LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
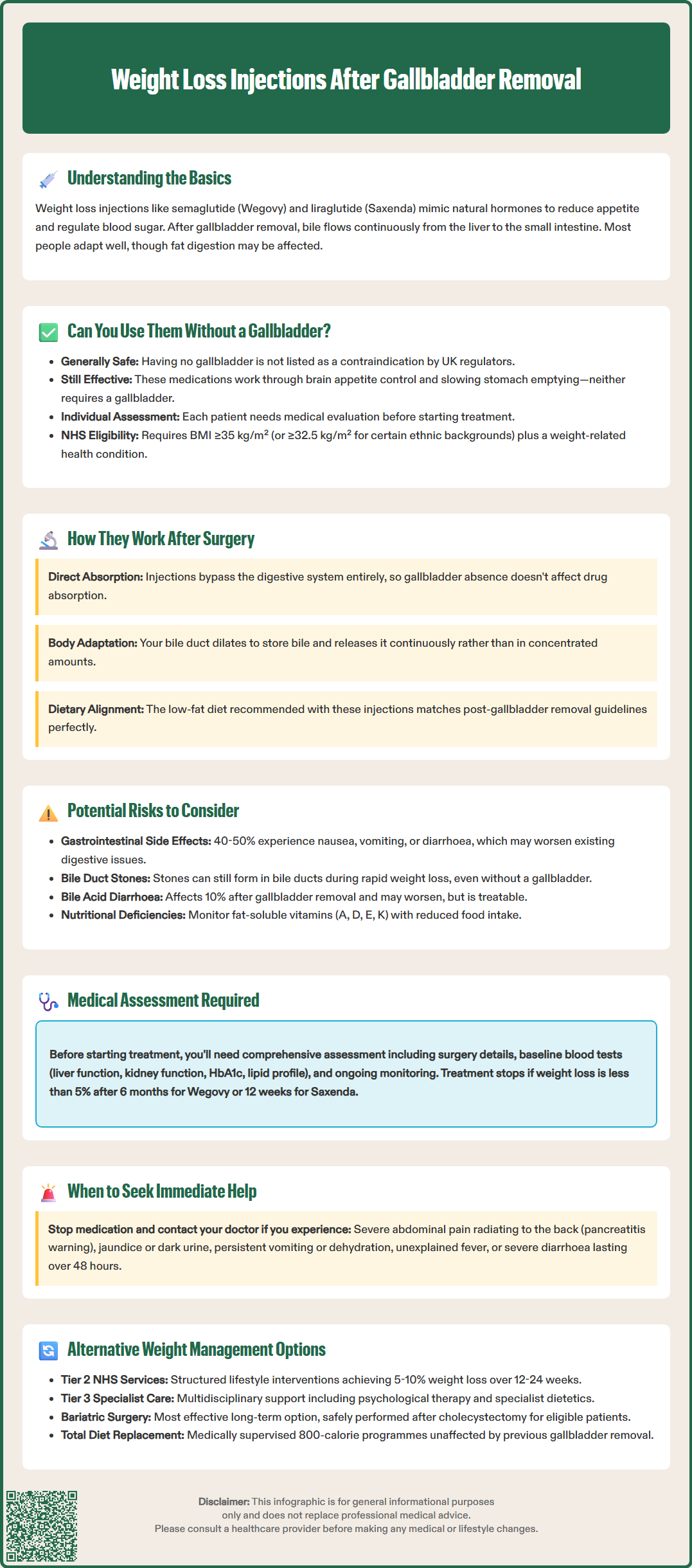
Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), are increasingly prescribed for weight management in the UK. Many patients who have undergone cholecystectomy (gallbladder removal) wonder whether these medications remain safe and effective for them. Having no gallbladder is not listed as a contraindication for GLP-1 receptor agonists, and these medications can generally be used after gallbladder surgery. However, individual assessment is essential, as gastrointestinal side effects may overlap with post-surgical digestive changes. This article examines the safety, efficacy, and considerations for using weight loss injections after cholecystectomy, alongside alternative weight management options available through the NHS.
Quick Answer: Yes, you can generally have weight loss injections after gallbladder removal, as cholecystectomy is not a contraindication for GLP-1 receptor agonists.
Weight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly prescribed for weight management in the UK. These medications work by mimicking natural hormones that regulate appetite and blood sugar levels, helping patients achieve significant weight reduction when combined with lifestyle modifications.
Cholecystectomy, or gallbladder removal, is one of the most common surgical procedures performed in the UK, with approximately 70,000 operations conducted annually through the NHS. The gallbladder stores bile produced by the liver, which aids in fat digestion. After removal, bile flows continuously from the liver directly into the small intestine, rather than being stored and released in response to meals. Most people adapt well to this change, though some experience altered fat digestion.
Obesity and gallstone disease often share common risk factors including metabolic syndrome, insulin resistance, and dietary patterns. This explains why some patients who have undergone cholecystectomy may also struggle with weight management and consider weight loss injections.
It's important to note that GLP-1 receptor agonists are associated with an increased risk of gallbladder and biliary disorders, including cholelithiasis (gallstones) and cholecystitis (gallbladder inflammation), as documented in their Summary of Product Characteristics. Even after gallbladder removal, this risk remains relevant as stones can still form in the bile ducts (choledocholithiasis).
Understanding the relationship between these treatments requires examining how weight loss injections function, how the body adapts after gallbladder removal, and whether the absence of a gallbladder affects the safety or efficacy of these medications. Current evidence suggests no absolute contraindication, but individual assessment remains essential.
Yes, you can generally have weight loss injections after gallbladder removal. Having undergone cholecystectomy is not listed as a contraindication for GLP-1 receptor agonists in the Summary of Product Characteristics (SmPC) approved by the Medicines and Healthcare products Regulatory Agency (MHRA). The absence of a gallbladder does not fundamentally prevent these medications from working or create an automatic safety concern.
The mechanism of action of GLP-1 receptor agonists does not depend on gallbladder function. These medications work primarily by:
Activating GLP-1 receptors in the brain to reduce appetite and increase satiety
Slowing gastric emptying to prolong feelings of fullness
Improving insulin secretion and reducing glucagon release
Modulating reward pathways related to food intake
None of these mechanisms require an intact gallbladder to function effectively. The liver continues to produce bile after cholecystectomy, and the digestive system adapts to the continuous flow of bile into the intestine. This adaptation typically occurs within weeks to months following surgery.
NHS availability of these medications is subject to specific criteria. NICE Technology Appraisal (TA875) recommends semaglutide (Wegovy) only for adults with at least one weight-related comorbidity and a BMI ≥35 kg/m² (or ≥32.5 kg/m² for people from South Asian, Chinese, other Asian, Middle Eastern, Black African or African-Caribbean backgrounds). Treatment should be provided within specialist weight management services and is usually limited to 2 years. Similar restrictions apply to liraglutide (Saxenda) under NICE TA664.
It's important to note that these NHS commissioning criteria are more restrictive than the licensed indications, which permit use at lower BMI thresholds. Your healthcare provider will consider your complete medical history, current health status, and any post-cholecystectomy complications when determining suitability.
The efficacy of weight loss injections is not known to be reduced by previous gallbladder removal. While clinical trials of GLP-1 receptor agonists have included participants with various medical histories, there are no specific published analyses focusing on post-cholecystectomy patients. However, there is no physiological reason to expect reduced effectiveness in this population. The medications continue to suppress appetite, increase satiety, and promote weight loss through their central and peripheral mechanisms.
After cholecystectomy, the body undergoes several digestive adaptations. The common bile duct may dilate slightly to accommodate increased bile storage, and bile acids flow continuously into the duodenum rather than being released in concentrated amounts during meals. This can initially affect fat digestion, with some patients experiencing loose stools or diarrhoea, particularly after fatty meals. Over time, most individuals adapt, and these symptoms typically resolve.
When GLP-1 receptor agonists are introduced after gallbladder removal, their effect of slowing gastric emptying may affect digestive patterns. By reducing the rate at which food enters the small intestine, these medications could potentially influence how the body manages the continuous flow of bile. However, this interaction has not been specifically studied in clinical trials.
Absorption of the medication itself is not affected by gallbladder absence. GLP-1 receptor agonists are administered via subcutaneous injection and absorbed directly into the bloodstream, bypassing the digestive system entirely. This route of administration ensures consistent drug levels regardless of gallbladder status or digestive function.
Patients should be aware that the dietary modifications recommended alongside weight loss injections—including reduced calorie intake and lower fat consumption—align well with post-cholecystectomy dietary advice, potentially making adherence easier and reducing gastrointestinal side effects.
It's important to remain vigilant for symptoms of biliary complications such as jaundice (yellowing of skin/eyes), dark urine, or pale stools, as GLP-1 receptor agonists can increase the risk of biliary events even in those without a gallbladder.
Whilst weight loss injections can be used after gallbladder removal, several important considerations warrant attention. The most common side effects of GLP-1 receptor agonists are gastrointestinal, including nausea, vomiting, diarrhoea, constipation, and abdominal discomfort. These effects occur in up to 40–50% of patients and are typically most pronounced during dose escalation.
For individuals who have undergone cholecystectomy, particularly those who experience post-cholecystectomy syndrome—characterised by ongoing digestive symptoms—the addition of GLP-1-related gastrointestinal effects may be more troublesome. Symptoms such as diarrhoea or abdominal cramping might be difficult to distinguish from medication side effects versus post-surgical digestive changes. This overlap can complicate management and may require closer monitoring.
Pancreatitis is an uncommon but serious adverse effect associated with GLP-1 receptor agonists (occurring in approximately 0.1–0.2% of patients). According to MHRA-approved SmPCs, if pancreatitis is suspected, the medication should be discontinued immediately and not restarted if pancreatitis is confirmed. Patients should seek immediate medical attention if they experience severe, persistent abdominal pain, particularly if radiating to the back, accompanied by nausea and vomiting.
Biliary complications remain relevant even after gallbladder removal. GLP-1 receptor agonists are associated with an increased risk of gallstones and biliary events. While the gallbladder is gone, stones can still form in the bile ducts, potentially causing cholangitis or biliary obstruction. Rapid weight loss itself also increases the risk of gallstone formation.
Nutritional considerations also merit attention. Some patients may experience reduced absorption of fat-soluble vitamins (A, D, E, and K) after cholecystectomy, though clinically significant deficiencies are uncommon unless there is persistent steatorrhoea. When combined with the reduced food intake associated with GLP-1 therapy, monitoring nutritional status may be appropriate in some cases.
Additionally, approximately 10% of post-cholecystectomy patients develop bile acid diarrhoea, which might be exacerbated by the gastrointestinal effects of weight loss injections. This condition can usually be managed with bile acid sequestrants such as colestyramine or colesevelam if necessary.
Before initiating weight loss injections after gallbladder removal, a comprehensive medical assessment is essential. Your GP or specialist weight management service will review your complete medical history, including:
The reason for cholecystectomy and time since surgery
Any ongoing post-surgical symptoms or complications
Current medications and potential drug interactions
Presence of other gastrointestinal conditions
Liver function and metabolic health status
History of pancreatitis or pancreatic disease
Pregnancy status or plans (GLP-1 RAs are contraindicated in pregnancy and breastfeeding)
Baseline investigations typically include blood tests to assess liver function, kidney function, HbA1c (for diabetes screening), and lipid profile. These establish a reference point for monitoring treatment effects and safety. Some clinicians may also check vitamin D levels and other nutritional markers if there are specific concerns about malabsorption.
Ongoing monitoring follows product-specific guidance and NICE recommendations:
For semaglutide (Wegovy): Assess at 6 months after reaching maintenance dose; discontinue if weight loss is less than 5% of initial body weight
For liraglutide (Saxenda): Evaluate after 12 weeks at the full dose (3.0 mg daily); discontinue if weight loss is less than 5%
Regular weight measurements and BMI calculations
Monitoring for adverse effects, particularly gastrointestinal symptoms
Blood pressure and cardiovascular risk factor assessment
Periodic blood tests to monitor metabolic parameters
For patients with diabetes who are taking insulin or sulfonylureas, doses of these medications may need to be reduced when starting GLP-1 receptor agonists to prevent hypoglycaemia.
Under NICE TA875, semaglutide (Wegovy) treatment on the NHS is usually limited to 2 years within specialist weight management services.
Patients should stop the medication and contact their healthcare provider immediately if they experience:
Severe or persistent abdominal pain (especially if radiating to the back), which could indicate pancreatitis
Persistent vomiting preventing adequate fluid intake
Signs of dehydration (dark urine, dizziness, reduced urination)
Yellowing of skin or eyes (jaundice) or pale stools
Unexplained fever
Severe diarrhoea lasting more than 48 hours
Treatment continuation is reviewed regularly, with decisions based on efficacy, tolerability, and ongoing clinical need. If weight loss targets are not met or side effects become problematic, alternative approaches should be considered.
For individuals who cannot tolerate weight loss injections after cholecystectomy, or for whom they are unsuitable, several evidence-based alternatives exist within NHS pathways.
Tier 2 weight management services provide structured lifestyle interventions including dietary counselling, physical activity programmes, and behavioural support. These services, available through GP referral, offer group or individual sessions over 12–24 weeks. They focus on sustainable behaviour change without medication, making them suitable for all patients regardless of surgical history. Evidence shows that intensive lifestyle interventions can achieve 5–10% weight loss in motivated individuals.
Orlistat (Xenical, Alli) represents an alternative pharmacological option. This medication works by inhibiting pancreatic lipase, reducing dietary fat absorption by approximately 30%. It is contraindicated in chronic malabsorption syndromes and cholestasis. After cholecystectomy, orlistat may exacerbate fat malabsorption and increase gastrointestinal side effects such as oily stools and faecal urgency. If prescribed, patients should follow a low-fat diet and take any fat-soluble vitamin supplements at least 2 hours before or after orlistat.
Tier 3 specialist weight management services provide multidisciplinary assessment and intervention for patients with complex obesity. These services, available in most NHS regions (though access varies locally), offer intensive support including psychological therapy, specialist dietetic input, and consideration for bariatric surgery referral when appropriate.
Bariatric surgery remains the most effective long-term weight loss intervention for eligible patients. Procedures such as gastric bypass or sleeve gastrectomy can be performed safely after cholecystectomy. NICE recommends considering bariatric surgery for patients with BMI ≥40 kg/m² (or ≥35 kg/m² with comorbidities) who have not achieved adequate weight loss with non-surgical methods. It may also be considered for people with BMI 30–34.9 kg/m² who have recent-onset type 2 diabetes.
Total diet replacement programmes (providing approximately 800 calories daily) offer another option. These programmes, delivered under healthcare supervision, can achieve rapid initial weight loss and are particularly useful for managing type 2 diabetes. NICE guidance supports their use as part of NHS services for selected patients. They require careful monitoring but do not interact with gallbladder status.
Ultimately, the choice of weight management approach should be individualised, considering your medical history, preferences, and circumstances, in partnership with your healthcare team.
Yes, weight loss injections such as semaglutide and liraglutide are generally safe after cholecystectomy, as gallbladder removal is not a contraindication. However, individual assessment is necessary, particularly if you experience ongoing digestive symptoms, as gastrointestinal side effects may be more troublesome.
Yes, GLP-1 receptor agonists remain effective after gallbladder removal. Their mechanism of action—reducing appetite, increasing satiety, and slowing gastric emptying—does not depend on gallbladder function, and the medications are absorbed directly into the bloodstream via subcutaneous injection.
Risks include gastrointestinal side effects that may overlap with post-surgical symptoms, increased risk of bile duct stones despite gallbladder absence, and rare but serious complications such as pancreatitis. Close monitoring and prompt reporting of severe abdominal pain, jaundice, or persistent vomiting are essential.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.