
Ozempic (semaglutide) is a GLP-1 receptor agonist widely prescribed in the UK for type 2 diabetes and weight management, but gastrointestinal side effects such as nausea, bloating, and altered bowel habits are very common. Many patients seek complementary strategies to manage these symptoms whilst continuing treatment. Probiotics—live microorganisms that support gut health—are increasingly considered as a potential adjunct to ease digestive discomfort. This article examines the evidence for using probiotics alongside Ozempic, explores which strains may be most relevant, and provides guidance on safe, informed use within the context of UK clinical practice and regulatory standards.
Quick Answer: There is no single 'best' probiotic specifically proven for Ozempic side effects, but strains such as Lactobacillus rhamnosus GG and Bifidobacterium lactis BB-12 may offer symptomatic relief for gastrointestinal discomfort.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereOzempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus and, at higher doses (as Wegovy), for weight management. The medication works by mimicking the action of naturally occurring GLP-1, a hormone released from the intestine in response to food intake. Semaglutide enhances insulin secretion in a glucose-dependent manner, suppresses glucagon release, and slows gastric emptying—the rate at which food leaves the stomach and enters the small intestine.
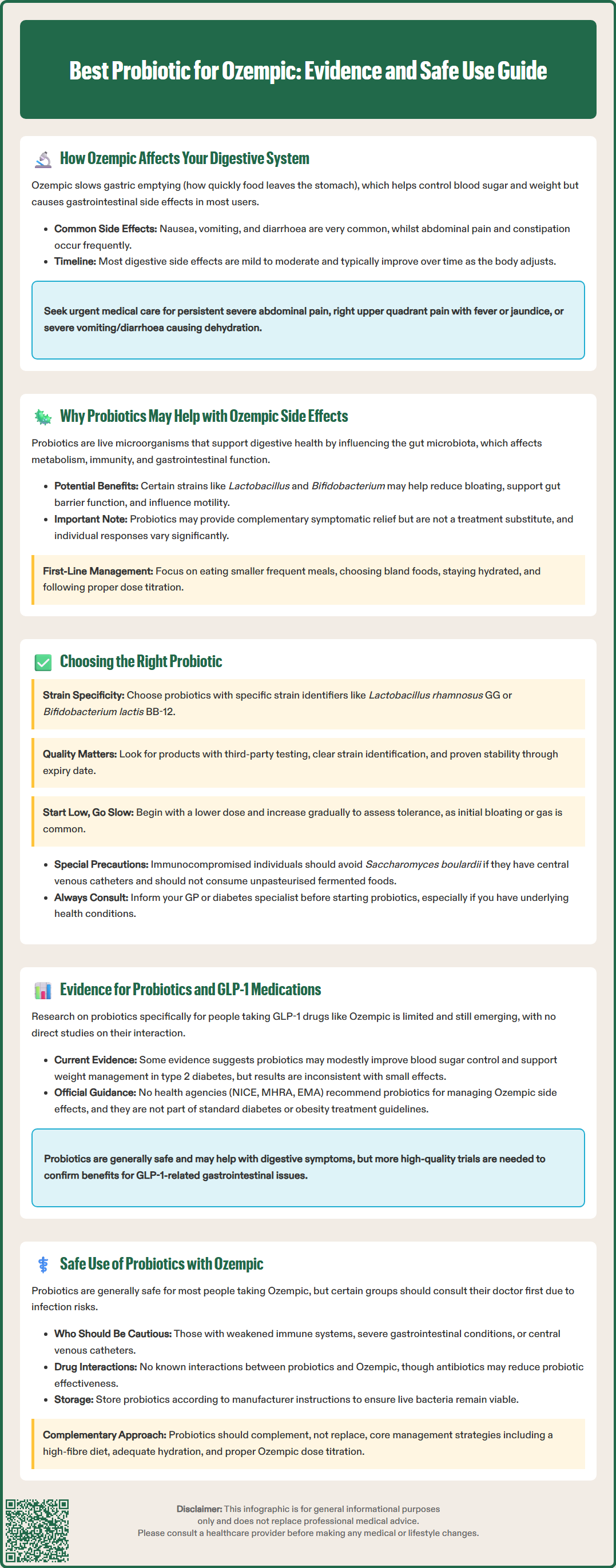
This slowing of gastric emptying contributes to Ozempic's therapeutic effect, alongside its primary action on appetite and satiety centres in the brain. These mechanisms help improve glycaemic control and promote weight reduction. However, these effects also underlie the most commonly reported adverse effects, which are predominantly gastrointestinal in nature. According to the MHRA-approved Summary of Product Characteristics (SmPC), nausea, vomiting, and diarrhoea are very common side effects with Ozempic, while abdominal pain and constipation are common, particularly during dose initiation and escalation. At the higher Wegovy doses, constipation is very common.
The effects on gastric motility can lead to feelings of fullness, bloating, and discomfort. Some patients experience alterations in bowel habit, ranging from loose stools to constipation. These effects are generally mild to moderate and tend to diminish over time as the body adapts to the medication. However, for a subset of patients, gastrointestinal symptoms can be persistent and may affect treatment adherence.
It's important to note that semaglutide carries warnings about more serious digestive system risks, including pancreatitis and gallbladder disease. Persistent severe abdominal pain (with or without vomiting) or right upper quadrant pain with fever or jaundice requires urgent medical assessment. Severe vomiting or diarrhoea can also lead to dehydration and potential kidney problems, particularly in vulnerable patients. Caution is advised in those with severe gastrointestinal disease, including gastroparesis.
Probiotics are live microorganisms that, when administered in adequate amounts, confer a health benefit on the host. They are thought to support digestive health by modulating the composition and function of the gut microbiota—the complex community of bacteria, fungi, and other microbes residing in the gastrointestinal tract. Emerging research suggests that the gut microbiome plays a role in metabolic health, immune function, and gastrointestinal motility.
Patients taking Ozempic may experience disruption to normal digestive processes due to delayed gastric emptying and altered gut transit time. This can potentially affect the balance of gut bacteria, though there is no official link definitively established between GLP-1 receptor agonists and dysbiosis (microbial imbalance). Probiotics might offer symptomatic relief for some of the gastrointestinal side effects associated with Ozempic, though evidence specifically for GLP-1-related symptoms is limited and indirect.
Certain probiotic strains, such as Lactobacillus and Bifidobacterium species, have been studied for their effects on gastrointestinal symptoms in various contexts. They may help by:
Supporting gut barrier function and potentially reducing inflammation
Influencing gut motility and transit time
Contributing to short-chain fatty acid production that may support intestinal health
Potentially reducing bloating and abdominal discomfort in some individuals
First-line approaches to managing Ozempic-related digestive symptoms typically include non-pharmacological measures such as eating smaller, more frequent meals, choosing bland foods, staying well-hydrated, and following healthcare provider advice on dose titration. Probiotics are not a treatment for the underlying condition or a substitute for prescribed medication, but may serve as a complementary approach for some individuals. It is important to note that responses vary considerably, and not all patients will experience benefit from probiotic supplementation.
Selecting an appropriate probiotic requires consideration of several factors, including strain specificity, colony-forming units (CFUs), product quality, and individual tolerance. Not all probiotics are equivalent; different bacterial strains have distinct effects, and evidence supporting one strain does not necessarily apply to another.
For gastrointestinal symptoms such as those experienced with Ozempic, the following strains have some evidence base in managing digestive discomfort in general (though not specifically for GLP-1 medication side effects):
Lactobacillus acidophilus NCFM and Lactobacillus rhamnosus GG: May help with some types of digestive discomfort
Bifidobacterium lactis BB-12 and Bifidobacterium longum 35624: Associated with improved bowel regularity in some studies
Saccharomyces boulardii CNCM I-745: A probiotic yeast that may help with certain types of diarrhoea, though evidence is primarily in antibiotic-associated and infectious diarrhoea
When choosing a probiotic product, consider:
Products listing specific strain identifiers (as above) with evidence for defined indications
Following manufacturer-recommended dosing, as effective doses vary by strain and condition
Products with evidence of stability and viability through to the expiry date
Third-party testing or certification where available, ensuring quality and accurate labelling
It is advisable to start with a lower dose and increase gradually to assess tolerance. Some individuals may experience initial bloating or gas as the gut microbiota adjusts. Probiotics are available as capsules, powders, and fermented foods (such as live yoghurt, kefir, and sauerkraut), though supplemental forms provide more standardised dosing.
Caution is warranted with Saccharomyces boulardii in those with central venous catheters or critical illness due to rare risks of fungemia. Immunocompromised individuals should avoid unpasteurised fermented foods. Always inform your GP or diabetes specialist nurse if you are considering probiotic supplementation, particularly if you have underlying health conditions.
The evidence base specifically examining probiotics in patients taking GLP-1 receptor agonists such as Ozempic remains limited and emerging. Most research on probiotics and metabolic health has focused on their role in weight management, glycaemic control, and general gastrointestinal symptoms, rather than their interaction with GLP-1 therapies directly.
Some observational and mechanistic studies suggest that the gut microbiome may influence the efficacy and tolerability of metabolic therapies. For instance, certain gut bacteria are involved in the metabolism of bile acids and the production of metabolites that affect glucose homeostasis and satiety signalling. Systematic reviews and meta-analyses have found that probiotic supplementation may modestly improve glycaemic parameters and support weight management in people with type 2 diabetes, though results are inconsistent across studies, with generally small effect sizes.
There is no official recommendation from regulatory bodies such as NICE, the MHRA, or the European Medicines Agency (EMA) supporting probiotics specifically for managing Ozempic-related side effects. Current NICE guidance on type 2 diabetes (NG28) and obesity management (TA875) does not include probiotics as part of standard care pathways for patients on GLP-1 receptor agonists.
However, probiotics are generally recognised as safe for most individuals, and their use for symptomatic gastrointestinal relief is supported by a broader evidence base in functional gastrointestinal disorders. Further high-quality randomised controlled trials are needed to clarify whether probiotics can meaningfully reduce GLP-1-associated gastrointestinal side effects and whether specific strains or formulations are superior.
Patients should be aware that while probiotics may offer symptomatic benefit, they do not replace the need for appropriate medical management of diabetes or obesity, nor do they mitigate the need for lifestyle interventions such as diet and physical activity. Any use should be considered adjunctive to standard care, and patients should continue to monitor their symptoms and discuss their management with healthcare professionals.
Probiotics are generally considered safe for the majority of individuals, including those taking Ozempic. They are classified as food supplements in the UK and are not subject to the same regulatory scrutiny as medicines. However, certain precautions and considerations are important to ensure safe and effective use.
Key safety considerations include:
Immunocompromised patients: Those with weakened immune systems (e.g., due to chemotherapy, HIV, or immunosuppressive medications) should consult their healthcare provider before starting probiotics, as there is a small risk of systemic infection from live bacteria.
Severe gastrointestinal conditions: Individuals with conditions such as short bowel syndrome, central venous catheters, or severe acute pancreatitis should seek medical advice before using probiotics. Semaglutide is not recommended in severe gastroparesis or inflammatory bowel disease without specialist advice.
Drug interactions: There is no known pharmacokinetic interaction between probiotics and Ozempic. However, if you are taking antibiotics, these may reduce the efficacy of probiotics, and timing of administration may need adjustment.
Quality and storage: Probiotics should be stored according to manufacturer instructions (some require refrigeration) to maintain viability. Choose reputable brands to ensure product integrity.
When to seek urgent medical care:
If you experience severe, persistent upper abdominal pain (especially if radiating to the back), with or without vomiting – this could indicate pancreatitis and requires immediate assessment
If you develop right upper quadrant pain, fever, or yellowing of the skin/eyes – possible signs of gallbladder disease
If you have persistent vomiting or diarrhoea leading to signs of dehydration (reduced urination, dizziness, extreme thirst)
When to contact your GP or diabetes care team:
If gastrointestinal symptoms worsen or do not improve after several weeks on Ozempic
If you have concerns about the suitability of probiotics given your medical history
If you experience any new or worsening symptoms while taking probiotics
Probiotics should be viewed as a complementary measure rather than a primary treatment. Maintaining a balanced diet rich in fibre, staying well hydrated, and following your healthcare provider's advice on dose titration of Ozempic remain the cornerstones of managing side effects effectively.
If you experience side effects that you think may be related to Ozempic, you can report them through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk), which helps monitor the safety of medicines in the UK.
Probiotics may offer symptomatic relief for some gastrointestinal side effects such as bloating and altered bowel habits, though evidence specifically for GLP-1 receptor agonists like Ozempic is limited. They should be considered a complementary measure alongside standard care, not a replacement for medical management.
Strains such as Lactobacillus rhamnosus GG, Bifidobacterium lactis BB-12, and Saccharomyces boulardii have some evidence for managing general digestive symptoms, though no strain is specifically proven for Ozempic-related side effects. Choosing products with defined strain identifiers and third-party testing is advisable.
Probiotics are generally safe for most individuals taking Ozempic, with no known drug interactions. However, immunocompromised patients and those with severe gastrointestinal conditions should consult their healthcare provider before starting probiotics.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.