Tirzepatide (Mounjaro, Zepbound) is a dual GIP and GLP-1 receptor agonist licensed in the UK for type 2 diabetes and weight management. Many patients wonder whether tirzepatide stops working over time, particularly when weight loss slows or plateaus after initial success. Understanding how this medication works, why plateaus occur, and how to maintain long-term effectiveness is essential for realistic expectations and optimal outcomes. This article explores the mechanisms behind tirzepatide, the science of weight plateaus, strategies to sustain treatment benefits, and when to seek medical review.
Quick Answer: Tirzepatide does not stop working over time, but weight loss typically slows or plateaus due to metabolic adaptation, hormonal changes, and lifestyle factors rather than loss of drug effectiveness.
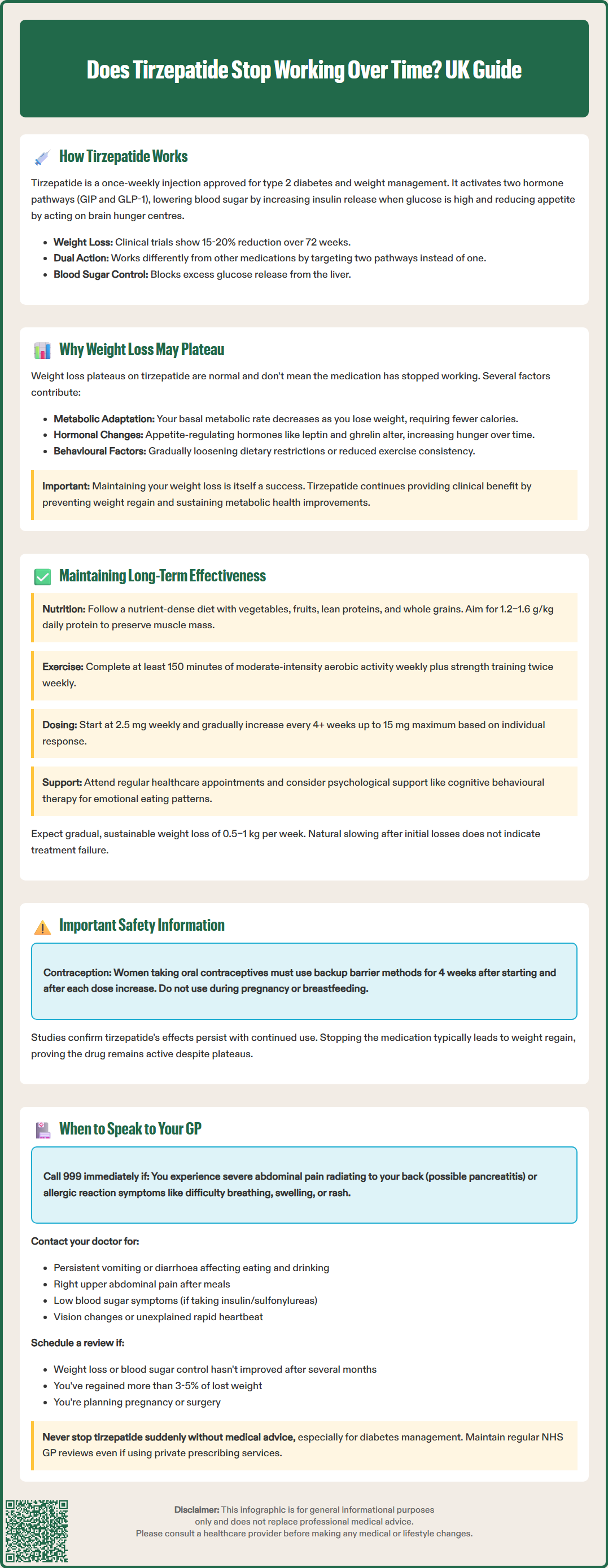
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK as Mounjaro for the treatment of type 2 diabetes mellitus and as Zepbound for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. It is administered as a once-weekly subcutaneous injection and works through multiple complementary mechanisms to improve glycaemic control and promote weight loss.
The medication enhances insulin secretion in a glucose-dependent manner, meaning it stimulates the pancreas to release insulin only when blood glucose levels are elevated, thereby reducing the risk of hypoglycaemia. Simultaneously, tirzepatide suppresses glucagon secretion, which helps prevent the liver from releasing excess glucose into the bloodstream. These actions work together to improve overall blood sugar regulation in people with type 2 diabetes. Tirzepatide is not indicated for type 1 diabetes.
For weight management, tirzepatide acts on appetite centres in the brain to reduce hunger and increase feelings of fullness (satiety). It also slows gastric emptying, though this particular effect may attenuate over time. Clinical trials, including the SURMOUNT and SURPASS programmes, have demonstrated significant weight loss that varies by dose and population—in the SURMOUNT-1 trial of non-diabetic adults, mean weight loss ranged from approximately 15% (5 mg dose) to 20% (15 mg dose) after 72 weeks. Weight loss tends to be lower in people with type 2 diabetes.
The dual receptor mechanism distinguishes tirzepatide from single GLP-1 receptor agonists. By activating both GIP and GLP-1 pathways, tirzepatide offers metabolic benefits, though individual responses vary. While improvements in cardiovascular risk factors such as blood pressure and lipid profiles have been observed, cardiovascular outcome benefits have not yet been established.
Important safety considerations include reduced exposure to oral contraceptives (requiring use of a barrier method for 4 weeks after initiation and each dose escalation) and avoidance during pregnancy and breastfeeding.

Mounjaro® is the most innovative GLP-1 medication proven to dramatically curb appetite, hunger, and cravings to help professional men achieve substantial weight loss.
Start Here
Wegovy® is a weekly injectable GLP-1 medication with proven effectiveness in reducing appetite, hunger, and cravings to help busy professionals lose significant weight.
Start HereMany patients using tirzepatide for weight management experience a plateau phase where weight loss slows or stabilises after an initial period of steady reduction. This phenomenon is well-recognised in obesity medicine and does not necessarily indicate that the medication has stopped working. Rather, it reflects normal physiological adaptations and the complex interplay of factors influencing body weight regulation.
As individuals lose weight, their basal metabolic rate typically decreases—the body requires fewer calories to maintain its new, lower weight. This metabolic adaptation is a natural survival mechanism but can make continued weight loss progressively more challenging. Additionally, hormonal changes occur during weight loss, including alterations in leptin, ghrelin, and other appetite-regulating hormones, which may increase hunger signals and reduce satiety over time.
Behavioural factors also play a crucial role in weight plateaus. Initial dietary changes and increased physical activity may become less stringent as treatment progresses. Portion sizes may gradually increase, or exercise routines may become less consistent. These subtle shifts can offset the appetite-suppressing effects of tirzepatide, leading to weight stabilisation rather than continued loss.
It is important to note that weight maintenance itself represents a therapeutic success. Research shows that without pharmacological intervention, most individuals regain lost weight within 1–2 years. If tirzepatide helps maintain a lower body weight—even without further reduction—it is still providing clinical benefit by preventing weight regain and sustaining improvements in metabolic health markers.
While the medication's core appetite-suppressing and metabolic effects generally persist with continued treatment, some specific effects—particularly delayed gastric emptying—do attenuate over time. Long-term studies such as SURMOUNT-4 demonstrate that continued tirzepatide treatment helps maintain weight loss, while discontinuation typically leads to weight regain, suggesting ongoing pharmacological activity. The overall plateau effect represents the balance between the drug's persistent effects and the body's compensatory mechanisms, alongside lifestyle factors that influence overall energy balance.
Optimising long-term outcomes with tirzepatide requires a comprehensive approach that combines pharmacotherapy with sustained lifestyle modifications. The medication is most effective when viewed as one component of a broader weight management or diabetes care strategy, rather than a standalone solution.
Dietary adherence remains fundamental throughout treatment. Working with a registered dietitian can help patients develop sustainable eating patterns that complement tirzepatide's appetite-suppressing effects. Focus should be on:
Nutrient-dense, whole foods including vegetables, fruits, lean proteins, and whole grains
Adequate protein intake (1.2–1.6 g/kg body weight per day) to preserve lean muscle mass during weight loss, though this should be individualised for those with renal impairment or frailty
Mindful eating practices to recognise true hunger and satiety signals
Regular meal patterns to maintain stable blood glucose levels
Physical activity is equally important for maintaining treatment effectiveness. The UK Chief Medical Officers' guidelines recommend adults aim for at least 150 minutes of moderate-intensity aerobic activity weekly, plus strength training twice weekly. Exercise helps preserve metabolic rate during weight loss, improves insulin sensitivity, and supports cardiovascular health. Importantly, physical activity should be gradually increased and tailored to individual capabilities and preferences to ensure long-term adherence.
Dose optimisation may be necessary for some patients. Tirzepatide is typically initiated at 2.5 mg weekly and gradually increased at minimum 4-week intervals through 5 mg, 7.5 mg, 10 mg, 12.5 mg to a maximum of 15 mg based on individual response and tolerability. If a dose is missed, it should be administered within 4 days of the scheduled dose, maintaining at least 3 days between injections; otherwise, skip until the next scheduled dose. If using tirzepatide alongside insulin or sulfonylureas, these doses may need reduction to prevent hypoglycaemia.
Regular monitoring through healthcare appointments allows for timely identification of plateaus and adjustment of the overall treatment plan. These consultations provide opportunities to review dietary habits, physical activity levels, medication adherence, and any barriers to success. Psychological support, including cognitive behavioural therapy for weight management, may benefit some patients by addressing emotional eating patterns or motivation challenges.
Patients should maintain realistic expectations about weight loss trajectories. Gradual, sustained weight loss of 0.5–1 kg per week is considered safe and sustainable. Rapid initial losses often slow naturally, and this does not indicate treatment failure.
Certain situations warrant prompt discussion with your GP or prescribing clinician to ensure safe and effective use of tirzepatide. Open communication about your treatment experience enables appropriate adjustments and helps identify any concerning developments early.
Seek immediate medical attention (call 999 or go to A&E) if you experience:
Signs of pancreatitis such as severe, persistent abdominal pain radiating to the back, often accompanied by nausea and vomiting
Signs of allergic reaction including rash, itching, swelling, difficulty breathing, or feeling faint
You should contact your healthcare provider if you experience:
Persistent or severe gastrointestinal symptoms including nausea, vomiting, diarrhoea, or abdominal pain that interferes with daily activities or prevents adequate nutrition and hydration
Symptoms of gallbladder disease including right upper abdominal pain, particularly after eating fatty meals
Hypoglycaemia symptoms (if taking tirzepatide alongside insulin or sulfonylureas) such as trembling, sweating, confusion, or palpitations
Changes in vision or eye problems, especially if you have diabetic retinopathy
Unexplained rapid heart rate or palpitations
Regarding treatment effectiveness, schedule a review appointment if:
Your weight loss or blood glucose control has not improved as expected after several months of treatment at the maximum tolerated dose
You experience significant weight regain (more than 3–5% of lost weight) despite maintaining lifestyle modifications
You are considering stopping treatment or have concerns about long-term use
You are planning pregnancy or become pregnant (tirzepatide should be discontinued)
You need to discuss contraception (reduced oral contraceptive effectiveness requires barrier method use for 4 weeks after starting and after each dose increase)
You have upcoming surgery or procedures requiring sedation (due to delayed gastric emptying effects)
Never discontinue tirzepatide abruptly without medical guidance, particularly if using it for diabetes management, as this may lead to deterioration in glycaemic control. Your GP can help determine whether treatment should continue, require modification, or transition to alternative therapies.
For patients using tirzepatide through private prescribing services, ensure you have regular NHS GP reviews to monitor overall health, cardiovascular risk factors, and any potential complications. Integrated care between private prescribers and NHS services optimises safety and treatment outcomes. Your GP can also provide referrals to specialist weight management services or diabetes teams if additional support is needed to achieve your health goals.
Report any suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk), which helps monitor the safety of medicines.
Weight loss slows due to metabolic adaptation (your body requires fewer calories at a lower weight), hormonal changes affecting appetite regulation, and potential relaxation of dietary or exercise habits. This plateau does not mean tirzepatide has stopped working—maintaining weight loss itself represents therapeutic success.
Long-term studies demonstrate that discontinuing tirzepatide typically leads to weight regain and, for those with diabetes, deterioration in blood glucose control. Never stop tirzepatide without medical guidance, particularly if using it for diabetes management.
Combine tirzepatide with sustained lifestyle modifications including nutrient-dense eating patterns, adequate protein intake, regular physical activity (at least 150 minutes weekly), and ongoing support from healthcare professionals. Dose optimisation and regular monitoring help ensure continued benefit.
All medical content on this blog is created based on reputable, evidence-based sources and reviewed regularly for accuracy and relevance. While we strive to keep content up to date with the latest research and clinical guidelines, it is intended for general informational purposes only.
DisclaimerThis content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional with any medical questions or concerns. Use of the information is at your own risk, and we are not responsible for any consequences resulting from its use.