLP-1 receptor agonist use and increased risk of gallbladder-related complications, including cholelithiasis (gallstones), cholecystitis (gallbladder inflammation), and biliary disease requiring surgical intervention. However, it is important to note that establishing a definitive causal relationship remains complex, as the patient populations using these medications often have pre-existing risk factors for gallbladder disease.
The proposed mechanism linking GLP-1 agonists to gallbladder problems primarily involves reduced gallbladder motility and bile stasis. GLP-1 receptor agonists reduce cholecystokinin release, which decreases gallbladder contractility and emptying. Additionally, the significant weight loss induced by these medications—particularly losses exceeding 1.5 kg per week—is a well-established risk factor for gallstone formation, as it can lead to increased cholesterol saturation in bile. The combination of reduced gallbladder emptying and rapid weight loss creates conditions favouring gallstone development.
Large-scale studies, including the STEP trials for semaglutide and real-world data analyses, have reported gallbladder-related adverse events in approximately 1–3% of patients, compared with lower rates in control groups. A 2022 meta-analysis published in JAMA Internal Medicine suggested a modest but statistically significant increase in cholelithiasis risk amongst GLP-1 agonist users, with higher risks observed at higher doses and with longer treatment duration. The Medicines and Healthcare products Regulatory Agency (MHRA) continues to monitor these reports, and product information for GLP-1 receptor agonists now includes gallbladder disorders as recognised adverse reactions in their Summary of Product Characteristics (SmPCs).
It is crucial to emphasise that whilst there is an observed association, the absolute risk remains relatively low, and for most patients, the cardiovascular and metabolic benefits of these medications outweigh the potential gallbladder risks. Healthcare professionals should discuss this risk as part of informed consent when initiating treatment.
Recognising the symptoms of gallbladder disease is essential for patients taking GLP-1 receptor agonists, as early identification can prevent serious complications. Biliary colic—the hallmark symptom of gallstones—typically presents as sudden, severe pain in the right upper quadrant or epigastrium (upper central abdomen). This pain often occurs after consuming fatty meals and may radiate to the right shoulder or between the shoulder blades. Episodes usually last from 30 minutes to several hours and may be accompanied by nausea and vomiting.
Acute cholecystitis represents a more serious complication when a gallstone obstructs the cystic duct, leading to gallbladder inflammation. Key features include:
Persistent right upper quadrant pain lasting more than six hours
Fever and systemic signs of infection
Tenderness in the right upper abdomen that worsens during deep breathing
Jaundice (yellowing of skin and eyes) if bile duct obstruction occurs
Dark urine and pale stools
Loss of appetite and general malaise
Some patients may experience chronic cholecystitis, characterised by recurrent episodes of milder abdominal discomfort, bloating, and intolerance to fatty foods. These symptoms can be non-specific and may be mistakenly attributed to gastrointestinal side effects commonly associated with GLP-1 agonists, such as nausea or dyspepsia.
Serious complications requiring urgent medical attention include ascending cholangitis (bile duct infection, characterised by Charcot's triad: right upper quadrant pain, fever, and jaundice), gallstone pancreatitis, or gallbladder perforation. Warning signs include high fever with rigors, severe unremitting pain, jaundice, confusion, or signs of sepsis. Patients should be advised not to dismiss persistent or worsening abdominal symptoms as routine medication side effects and to seek prompt medical evaluation if concerned.
Whilst GLP-1 receptor agonists may increase gallbladder disease risk in the general population using these medications, certain patient groups face heightened susceptibility due to pre-existing risk factors. Understanding these risk stratifications helps clinicians identify individuals who may benefit from enhanced monitoring or preventive strategies.
Demographic and constitutional risk factors include:
Female sex: Women are two to three times more likely to develop gallstones than men, particularly during reproductive years
Age over 40 years: Gallstone prevalence increases significantly with advancing age
Obesity: Individuals with BMI >30 kg/m² have substantially elevated baseline risk
Rapid weight loss history: Previous episodes of quick weight reduction
Ethnicity: Risk varies across different populations, with some ethnic groups showing higher predisposition
Medical conditions that compound gallbladder disease risk include:
Type 2 diabetes mellitus: Independent risk factor for gallstone formation
Metabolic syndrome: Clustering of cardiovascular risk factors
Pre-existing gallstones: Asymptomatic cholelithiasis may become symptomatic
Inflammatory bowel disease, particularly Crohn's disease affecting the terminal ileum
Cirrhosis or other chronic liver conditions
Haemolytic anaemias: Conditions causing increased bilirubin production
Medication and lifestyle factors include prolonged fasting, very low-calorie diets, total parenteral nutrition, and certain medications such as fibrates or oestrogen therapy. Patients with family history of gallbladder disease also warrant closer attention.
Risk appears greater with higher GLP-1 doses and longer treatment duration, and may be more pronounced in those using these medications for weight management rather than diabetes alone, as shown in the 2022 JAMA Internal Medicine meta-analysis.
For individuals with multiple risk factors, clinicians should engage in shared decision-making, weighing the substantial metabolic benefits of GLP-1 therapy against potential gallbladder complications. Routine baseline ultrasound screening is not recommended in asymptomatic individuals. The presence of risk factors should not automatically preclude GLP-1 agonist use but should inform monitoring strategies and patient education.
Whilst the association between GLP-1 receptor agonists and gallbladder disease cannot be entirely eliminated, several evidence-based strategies may help minimise risk whilst maintaining the therapeutic benefits of these medications.
Gradual weight loss represents the most important modifiable factor. Aim for steady, sustainable weight reduction of approximately 0.5–1 kg per week rather than rapid losses. This measured approach allows the body to adapt metabolically and reduces the likelihood of bile supersaturation with cholesterol. Work with your healthcare team to establish realistic weight loss targets that balance efficacy with safety.
Dietary modifications can support gallbladder health:
Maintain regular meal patterns: Avoid prolonged fasting, which reduces gallbladder emptying
Include moderate healthy fats: Complete fat avoidance may paradoxically reduce gallbladder contractility; incorporate sources like olive oil, avocados, and oily fish
Increase fibre intake: Soluble fibre may help regulate bile acid metabolism
Stay well hydrated: Adequate fluid intake supports bile flow
Limit refined carbohydrates: High glycaemic foods may adversely affect bile composition
Medication adherence and monitoring are crucial. Follow your prescribed dosing schedule carefully, including the recommended gradual dose escalation outlined in the product information. Erratic use may contribute to metabolic fluctuations. Attend all scheduled follow-up appointments, which typically include assessment of weight loss velocity, glycaemic control, and adverse effects. Report any new abdominal symptoms promptly rather than waiting for routine appointments.
Physical activity supports healthy weight management and may improve gallbladder motility. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity activity weekly for adults.
For patients with pre-existing asymptomatic gallstones, discuss the risks and benefits of continuing GLP-1 therapy with your clinician. Prophylactic cholecystectomy and ursodeoxycholic acid are not routinely recommended for GLP-1 users and should only be considered under specialist guidance for specific clinical circumstances unrelated to GLP-1 therapy. If you experience any suspected adverse effects, report them via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Knowing when to contact healthcare services is essential for patients taking GLP-1 receptor agonists, as timely intervention can prevent serious complications and ensure appropriate management of potential gallbladder disease.
Contact your GP or diabetes specialist nurse within 24–48 hours if you experience:
New or persistent right upper abdominal pain, particularly if it differs from typical GLP-1 side effects
Recurrent episodes of abdominal discomfort after eating, especially fatty meals
Unexplained nausea and vomiting that persists beyond the initial medication adjustment period (most GLP-1 gastrointestinal effects improve within 4–8 weeks)
Changes in stool colour or urine darkening
Mild jaundice or yellowing of the eyes
Seek same-day urgent assessment (via GP urgent appointment or NHS 111) for:
Severe abdominal pain lasting more than a few hours
Pain accompanied by fever (temperature >38°C)
Persistent vomiting preventing oral intake
Visible jaundice with abdominal pain
Call 999 or attend A&E immediately if you develop:
Severe, unrelenting abdominal pain unresponsive to simple analgesia
High fever with rigors (shaking chills) and abdominal pain
Signs of sepsis: confusion, extreme weakness, rapid breathing, or feeling severely unwell
Severe jaundice with confusion or altered consciousness
Symptoms suggesting pancreatitis: severe upper abdominal pain radiating to the back
Important: If acute pancreatitis is suspected, stop taking your GLP-1 receptor agonist immediately and seek urgent medical care. If pancreatitis is confirmed, the medication should not be restarted.
Suspected cholangitis (combination of right upper quadrant pain, fever, and jaundice) requires same-day hospital assessment.
For routine monitoring, inform your healthcare team at regular appointments about any abdominal symptoms, even if mild or intermittent. Do not discontinue your GLP-1 medication without medical advice, as abrupt cessation may affect glycaemic control. Your clinician can arrange appropriate investigations, typically starting with liver function tests and abdominal ultrasound, which is the first-line imaging modality for suspected gallbladder disease. If gallbladder pathology is confirmed, your healthcare team will discuss management options, which may include conservative management, medication adjustment, or surgical referral depending on severity and individual circumstances.
Yes, GLP-1 receptor agonists are associated with a modest increase in gallstone risk, affecting approximately 1–3% of users. The mechanism involves reduced gallbladder motility and rapid weight loss, both of which promote gallstone formation.
Key warning signs include sudden severe right upper abdominal pain (especially after fatty meals), fever, jaundice, dark urine, pale stools, and persistent nausea or vomiting. Seek urgent medical attention if symptoms are severe or accompanied by fever.
Do not stop your GLP-1 medication without medical advice, as this may affect your diabetes control. If you experience concerning symptoms, contact your GP or diabetes team promptly for assessment and guidance on whether medication adjustment is needed.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.